Frontotemporal dementia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Frontotemporal dementia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
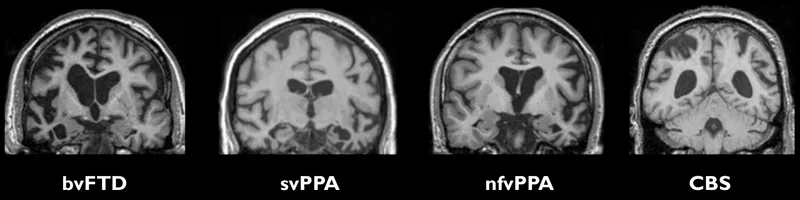
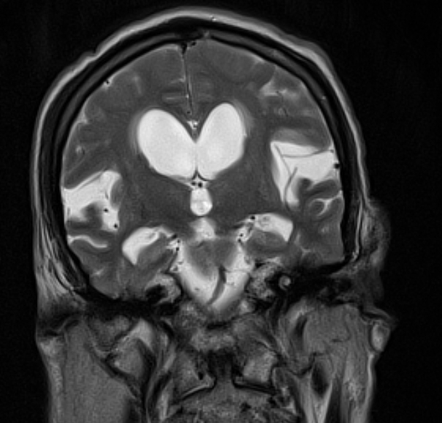
Frontotemporal dementia US Medical PG Question 1: A 73-year-old man is brought in by his wife with a history of progressive personality changes. The patient’s wife says that, over the past 3 years, he has become increasingly aggressive and easily agitated, which is extremely out of character for him. His wife also says that he has had several episodes of urinary incontinence in the past month. He has no significant past medical history. The patient denies any history of smoking, alcohol use, or recreational drug use. The patient is afebrile, and his vital signs are within normal limits. A physical examination is unremarkable. The patient takes the mini-mental status examination (MMSE) and scores 28/30. A T2 magnetic resonance image (MRI) of the head is performed and the results are shown in the exhibit (see image). Which of the following is the next best diagnostic step in the management of this patient?
- A. Contrast MRI of the head
- B. Lumbar puncture (Correct Answer)
- C. Noncontrast CT of the head
- D. Brain biopsy
- E. Serum ceruloplasmin level
Frontotemporal dementia Explanation: ***Lumbar puncture***
- The MRI shows **ventriculomegaly** with **transependymal CSF flow**, indicating **normal pressure hydrocephalus (NPH)**. A high-volume lumbar puncture serves as both a diagnostic and therapeutic test for NPH, as improvement in symptoms after CSF removal (typically 30-50 mL) strongly supports the diagnosis.
- This patient presents with **progressive cognitive decline** (personality changes, aggression, agitation) and **urinary incontinence**, two components of the classic NPH triad. While gait disturbance is the third component and most common presenting feature, NPH can present with incomplete triads, and the imaging findings strongly support this diagnosis.
*Contrast MRI of the head*
- Contrast-enhanced MRI is used to visualize specific lesions such as **tumors, infections, or inflammatory processes**, which are not suggested by this patient's presentation.
- The T2 MRI has already demonstrated findings consistent with NPH (ventriculomegaly with transependymal flow), making additional contrast imaging unnecessary for diagnosis at this stage.
*Noncontrast CT of the head*
- While noncontrast CT can demonstrate ventriculomegaly, **MRI provides superior resolution** for evaluating brain parenchyma and detecting **transependymal CSF flow**, a key indicator of NPH.
- Since MRI has already been performed and revealed findings diagnostic of NPH, repeating imaging with a less detailed modality would not add diagnostic value.
*Brain biopsy*
- Brain biopsy is an **invasive procedure** reserved for cases where **neoplastic, infectious, or demyelinating** conditions are strongly suspected and cannot be diagnosed by less invasive means.
- There is no indication of a mass lesion, infection, or focal abnormality requiring tissue diagnosis in this patient's clinical presentation or imaging findings.
*Serum ceruloplasmin level*
- Serum ceruloplasmin is used to diagnose **Wilson's disease**, a rare genetic disorder of copper metabolism presenting with neuropsychiatric symptoms and movement disorders, typically in patients **under 40 years of age**.
- Given this patient's age (73 years) and clear radiological evidence of NPH, Wilson's disease is not a consideration in the differential diagnosis.
Frontotemporal dementia US Medical PG Question 2: A 61-year-old woman presents to her primary care doctor with her son who reports that his mother is not acting like herself. She has gotten lost while driving several times in the past 2 months and appears to be talking to herself frequently. Of note, the patient’s husband died from a stroke 4 months ago. The patient reports feeling sad and guilty for causing so much trouble for her son. Her appetite has decreased since her husband died. On examination, she is oriented to person, place, and time. She is inattentive, and her speech is disorganized. She shakes her hand throughout the exam without realizing it. Her gait is slow and appears unstable. This patient’s condition would most likely benefit from which of the following medications?
- A. Bromocriptine
- B. Rivastigmine (Correct Answer)
- C. Reserpine
- D. Selegiline
- E. Levodopa
Frontotemporal dementia Explanation: ***Rivastigmine***
- The patient's symptoms of progressive cognitive decline (getting lost while driving, talking to herself), inattention, disorganized speech, and motor symptoms (hand tremor, unstable gait) suggest **Dementia with Lewy Bodies (DLB)**.
- Key features supporting DLB over depression with pseudodementia: **involuntary hand tremor**, **unstable gait**, **visual hallucinations** (talking to herself), and **disorganized speech** occurring with cognitive decline.
- **Rivastigmine**, a cholinesterase inhibitor, is a first-line treatment for the cognitive and behavioral symptoms in DLB and is FDA-approved for this indication.
- While bereavement-related depression is present, the prominent motor and cognitive features indicate an underlying neurodegenerative process.
*Bromocriptine*
- This is a **dopamine agonist** typically used for Parkinson's disease, hyperprolactinemia, and acromegaly.
- While Parkinsonian features are present in DLB, dopamine agonists can worsen **psychotic symptoms** (hallucinations) common in DLB, making them unsuitable as first-line treatment.
*Reserpine*
- **Reserpine** depletes catecholamines and serotonin and is primarily used as an antihypertensive.
- Its use in dementia is not indicated and could exacerbate mood, cognitive issues, and Parkinsonian symptoms due to its dopamine-depleting effects.
- This medication is rarely used in modern practice.
*Selegiline*
- **Selegiline** is a **monoamine oxidase-B (MAO-B) inhibitor** used in Parkinson's disease to reduce dopamine breakdown.
- While it may help with motor symptoms, its benefit in DLB is less established compared to cholinesterase inhibitors.
- The prominent **cognitive and behavioral symptoms** in this patient make cholinesterase inhibition the priority.
*Levodopa*
- **Levodopa** is a dopamine precursor and the most effective medication for motor symptoms of Parkinson's disease.
- In DLB, while it can improve motor symptoms, it can significantly worsen **psychotic symptoms** (hallucinations, delusions) and cognitive fluctuations.
- Given the prominent non-motor symptoms and existing hallucinations, levodopa is not first-line therapy for this patient.
Frontotemporal dementia US Medical PG Question 3: A 63-year-old woman is brought to the clinic by her husband with complaints of cognitive decline. The patient's husband says that she has had intermittent problems with her memory for the past few years. He says she has occasional 'bad days' where her memory deteriorates to the point where she cannot perform activities of daily living. She is also sometimes found conversing in an empty room and, when inquired, she confirms that she is talking to a friend. There have also been some recent falls. There is no history of fever, recent head trauma, loss of consciousness, or illicit drug use. Past medical history is significant for bronchial asthma and osteoarthritis, both managed medically. Her mother died due to metastatic breast cancer at age 71 and her father was diagnosed with Alzheimer's disease at age 65. The patient is afebrile and her vital signs are within normal limits. Physical examination reveals a tremor present in both her hands that attenuates with voluntary movement. Deep tendon reflexes are 2+ bilaterally. Romberg's sign is negative. She has a slow gait with a mild stooped posture. Her laboratory findings are significant for the following:
Hemoglobin 12.9 g/dL
White cell count 8,520/mm³
Platelets 295,000/mm³
Serum creatinine 1.0 mg/dL
Glucose 94 mg/dL
Sodium 141 mEq/L
Potassium 3.9 mEq/L
Calcium 92 mg/dL
Ferritin 125 ng/mL
Serum B12 305 ng/L
TSH 2.1 µU/mL
Ceruloplasmin 45 mg/dL
Which of the following is the most appropriate management for this patient?
- A. Escitalopram
- B. Penicillamine
- C. Haloperidol
- D. Ropinirole
- E. Rivastigmine (Correct Answer)
Frontotemporal dementia Explanation: ***Rivastigmine***
- The patient exhibits classic symptoms of **dementia with Lewy bodies (DLB)**, including cognitive fluctuations, visual hallucinations (conversing in an empty room), and parkinsonism (tremor, slow gait, stooped posture, and falls). **Cholinesterase inhibitors** like **rivastigmine** are the first-line treatment for cognitive and neuropsychiatric symptoms in DLB as they can help improve cognitive function and reduce hallucinations.
- While Parkinson's disease itself is not the primary diagnosis, the presence of **parkinsonian features** and cognitive decline with hallucinations makes DLB a strong consideration. Rivastigmine increases the availability of **acetylcholine** in the brain, improving cognitive function and behavioral symptoms in DLB.
*Escitalopram*
- **Escitalopram** is an **SSRI antidepressant** and would be appropriate if the patient's primary symptoms were **depression or anxiety**.
- While depression can coexist with dementia, the described symptoms of cognitive fluctuations, hallucinations, and parkinsonism are not primarily indicative of depression.
*Penicillamine*
- **Penicillamine** is a **chelating agent** used primarily in the treatment of **Wilson's disease**, which is characterized by copper accumulation.
- The patient's **ceruloplasmin levels are normal**, making Wilson's disease unlikely, and the clinical presentation does not align with typical Wilson's disease symptoms.
*Haloperidol*
- **Haloperidol** is a **first-generation antipsychotic** that could be used for severe behavioral disturbances or psychosis.
- However, in patients with **dementia with Lewy bodies (DLB)**, antipsychotics, particularly typical ones like haloperidol, can significantly worsen parkinsonian symptoms and cognitive function due to **extreme sensitivity to neuroleptics**.
*Ropinirole*
- **Ropinirole** is a **dopamine agonist** primarily used in the treatment of **Parkinson's disease** to manage motor symptoms.
- While the patient has parkinsonian features, the prominent cognitive fluctuations and visual hallucinations point more towards **Dementia with Lewy Bodies (DLB)**, where dopamine agonists can sometimes exacerbate hallucinations and other neuropsychiatric symptoms.
Frontotemporal dementia US Medical PG Question 4: A 55-year-old man is brought to the physician because of inappropriate behavior for the past 6 months. He has been making inappropriate comments and jokes while talking to friends and family members. He was arrested 3 weeks ago while trying to kiss strangers on the street. He has no interest in talking to his daughter or playing with his grandchildren. During this period, he has developed a strong desire for chocolate pudding and potato chips and has gained 10 kg (22 lb). He appears unkempt. Vital signs are within normal limits. Physical examination is unremarkable. Mental status examination shows apathy and a blunt affect. He avoids answering questions and instead comments on the individuals he saw in the waiting room. Mini-Mental State Examination score is 28/30. A complete blood count and serum concentrations of glucose, creatinine, and electrolytes are within the reference range. Which of the following is the most likely diagnosis?
- A. Parkinson disease
- B. Normal pressure hydrocephalus
- C. Amyotrophic lateral sclerosis
- D. Wilson disease
- E. Frontotemporal dementia (Correct Answer)
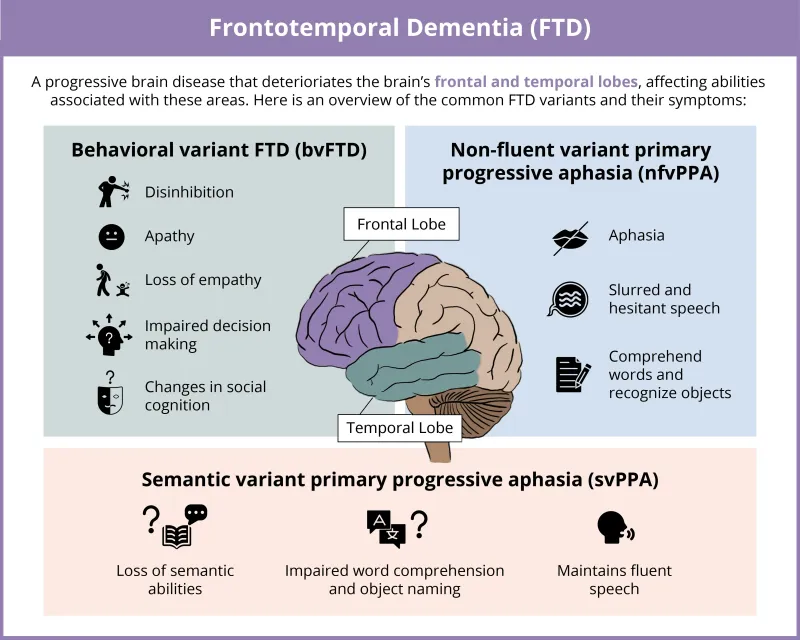
Frontotemporal dementia Explanation: ***Frontotemporal dementia***
- This patient's presentation with **inappropriate behavior**, **disinhibition**, **apathy**, **dietary changes** (sweet cravings, weight gain), and **lack of insight** are classic features of the **behavioral variant of frontotemporal dementia (bvFTD)**.
- The **Mini-Mental State Examination (MMSE) score of 28/30** indicates relatively preserved memory and visuospatial skills, which is typical in early bvFTD as cognitive deficits often appear later.
*Parkinson disease*
- While Parkinson's can present with **cognitive and behavioral changes** in later stages (Parkinson's disease dementia), the *initial* presentation is typically dominated by **motor symptoms** such as **bradykinesia, tremor, and rigidity**, which are absent here.
- The prominent behavioral disinhibition and early dietary changes are less characteristic of Parkinson's disease.
*Normal pressure hydrocephalus*
- Characterized by the classic triad of **gait disturbance**, **urinary incontinence**, and **dementia (subcortical)**.
- While some behavioral changes can occur, the prominent disinhibition, hyperorality, and specific dietary cravings seen here are not typical primary symptoms.
*Amyotrophic lateral sclerosis*
- This is a **motor neuron disease** characterized by progressive **muscle weakness, atrophy, and fasciculations**, affecting both upper and lower motor neurons.
- While approximately 15% of ALS patients can develop FTD, the primary presentation is invariably motor, and there are no motor symptoms described in this patient.
*Wilson disease*
- A **rare genetic disorder** leading to **copper accumulation**, affecting the **liver** and **brain**.
- Presents with a combination of **hepatic symptoms** (e.g., cirrhosis), **neurological symptoms** (e.g., tremor, dystonia, dysarthria), and **psychiatric symptoms** (e.g., depression, psychosis), often with **Kayser-Fleischer rings** in the cornea. The patient has none of these characteristic findings.
Frontotemporal dementia US Medical PG Question 5: A 59-year-old man is brought to the physician by his wife for a psychiatric evaluation. Over the past 12 months, his behavior has become increasingly disruptive. His wife no longer brings him along shopping because he has attempted to grope a female cashier on 2 occasions. He has begun to address the mail carrier using a racial epithet. Three years later, the patient dies. Light microscopy of sections of the frontal and temporal lobes shows intracellular inclusions of transactive response DNA binding protein (TDP-43). These proteins are bound to a regulatory molecule that usually marks them for degradation. The regulatory molecule in question is most likely which of the following?
- A. Kinesin
- B. Chaperone
- C. Cyclin
- D. Ubiquitin (Correct Answer)
- E. Clathrin
Frontotemporal dementia Explanation: ***Ubiquitin***
- **Ubiquitin** is a small regulatory protein that marks other proteins for degradation, typically by the **proteasome**. In neurodegenerative diseases like **frontotemporal dementia (FTD)**, aggregates of misfolded proteins, such as **TDP-43**, can accumulate when the ubiquitin-proteasome system is overwhelmed or dysfunctional.
- The patient's clinical presentation of **behavioral changes** (disruptive, inappropriate, racial epithets) and the pathological finding of **TDP-43 inclusions** in the frontal and temporal lobes are highly characteristic of **FTD**. The accumulation of TDP-43, despite being marked for degradation, points to a failure of the normal ubiquitin-mediated protein disposal pathway.
*Kinesin*
- **Kinesin** is a motor protein that facilitates **anterograde axonal transport**, moving cargo away from the cell body along microtubules.
- While important for neuronal function, kinesin is not directly involved in marking proteins for degradation.
*Chaperone*
- **Chaperones** are proteins that assist in the proper **folding of other proteins** and can help refold misfolded proteins, preventing aggregation.
- While chaperones play a role in protein quality control, they do not directly mark proteins for degradation in the same way as ubiquitin.
*Cyclin*
- **Cyclins** are a family of proteins that regulate the progression of cells through the **cell cycle** by activating cyclin-dependent kinases (CDKs).
- They are primarily involved in cell division and growth, not protein degradation pathways.
*Clathrin*
- **Clathrin** is a protein that plays a key role in the formation of **coated vesicles** involved in endocytosis and intracellular trafficking.
- It is crucial for forming vesicles that transport cargo, but it is not directly involved in marking proteins for degradation.
Frontotemporal dementia US Medical PG Question 6: An 81-year-old woman presents to your office accompanied by her husband. She has been doing well except for occasional word finding difficulty. Her husband is concerned that her memory is worsening over the past year. Recently, she got lost twice on her way home from her daughter’s house, was unable to remember her neighbor’s name, and could not pay the bills like she usually did. She has a history of hypertension and arthritis. She has no significant family history. Her medications include a daily multivitamin, hydrochlorothiazide, and ibuprofen as needed. Physical exam is unremarkable. Which of the following is associated with an increased risk of this patient’s disease?
- A. Presenilin-2
- B. ApoE2
- C. ApoE4 (Correct Answer)
- D. Female gender
- E. Advanced age (>85 years)
Frontotemporal dementia Explanation: ***Correct: ApoE4***
- The patient's symptoms (progressive memory loss, getting lost on familiar routes, difficulty with routine tasks like paying bills) in an 81-year-old suggest **Alzheimer's disease**.
- The **ApoE4 allele** is a well-established genetic risk factor for **late-onset Alzheimer's disease**, significantly increasing the likelihood (3-fold increased risk for one allele, 12-fold for two alleles) and often lowering the age of onset.
- ApoE4 is the **most specific and discriminating risk factor** among the options provided.
*Incorrect: Presenilin-2*
- **Presenilin-2** mutations are associated with **early-onset familial Alzheimer's disease**, which typically manifests before age 65 and often has a strong family history.
- This patient is 81 years old and has no significant family history, making early-onset familial AD unlikely.
*Incorrect: ApoE2*
- The **ApoE2 allele** is actually associated with a **decreased risk** of Alzheimer's disease.
- It is thought to be protective due to its more efficient clearance of amyloid beta peptides from the brain.
*Incorrect: Female gender*
- While **female gender** is indeed a risk factor for Alzheimer's disease (women have approximately 2:1 higher lifetime risk even after adjusting for longevity), it is less specific than ApoE4 as a discriminating answer.
- All patients have a biological sex, but only some carry the ApoE4 allele, making ApoE4 a more useful clinical and epidemiological marker.
*Incorrect: Advanced age (>85 years)*
- **Advanced age** is actually the strongest non-modifiable risk factor for Alzheimer's disease, with incidence doubling every 5 years after age 65.
- However, in the context of this question, **ApoE4 is the better answer** because it represents a specific genetic risk factor that can be tested and is directly associated with disease pathogenesis, whereas advanced age is a universal demographic factor that applies to all individuals who live long enough.
Frontotemporal dementia US Medical PG Question 7: A 72-year-old woman is brought to the physician by her son for an evaluation of cognitive decline. Her son reports that she has had increased difficulty finding her way back home for the last several months, despite having lived in the same city for 40 years. He also reports that his mother has been unable to recall the names of her relatives and been increasingly forgetting important family gatherings such as her grandchildren's birthdays over the last few years. The patient has hypertension and type 2 diabetes mellitus. She does not smoke or drink alcohol. Her current medications include enalapril and metformin. Her temperature is 37°C (98.6°F), pulse is 70/min, and blood pressure is 140/80 mm Hg. She is confused and oriented only to person and place. She recalls 2 out of 3 words immediately and 1 out of 3 after 5 minutes. Her gait and muscle strength are normal. Deep tendon reflexes are 2+ bilaterally. The remainder of the examination shows no abnormalities. Further evaluation is most likely to reveal which of the following findings?
- A. Generalized cerebral atrophy (Correct Answer)
- B. Myoclonic movements
- C. Hallucinations
- D. Urinary incontinence
- E. Resting tremor
Frontotemporal dementia Explanation: ***Generalized cerebral atrophy***
- The patient's symptoms of progressive **cognitive decline**, including difficulty with navigation and memory, are classic signs of **Alzheimer's disease**.
- **Generalized cerebral atrophy**, particularly of the **hippocampus** and **temporal lobes**, is a hallmark pathological finding in Alzheimer's disease due to neuronal loss and synaptic dysfunction.
*Myoclonic movements*
- **Myoclonic movements** are sudden, brief, involuntary muscle jerks, most commonly associated with **Creutzfeldt-Jakob disease** or certain types of dementia with Lewy bodies, which are not suggested by the patient's presentation.
- While some rare forms of early-onset Alzheimer's can have atypical features, myoclonus is not a typical or early finding in the more common late-onset presentation described.
*Hallucinations*
- **Hallucinations**, particularly visual hallucinations, are frequently seen in **dementia with Lewy bodies** and **Parkinson's disease dementia**, often preceding or co-occurring with cognitive decline.
- While hallucinations can occur in late-stage Alzheimer's, they are not a prominent or early feature differentiating it from other dementias.
*Urinary incontinence*
- **Urinary incontinence** can be a symptom of various conditions, including **normal pressure hydrocephalus (NPH)**, which presents with a triad of gait instability, dementia, and urinary incontinence.
- In Alzheimer's disease, incontinence typically appears in the **later stages**, after significant cognitive impairment and functional decline have occurred.
*Resting tremor*
- A **resting tremor** is a characteristic symptom of **Parkinson's disease** and is often seen in **Parkinson's disease dementia** or **dementia with Lewy bodies**.
- The patient's neurological examination, including normal gait and muscle strength, does not suggest Parkinsonian features.
Frontotemporal dementia US Medical PG Question 8: A 53-year-old man is brought to the clinic by his son for the evaluation of unusual behavior. He is a shopkeeper by profession and sometimes behaves very rudely to the customers. Recently, he accused one of the customers of using black magic over his shop. He has been increasingly irritable, forgetting things, and having problems managing his finances over the past 8 months. He is also having difficulty finding words and recalling the names of objects during the conversation. There is no history of recent head trauma, fever, hallucinations, or abnormal limb movements. Past medical history is significant for a well-controlled type 2 diabetes mellitus. Family history is unremarkable. He does not smoke or use illicit drugs. Vital signs are stable with a blood pressure of 134/76 mm Hg, a heart rate of 88/min, and a temperature of 37.0°C (98.6°F). On physical examination, he has problems naming objects and planning tasks. Mini-mental state examination (MMSE) score is 26/30. Cranial nerve examination is normal. Muscle strength is normal in all 4 limbs with normal muscle tone and deep tendon reflexes. Sensory examination is also normal. What is the most likely diagnosis?
- A. Huntington’s disease
- B. Pick’s disease (Correct Answer)
- C. Creutzfeldt–Jakob disease
- D. Lewy body dementia
- E. Alzheimer’s disease
Frontotemporal dementia Explanation: ***Pick’s disease***
* This patient presents with prominent **behavioral changes** (rudeness, irritability, accusation of black magic) and **language difficulties** (finding words, recalling names of objects), along with impaired financial management—these are characteristic features of **frontotemporal dementia (FTD)**, of which Pick's disease is a subtype.
* The early onset of behavioral symptoms and language deficits, with relative preservation of memory in the initial stages (MMSE 26/30), points towards FTD rather than Alzheimer's.
*Huntington’s disease*
* This condition is primarily characterized by **chorea** (involuntary jerky movements) and **psychiatric symptoms** often preceding motor dysfunction, which are not described in the patient.
* While dementia can occur, it typically manifests later in the disease course and is often overshadowed by prominent motor symptoms.
*Creutzfeldt–Jakob disease*
* This rapidly progressive neurodegenerative disorder presents with quickly worsening dementia, often accompanied by **myoclonus**, ataxia, and other neurological signs, which are absent in this patient's slower progression and symptoms.
* The patient's symptoms have been ongoing for 8 months without the rapid global decline typical of CJD.
*Lewy body dementia*
* Key features of Lewy body dementia include **fluctuating cognition**, recurrent **visual hallucinations**, and **parkinsonism** (rigidity, bradykinesia), none of which are reported in this case.
* Psychiatric symptoms are common, but the specific type of behavioral disinhibition and language deficits presented here are less typical.
*Alzheimer’s disease*
* **Memory impairment** is typically the most prominent early symptom in Alzheimer's disease, whereas this patient's presentation is dominated by **behavioral changes** and **language difficulties**.
* While severe behavior changes can occur, they usually manifest in later stages; significant executive dysfunction and language problems without prominent initial memory loss are more indicative of frontotemporal dementia.
Frontotemporal dementia US Medical PG Question 9: A 60-year-old woman is brought into the office by her son. Her son states that the patient has been acting inappropriately over the last few years. She has been taking off her clothes in front of visitors and putting objects in her mouth. She has had no emotional response to the death of one of her close friends and was laughing at her funeral. She has almost no memory issues, but sometimes forgets how to use objects such as a telephone. She has no other medical issues and takes no medications. On exam, she has no focal neurological deficits and her mini-mental status exam is 25/30. What is the most likely diagnosis?
- A. Alzheimer's dementia
- B. Pick's disease (Correct Answer)
- C. Normal aging
- D. Vascular dementia
- E. Lewy body dementia
Frontotemporal dementia Explanation: ***Pick's disease***
- The patient's presentation with **disinhibition**, **inappropriate social behavior**, putting objects in her mouth (hyperorality), and **emotional blunting** with preserved memory are classic signs of **frontotemporal dementia (FTD)**, of which Pick's disease is a subtype.
- The relative preservation of memory and visuospatial skills, as indicated by a mini-mental status exam score of 25/30, further supports an FTD diagnosis over Alzheimer's.
*Alzheimer's dementia*
- This typically presents with **prominent memory impairment** (especially **episodic memory**) as an early and defining feature, which is not the case here.
- Behavioral changes in Alzheimer's dementia usually occur later in the disease progression, unlike the early and severe **disinhibition** seen in this patient.
*Normal aging*
- While some cognitive changes can occur with normal aging, such as mild slowing of processing speed or occasional word-finding difficulties, they do not include severe **disinhibition**, **hyperorality**, or marked personality changes.
- Normal aging does not cause significant impairment in daily functioning or inappropriate social behavior.
*Vascular dementia*
- This type of dementia is characterized by a **stepwise decline** in cognitive function, often associated with a history of **strokes** or **cardiovascular risk factors**.
- Its presentation is typically focal neurological deficits and cognitive deficits that correlate with the location of vascular lesions, which are not described in this patient.
*Lewy body dementia*
- Hallmarks of Lewy body dementia include **fluctuating cognition**, **recurrent visual hallucinations**, and **parkinsonism**, none of which are detailed in the patient's presentation.
- While behavioral disturbances can occur, the prominent and early disinhibition and hyperorality seen here are more indicative of frontotemporal dementia.
Frontotemporal dementia US Medical PG Question 10: A 77-year-old woman is brought to the physician for gradually increasing confusion and difficulty walking for the past 4 months. Her daughter is concerned because she has been forgetful and seems to be walking more slowly. She has been distracted during her weekly bridge games and her usual television shows. She has also had increasingly frequent episodes of urinary incontinence and now wears an adult diaper daily. She has hyperlipidemia and hypertension. Current medications include lisinopril and atorvastatin. Her temperature is 36.8°C (98.2°F), pulse is 84/min, respirations are 15/min, and blood pressure is 139/83 mmHg. She is confused and oriented only to person and place. She recalls 2 out of 3 words immediately and 1 out of 3 after five minutes. She has a broad-based gait and takes short steps. Sensation is intact and muscle strength is 5/5 throughout. Laboratory studies are within normal limits. Which of the following is the most likely diagnosis in this patient?
- A. Pseudodementia
- B. Normal pressure hydrocephalus (Correct Answer)
- C. Creutzfeldt-Jakob disease
- D. Frontotemporal dementia
- E. Dementia with Lewy-bodies
Frontotemporal dementia Explanation: ***Normal pressure hydrocephalus***
- The constellation of **gradually increasing confusion**, an **ataxic gait** (broad-based, short steps), and **urinary incontinence** in an elderly patient is the classic triad of **normal pressure hydrocephalus (NPH)**.
- Lumbar puncture with temporary symptom improvement or **neuroimaging** showing ventriculomegaly without significant sulcal atrophy would further support this diagnosis.
*Pseudodementia*
- **Pseudodementia** is a cognitive impairment primarily caused by **depression**, characterized by rapid onset of symptoms and often a history of mood disturbances.
- The patient's progressive decline over 4 months and lack of overt depressive symptoms make this less likely.
*Creutzfeldt-Jakob disease*
- **Creutzfeldt-Jakob disease (CJD)** is a rapidly progressive and fatal neurodegenerative disorder characterized by a very fast decline in cognitive function, typically over months, along with **myoclonus**, ataxia, and other neurological signs.
- The slower, more subtle progression of symptoms and absence of myoclonus make CJD less likely.
*Frontotemporal dementia*
- **Frontotemporal dementia (FTD)** usually presents with prominent early changes in **personality, behavior**, or **language (aphasia)**, rather than the classic NPH triad.
- While confusion can occur, gait disturbance and incontinence are not typically primary or early features.
*Dementia with Lewy-bodies*
- **Dementia with Lewy bodies (DLB)** is characterized by **fluctuating cognition**, **recurrent visual hallucinations**, and **spontaneous parkinsonism**.
- While gait disturbance can occur (parkinsonism), the absence of hallucinations and significant cognitive fluctuations makes NPH a more fitting diagnosis for the specific triad presented.
More Frontotemporal dementia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.