Mild cognitive impairment US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mild cognitive impairment. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Mild cognitive impairment US Medical PG Question 1: A group of neurologists develop a new blood test for Alzheimer's. They are optimistic about the test, as they have found that for any given patient, the test repeatedly produces very similar results. However, they find that the new test results are not necessarily consistent with the gold standard of diagnosis. How would this new test most accurately be described?
- A. Valid and reliable
- B. Reliable (Correct Answer)
- C. Valid
- D. Biased
- E. Neither valid nor reliable
Mild cognitive impairment Explanation: ***Reliable***
- The test produces **similar results repeatedly** upon repeated measures, indicating high **reliability** or **precision**.
- Reliability refers to the **consistency** of a measure, even if it is not accurate.
*Valid and reliable*
- While the test is **reliable**, it is explicitly stated that the results are **not consistent with the gold standard**, meaning it lacks **validity**.
- A test must be both **consistent** (reliable) and **accurate** (valid) to be described as valid and reliable.
*Valid*
- **Validity** refers to the **accuracy** of a test, or how well it measures what it is supposed to measure.
- The test is explicitly stated to **not be consistent with the gold standard**, indicating a lack of agreement with the true measure of Alzheimer's.
*Biased*
- **Bias** refers to a **systematic error** in measurement that can lead to consistently high or low results compared to the true value.
- While the test might be biased due to its lack of consistency with the gold standard, "biased" is not the most accurate single descriptor of its measurement properties given the information provided.
*Neither valid nor reliable*
- The test is described as producing **very similar results repeatedly**, which directly indicates it has **high reliability**.
- Therefore, stating it is neither valid nor reliable is incorrect, as it possesses reliability.
Mild cognitive impairment US Medical PG Question 2: A 72-year-old man is brought to the physician by his wife for memory issues over the last 7 months. The patient's wife feels that he has gradually become more forgetful. He commonly misplaces his car keys and forgets his children's names. He seems to have forgotten how to make dinner and sometimes serves uncooked noodles or raw meat. One night he parked his car in a neighbor's bushes and was found wandering the street. He has a history of hypertension, hyperlipidemia, and COPD. Current medications include atorvastatin, metoprolol, ipratropium, and fluticasone. Vital signs are within normal limits. He is alert and oriented to person and place only. Neurologic examination shows no focal findings. His Mini-Mental State Examination score is 19/30. A complete blood count and serum concentrations of electrolytes, urea nitrogen, creatinine, thyroid-stimulating hormone, liver function tests, vitamin B12 (cobalamin), and folate are within the reference range. Which of the following is the most appropriate next step in diagnosis?
- A. Electroencephalography
- B. PET scan
- C. MRI of the brain (Correct Answer)
- D. Lumbar puncture
- E. Neuropsychologic testing
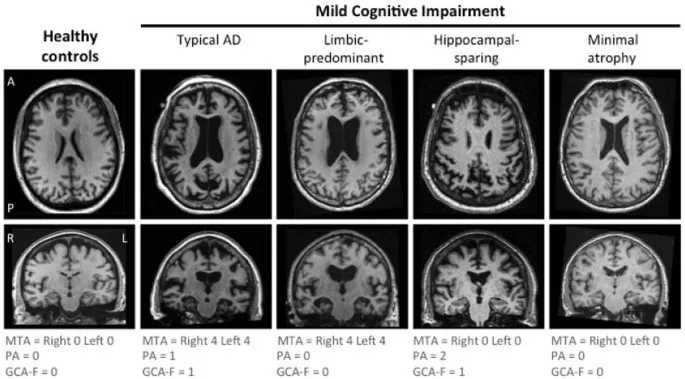
Mild cognitive impairment Explanation: ***MRI of the brain***
- An **MRI of the brain** is crucial for evaluating **structural causes of cognitive impairment**, such as tumors, strokes, hydrocephalus, or significant atrophy that might explain the patient's rapidly progressing memory loss and functional decline.
- Given the patient's age, rapidly worsening dementia symptoms, and normal initial lab work, imaging is essential to rule out **reversible or treatable causes** and to characterize the extent of neurodegeneration.
*Electroencephalography*
- **EEG** is primarily used to detect **seizure activity** or to evaluate for rapidly progressive encephalopathies like Creutzfeldt-Jakob disease, which is not indicated by the patient's presentation.
- The patient's symptoms are consistent with a dementia syndrome, not acute encephalopathy or seizures.
*PET scan*
- A **PET scan** (e.g., FDG-PET or amyloid-PET) can provide information about metabolic activity or amyloid plaques, useful for **differentiating types of dementia** (e.g., Alzheimer's disease).
- However, it is an advanced test typically considered after structural imaging has ruled out other causes and when the diagnosis remains unclear.
*Lumbar puncture*
- **Lumbar puncture** is performed to analyze **cerebrospinal fluid (CSF)** for biomarkers (e.g., tau, Aβ42 levels) to help diagnose specific neurodegenerative diseases like Alzheimer's or to rule out infectious/inflammatory causes.
- It's usually reserved for cases where other investigations are inconclusive or specific conditions are strongly suspected, and structural imaging has been performed.
*Neuropsychologic testing*
- **Neuropsychologic testing** provides a detailed assessment of various cognitive domains and can help to **characterize the pattern and severity of cognitive impairment**.
- While valuable, it is usually performed after initial medical workup and structural imaging to understand the functional impact of any identified brain changes or to further delineate the type of cognitive disorder.
Mild cognitive impairment US Medical PG Question 3: An 80-year-old woman is brought to the physician by her 2 daughters for worsening memory loss. They report that their mother is increasingly forgetful about recent conversations and events. She is unable to remember her appointments and commitments she has made. 3 years ago, the patient was moved into an elder care facility because she was often getting lost on her way home and forgetting to take her medications. The patient reports that she is very socially active at her new home and has long conversations with the other residents about her adventures as an air hostess during her youth. Which of the following cerebral pathologies is most likely present in this patient?
- A. Lewy bodies
- B. Lacunar infarcts
- C. Intracytoplasmic vacuoles
- D. Neurofibrillary tangles (Correct Answer)
- E. Demyelination
Mild cognitive impairment Explanation: ***Neurofibrillary tangles***
- The patient's presentation with **progressive memory loss** affecting recent events, getting lost, and forgetting medications, while largely preserving long-term memory (recalling youth as an air hostess and engaging in conversations), is highly characteristic of **Alzheimer's disease**.
- **Neurofibrillary tangles**, composed of hyperphosphorylated tau protein, along with **amyloid plaques**, are the hallmark pathological findings in Alzheimer's disease.
*Lewy bodies*
- **Lewy bodies** are characteristic of **Lewy body dementia** or Parkinson's disease with dementia, which typically present with prominent **fluctuations in cognition**, recurrent **visual hallucinations**, and parkinsonism.
- While memory loss can occur, the dominant features in this case point away from Lewy body pathology.
*Lacunar infarcts*
- **Lacunar infarcts** are associated with **vascular dementia**, which often presents with a more **step-wise decline** in cognitive function, focal neurological deficits, and evidence of cerebrovascular disease on imaging.
- The patient's gradual and progressive memory loss is less typical of lacunar infarcts as the primary cause.
*Intracytoplasmic vacuoles*
- **Intracytoplasmic vacuoles** are characteristic of **Creutzfeldt-Jakob disease** (spongiform encephalopathy), which is a rapidly progressive and fatal neurodegenerative disorder with distinct neurological symptoms such as myoclonus and ataxia, not fitting this patient's profile.
- The disease course is typically much faster than the 3-year progression described.
*Demyelination*
- **Demyelination** is the hallmark of conditions like **multiple sclerosis**, which primarily affects younger individuals and typically presents with a range of neurological deficits, including motor, sensory, and visual disturbances, that often relapse and remit.
- It does not typically present as a primary, progressive memory disorder in an 80-year-old in this manner.
Mild cognitive impairment US Medical PG Question 4: A 63-year-old woman is brought to the clinic by her husband with complaints of cognitive decline. The patient's husband says that she has had intermittent problems with her memory for the past few years. He says she has occasional 'bad days' where her memory deteriorates to the point where she cannot perform activities of daily living. She is also sometimes found conversing in an empty room and, when inquired, she confirms that she is talking to a friend. There have also been some recent falls. There is no history of fever, recent head trauma, loss of consciousness, or illicit drug use. Past medical history is significant for bronchial asthma and osteoarthritis, both managed medically. Her mother died due to metastatic breast cancer at age 71 and her father was diagnosed with Alzheimer's disease at age 65. The patient is afebrile and her vital signs are within normal limits. Physical examination reveals a tremor present in both her hands that attenuates with voluntary movement. Deep tendon reflexes are 2+ bilaterally. Romberg's sign is negative. She has a slow gait with a mild stooped posture. Her laboratory findings are significant for the following:
Hemoglobin 12.9 g/dL
White cell count 8,520/mm³
Platelets 295,000/mm³
Serum creatinine 1.0 mg/dL
Glucose 94 mg/dL
Sodium 141 mEq/L
Potassium 3.9 mEq/L
Calcium 92 mg/dL
Ferritin 125 ng/mL
Serum B12 305 ng/L
TSH 2.1 µU/mL
Ceruloplasmin 45 mg/dL
Which of the following is the most appropriate management for this patient?
- A. Escitalopram
- B. Penicillamine
- C. Haloperidol
- D. Ropinirole
- E. Rivastigmine (Correct Answer)
Mild cognitive impairment Explanation: ***Rivastigmine***
- The patient exhibits classic symptoms of **dementia with Lewy bodies (DLB)**, including cognitive fluctuations, visual hallucinations (conversing in an empty room), and parkinsonism (tremor, slow gait, stooped posture, and falls). **Cholinesterase inhibitors** like **rivastigmine** are the first-line treatment for cognitive and neuropsychiatric symptoms in DLB as they can help improve cognitive function and reduce hallucinations.
- While Parkinson's disease itself is not the primary diagnosis, the presence of **parkinsonian features** and cognitive decline with hallucinations makes DLB a strong consideration. Rivastigmine increases the availability of **acetylcholine** in the brain, improving cognitive function and behavioral symptoms in DLB.
*Escitalopram*
- **Escitalopram** is an **SSRI antidepressant** and would be appropriate if the patient's primary symptoms were **depression or anxiety**.
- While depression can coexist with dementia, the described symptoms of cognitive fluctuations, hallucinations, and parkinsonism are not primarily indicative of depression.
*Penicillamine*
- **Penicillamine** is a **chelating agent** used primarily in the treatment of **Wilson's disease**, which is characterized by copper accumulation.
- The patient's **ceruloplasmin levels are normal**, making Wilson's disease unlikely, and the clinical presentation does not align with typical Wilson's disease symptoms.
*Haloperidol*
- **Haloperidol** is a **first-generation antipsychotic** that could be used for severe behavioral disturbances or psychosis.
- However, in patients with **dementia with Lewy bodies (DLB)**, antipsychotics, particularly typical ones like haloperidol, can significantly worsen parkinsonian symptoms and cognitive function due to **extreme sensitivity to neuroleptics**.
*Ropinirole*
- **Ropinirole** is a **dopamine agonist** primarily used in the treatment of **Parkinson's disease** to manage motor symptoms.
- While the patient has parkinsonian features, the prominent cognitive fluctuations and visual hallucinations point more towards **Dementia with Lewy Bodies (DLB)**, where dopamine agonists can sometimes exacerbate hallucinations and other neuropsychiatric symptoms.
Mild cognitive impairment US Medical PG Question 5: A 69-year-old woman is brought to the physician by her daughter because of increasing forgetfulness and generalized fatigue over the past 4 months. She is unable to remember recent events and can no longer recognize familiar people. She lives independently, but her daughter has hired a helper in the past month since the patient has found it difficult to shop or drive by herself. She has stopped attending family functions and refuses to visit the neighborhood clubhouse, where she used to conduct game nights for the residents. She has had a 7-kg (15-lb) weight gain over this period. She is alert and oriented to time, place, and person. Her temperature is 36°C (97.6°F), pulse is 54/min, and blood pressure is 122/80 mm Hg. Mental status examination shows impaired attention and concentration; she has difficulty repeating seven digits forward and five in reverse sequence. She cannot recall any of the 3 objects shown to her after 10 minutes. She has no delusions or hallucinations. Further evaluation is most likely to show which of the following?
- A. Ventriculomegaly on CT scan of the head
- B. Elevated serum WBC count
- C. Decreased serum vitamin B12
- D. Elevated serum TSH (Correct Answer)
- E. Diffuse cortical atrophy on brain MRI
Mild cognitive impairment Explanation: ***Elevated serum TSH***
- The patient's symptoms, including **forgetfulness**, generalized **fatigue**, weight gain, and **bradycardia** (pulse 54/min), are highly suggestive of **hypothyroidism**.
- **Hypothyroidism** can present with cognitive dysfunction (often mistaken for dementia), depression-like symptoms (withdrawal from social activities), and metabolic changes like weight gain.
*Ventriculomegaly on CT scan of the head*
- **Ventriculomegaly** is often associated with conditions like **Normal Pressure Hydrocephalus (NPH)**, which presents with a triad of gait disturbance, urinary incontinence, and dementia.
- While cognitive impairment is present, the absence of gait issues and incontinence makes NPH less likely, and other symptoms point away from it.
*Elevated serum WBC count*
- An **elevated WBC count** indicates an **infection** or inflammatory process.
- The patient's symptoms are chronic (4 months), subacute, and lack specific signs of infection such as fever (temperature is normal) or acute inflammation.
*Decreased serum vitamin B12*
- **Vitamin B12 deficiency** can cause cognitive impairment, fatigue, and neurological symptoms.
- However, it is typically associated with **anemia** and/or peripheral neuropathy, which are not mentioned in this patient's presentation.
*Diffuse cortical atrophy on brain MRI*
- **Diffuse cortical atrophy** is a common finding in various forms of **dementia**, such as **Alzheimer's disease**.
- While it's a possibility, other more treatable causes of cognitive decline, like hypothyroidism, should be investigated first given the constellation of symptoms.
Mild cognitive impairment US Medical PG Question 6: A 82-year-old woman is brought to the physician by her son because he is concerned about her forgetfulness for the past 2 years. She occasionally walks into a room and forgets why she went there and often forgets where she left her keys. She is sometimes unable to recall a familiar individual's name. She reports that she has become slower at completing sudoku puzzles. She has been living independently since the death of her husband 3 years ago. She goes shopping, cooks her own meals, and plays bridge with her friends every weekend. She is not anxious about her memory lapses. She has no trouble sleeping but has been getting up earlier than she used to. She has hypertension that is managed with hydrochlorothiazide. She appears healthy. Vital signs are within normal limits. She is oriented to person, place, and time. Examination shows a normal gait. She describes her mood as “good” and her speech is normal. Her thought process is organized and her judgement is intact. She makes one error when performing serial sevens. The remainder of the examination shows no abnormalities. Which of the following is the most likely cause of this patient's symptoms?
- A. Alzheimer's disease
- B. Normal pressure hydrocephalus
- C. Vascular dementia
- D. Lewy-body dementia
- E. Aging (Correct Answer)
Mild cognitive impairment Explanation: ***Aging***
- The patient exhibits mild, age-associated cognitive changes such as occasional forgetfulness and slower cognitive processing (sudoku puzzles), without significant functional impairment in daily activities. This aligns with **normal cognitive aging**.
- Her ability to live independently, manage finances, perform household tasks, and engage in social activities (playing bridge) indicates that these memory lapses do not meet the criteria for a dementia syndrome.
*Alzheimer's disease*
- Alzheimer's disease typically presents with more pervasive and progressive memory loss, significantly impacting daily activities and **instrumental activities of daily living (IADLs)**, which are preserved in this patient.
- While forgetfulness is present, it's not severe enough to suggest the **pathological changes** characteristic of Alzheimer's, such as marked impairment in multiple cognitive domains and functional decline.
*Normal pressure hydrocephalus*
- This condition is characterized by the classic triad of **gait disturbance**, **urinary incontinence**, and **dementia (cognitive impairment)**.
- The patient has no issues with gait or urinary incontinence, and her cognitive symptoms are mild and do not constitute dementia.
*Vascular Dementia*
- Vascular dementia is usually associated with a history of **strokes** or significant **vascular risk factors** leading to step-wise cognitive decline.
- The patient's hypertension is managed, and there is no evidence of focal neurological deficits, stroke history, or a fluctuating course often seen in vascular dementia.
*Lewy-body dementia*
- Key features of Lewy body dementia include **fluctuating cognition**, **recurrent visual hallucinations**, and **spontaneous parkinsonism**.
- None of these defining symptoms are present in the patient's presentation; her mood is good, and her gait is normal.
Mild cognitive impairment US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Mild cognitive impairment Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Mild cognitive impairment US Medical PG Question 8: A 78-year-old man is brought to the physician by his daughter for a follow-up examination. The daughter noticed that he has gradually become more forgetful and withdrawn over the last year. He frequently misplaces his car keys and forgets the names of his neighbors, whom he has known for 30 years. He has difficulty recalling his address and telephone number. He recently had an episode of urinary and fecal incontinence. Last week, his neighbor found him wandering the parking lot of the grocery store. He has hypertension and hyperlipidemia. He had smoked one pack of cigarettes daily for 40 years but quit 18 years ago. His current medications include hydrochlorothiazide and atorvastatin. He appears healthy; BMI is 23 kg/m2. His temperature is 37.2°C (99.0°F), pulse is 86/min, respirations are 14/min, and blood pressure is 136/84 mm Hg. Mini-mental state examination score is 19/30. He is not bothered by his forgetfulness. Cranial nerves II–XII are intact. He has 5/5 strength and full sensation to light touch in all extremities. His patellar, Achilles, and biceps reflexes are 2+ bilaterally. His gait is steady. MRI scan of the brain shows ventriculomegaly and prominent cerebral sulci. Which of the following is the most appropriate pharmacotherapy?
- A. Acetazolamide
- B. Sertraline
- C. Memantine
- D. Thiamine
- E. Donepezil (Correct Answer)
Mild cognitive impairment Explanation: ***Donepezil***
- The patient exhibits features consistent with **Alzheimer's disease**, including gradual memory loss, difficulty with daily tasks, episodes of incontinence, and a Mini-Mental State Examination (MMSE) score of 19/30. Donepezil, a **cholinesterase inhibitor**, is a first-line treatment for mild to moderate Alzheimer's to slow cognitive decline.
- The MRI findings of **ventriculomegaly and prominent cerebral sulci** are consistent with general cerebral atrophy often seen in Alzheimer's disease, not hydrocephalus requiring shunting or other specific brain pathologies (normal pressure hydrocephalus would have gait disturbance as a prominent feature, which is absent here).
*Acetazolamide*
- **Acetazolamide** is a **carbonic anhydrase inhibitor** used to treat conditions like glaucoma, altitude sickness, and idiopathic intracranial hypertension.
- There is no indication of elevated intracranial pressure or hydrocephalus that would warrant the use of acetazolamide in this patient.
*Sertraline*
- **Sertraline** is a **selective serotonin reuptake inhibitor (SSRI)** primarily used to treat depression, anxiety disorders, and obsessive-compulsive disorder.
- While depression can coexist with dementia, the primary cognitive symptoms described here are not primarily depressive; therefore, an antidepressant is not the most appropriate initial pharmacotherapy for cognitive decline.
*Memantine*
- **Memantine** is an **NMDA receptor antagonist** used in moderate to severe Alzheimer's disease, often in combination with cholinesterase inhibitors or when cholinesterase inhibitors are not tolerated.
- While appropriate for moderate to severe Alzheimer's, **cholinesterase inhibitors** are typically the initial treatment for mild to moderate stages, and the patient's MMSE score of 19/30 often falls into the mild-moderate category where donepezil is usually favored first.
*Thiamine*
- **Thiamine** (vitamin B1) supplementation is primarily used to treat **Wernicke-Korsakoff syndrome**, which is associated with chronic alcohol abuse and presents with ataxia, ophthalmoplegia, and confusion, none of which are the primary presenting symptoms here.
- There is no evidence of **nutritional deficiency** or alcohol abuse in this patient to suggest thiamine deficiency as the cause of his cognitive decline.
Mild cognitive impairment US Medical PG Question 9: A 68-year-old man seeks evaluation by a physician with complaints of worsening forgetfulness and confusion for 1 year. According to his wife, he has always been in good health and is generally very happy; however, he has started to forget important things. He recently had his driving license revoked because of multiple tickets, but he cannot recall having done anything wrong. This morning, he neglected to put on his socks and was quite agitated when she pointed this out to him. He denies having a depressed mood, sleep problems, or loss of interest. He occasionally has a glass of wine with dinner and has never smoked or used recreational drugs. His medical history and family medical history are unremarkable. His pulse is 68/min, respirations are 14/min, and blood pressure is 130/84 mm Hg. Except for a mini-mental state examination (MMSE) score of 20/30, the remainder of the physical examination is unremarkable. Imaging studies, including a chest X-ray and CT of the brain, reveal no pathologic findings. An electrocardiogram (ECG) is also normal. Laboratory testing showed the following:
Serum glucose (fasting) 76 mg/dL
Serum electrolytes:
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Serum creatinine 0.9 mg/dL
Blood urea nitrogen 11 mg/dL
Cholesterol, total: 180 mg/dL
HDL-cholesterol 45 mg/dL
LDL-cholesterol 75 mg/dL
Triglycerides 135 mg/dL
Hemoglobin (Hb%) 16 g/dL
Mean corpuscular volume (MCV) 85 fL
Reticulocyte count 0.9%
Erythrocyte count 5 million/mm³
Thyroid-stimulating hormone 3.5 µU/mL
Urinalysis
Glucose Negative
Ketones Negative
Leucocytes Negative
Nitrite Negative
RBCs Negative
Casts Negative
Which of the following is the most likely diagnosis?
- A. Alzheimer’s dementia (Correct Answer)
- B. Creutzfeldt-Jakob disease
- C. Lewy body dementia
- D. Parkinson’s disease
- E. Vascular dementia
Mild cognitive impairment Explanation: ***Alzheimer’s dementia***
- The patient presents with **progressive memory loss** and **confusion** that has worsened over a year, along with **agitational behavior** and difficulty with daily tasks (neglecting to put on socks), which are classic symptoms of Alzheimer's dementia.
- The **MMSE score of 20/30** indicates cognitive impairment, and the absence of other neurological findings or clear vascular risk factors supports this diagnosis.
*Creutzfeldt-Jakob disease*
- This is a rare, rapidly progressive, and fatal neurodegenerative disease that typically presents with **rapidly progressive dementia**, **myoclonus**, and other neurological signs, which are not described in this case.
- The patient's symptoms have progressed over a year, which is not as rapid as the typical course of CJD.
*Lewy body dementia*
- Characterized by **fluctuating cognition**, **recurrent visual hallucinations**, and **spontaneous parkinsonism**, which are not reported in this patient.
- While agitation can occur, the core features of Lewy body dementia are absent.
*Parkinson’s disease*
- Primarily a **movement disorder** characterized by **bradykinesia**, **rigidity**, **tremor**, and **postural instability**. While dementia can occur in later stages (Parkinson's disease dementia), the initial presentation in this patient is predominantly cognitive decline without prominent motor symptoms.
- The patient's physical examination is "unremarkable," suggesting an absence of parkinsonian motor signs.
*Vascular dementia*
- Typically associated with a history of **stroke** or significant **vascular risk factors** (e.g., uncontrolled hypertension, diabetes) and often presents with a **step-wise decline** in cognitive function.
- This patient has a largely unremarkable medical history, controlled blood pressure, and normal cholesterol, and a CT scan showed no pathological findings (e.g., infarcts), making vascular dementia less likely.
Mild cognitive impairment US Medical PG Question 10: A patient with second-degree cervical prolapse complains of dribbling of urine when coughing. What is the most likely diagnosis?
- A. Cystitis
- B. Stress incontinence (Correct Answer)
- C. Overflow incontinence
- D. Functional incontinence
Mild cognitive impairment Explanation: ***Stress incontinence***
- **Stress incontinence** is characterized by involuntary urine leakage due to increased intra-abdominal pressure (e.g., coughing, sneezing), which is common in association with **pelvic organ prolapse** like a second-degree cervical prolapse.
- The prolapse weakens the **pelvic floor muscles** and supporting structures around the urethra, diminishing its ability to maintain closure during sudden pressure changes.
*Cystitis*
- **Cystitis** is an inflammation of the bladder, typically presenting with symptoms like painful urination (dysuria), frequent urination, and urgency.
- While it can cause bladder irritation, it does not directly lead to urine dribbling with coughing in the absence of other typical infection symptoms.
*Overflow incontinence*
- **Overflow incontinence** occurs due to an **overfilled bladder** that can't empty completely, leading to constant dribbling or leakage.
- This typically results from a **bladder outlet obstruction** or an **underactive detrusor muscle**, not directly from increased abdominal pressure during coughing.
*Functional incontinence*
- **Functional incontinence** is when a person has control over their bladder but cannot reach the toilet in time due to **physical or cognitive impairments**.
- It does not involve a problem with the urinary tract itself but rather with the ability to respond to the urge to urinate.
More Mild cognitive impairment US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.