Alzheimer's disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Alzheimer's disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Alzheimer's disease US Medical PG Question 1: A 71-year-old man is brought in by his daughter for forgetfulness. The daughter finds herself repeating things she has already told him. She also reports that the patient recently missed a lunch date they had scheduled. She is worried that he may have Alzheimer's disease because her mother had it, and this is how it started. The patient states that he sometimes forgets where he puts his glasses, but this is not new. He also admits to missing appointments if he doesn't write them in his planner, but he states “I always remember birthdays.” Since his wife passed, the patient has been responsible for all the finances, and the daughter confirms that he pays the bills on time. He cooks for himself, though sometimes he is “lazy” and will order fast food. The patient’s medical history is significant for hypertension, atherosclerosis, and rheumatoid arthritis. His medications include aspirin, lisinopril, atorvastatin, and methotrexate. He was also treated for depression for the first year following his wife's death, which was 3 years ago. He currently denies feelings of depression or suicidal ideation, but admits that he has been thinking more about death since some of his weekly golfing buddies have passed away. He drinks a beer every night with dinner and smokes cigars socially. A physical examination reveals ulnar deviation of the fingers, decreased grip strength, and a slow, steady gait. The patient is able to spell a 5-letter word backwards and remembers 3/3 items after 5 minutes. Which of the following diagnoses most likely explains the patient’s symptoms?
- A. Vascular dementia
- B. Alzheimer disease
- C. Frontotemporal dementia
- D. Normal aging (Correct Answer)
- E. Major depressive disorder
Alzheimer's disease Explanation: ***Normal aging***
- The patient exhibits age-associated memory impairment, such as occasional forgetfulness (e.g., misplacing glasses, missing an appointment if not written down), but his **activities of daily living** (ADLs) and instrumental ADLs (IADLs) like managing finances and cooking are **intact**.
- His cognitive function, evidenced by recalling 3/3 items after 5 minutes and spelling a 5-letter word backward, is **normal for his age**, and there's no significant decline affecting his overall function.
*Vascular dementia*
- This dementia type typically presents with a **step-wise decline** in cognitive function and often has **focal neurological deficits** corresponding to ischemic events.
- The patient's history of **hypertension and atherosclerosis** are risk factors, but his current symptoms do not suggest a significant, progressive decline or focal neurological signs indicative of vascular dementia.
*Alzheimer disease*
- Characterized by **progressive memory decline** that significantly impacts ADLs and IADLs, often starting with difficulty learning and recalling new information, which is not evident here.
- While familial history is a risk factor, the patient's ability to manage finances, cook, and perform well on short cognitive tests makes Alzheimer's less likely at this stage.
*Frontotemporal dementia*
- Primarily affects **personality, behavior, and language** earlier than memory, often leading to disinhibition, apathy, or language difficulties.
- The patient's presentation does not describe significant changes in personality or behavior, distinguishing it from frontotemporal dementia.
*Major depressive disorder*
- Although the patient had a history of depression and mentions thinking about death (contextually appropriate given friends' recent deaths), he **denies current feelings of depression or suicidal ideation**.
- His forgetfulness is mild and does not show features of **pseudodementia** (depression-related cognitive impairment), which typically presents with more prominent subjective complaints, poor effort on testing, and greater functional impairment than objective findings suggest.
- His **normal performance** on cognitive testing (3/3 recall) further argues against depression-related cognitive dysfunction.
Alzheimer's disease US Medical PG Question 2: A 66-year-old man is brought into the emergency department by his daughter for a change in behavior. Yesterday the patient seemed more confused than usual and was asking the same questions repetitively. His symptoms have not improved over the past 24 hours, thus the decision to bring him in today. Last year, the patient was almost completely independent but he then suffered a "series of falls," after which his ability to care for himself declined. After this episode he was no longer able to cook for himself or pay his bills but otherwise had been fine up until this episode. The patient has a past medical history of myocardial infarction, hypertension, depression, diabetes mellitus type II, constipation, diverticulitis, and peripheral neuropathy. His current medications include metformin, insulin, lisinopril, hydrochlorothiazide, sodium docusate, atorvastatin, metoprolol, fluoxetine, and gabapentin. On exam you note a confused man who is poorly kept. He has bruises over his legs and his gait seems unstable. He is alert to person and place, and answers some questions inappropriately. The patient's pulse is 90/minute and his blood pressure is 170/100 mmHg. Which of the following is the most likely diagnosis?
- A. Normal aging
- B. Lewy body dementia
- C. Vascular dementia (Correct Answer)
- D. Pseudodementia (depression-related cognitive impairment)
- E. Alzheimer's dementia
Alzheimer's disease Explanation: ***Vascular dementia***
- This diagnosis is strongly supported by the patient's **stepwise decline** in cognitive function following a "series of falls" (likely small strokes or transient ischemic attacks) and his extensive history of **vascular risk factors** including hypertension, diabetes, and previous myocardial infarction.
- The acute worsening of confusion over 24 hours, coupled with pre-existing impaired executive function (inability to cook or pay bills), is characteristic of **vascular dementia's fluctuating course** and presentation often linked to new cerebrovascular events.
*Incorrect: Normal aging*
- **Normal aging** involves a very gradual and mild decline in cognitive functions, primarily affecting processing speed and memory recall, without significant impairment in daily activities.
- This patient's rapid, stepwise decline and inability to perform instrumental activities of daily living (IADLs) such as cooking and managing finances go beyond what is considered normal cognitive changes with aging.
*Incorrect: Lewy body dementia*
- **Lewy body dementia** is characterized by prominent **fluctuations in attention and alertness**, recurrent visual hallucinations, and spontaneous parkinsonism, none of which are explicitly mentioned as primary features in this patient's presentation.
- While fluctuations in confusion are present, the history of a clear stepwise decline post-falls and significant vascular risk factors points away from Lewy body dementia as the most likely primary cause.
*Incorrect: Pseudodementia (depression-related cognitive impairment)*
- **Pseudodementia** refers to cognitive impairment that occurs in the context of **major depression**, where patients may exhibit poor concentration, memory difficulties, and psychomotor slowing that mimics dementia.
- While this patient is on fluoxetine for depression, the **stepwise decline** after clear vascular events (falls), multiple vascular risk factors, and impaired executive function point to a true neurodegenerative process rather than depression-induced cognitive changes, which typically improve with treatment of the underlying mood disorder.
*Incorrect: Alzheimer's dementia*
- **Alzheimer's dementia** typically presents with a **gradual and progressive decline** in memory, particularly episodic memory, followed by other cognitive domains over several years.
- The patient's history of a clear **stepwise decline** in function after acute events (falls) and the strong presence of **vascular risk factors** make vascular dementia a more fitting diagnosis than Alzheimer's, which is not typically associated with such a sudden, step-like progression.
Alzheimer's disease US Medical PG Question 3: A 70-year-old female presents to you for an office visit with complaints of forgetfulness. The patient states that over the last several years, the patient has stopped cooking for herself even though she lives alone. Recently, she also forgot how to drive back home from the grocery store and has difficulty paying her bills. The patient says she has been healthy over her whole life and does not take any medications. Her vitals are normal and her physical exam does not reveal any focal neurological deficits. Her mini-mental status exam is scored 19/30 and her MRI reveals diffuse cortical atrophy. What is the best initial treatment for this patient's condition?
- A. Rivastigmine (Correct Answer)
- B. Memantine
- C. Bromocriptine
- D. Pramipexole
- E. Ropinirole
Alzheimer's disease Explanation: ***Rivastigmine***
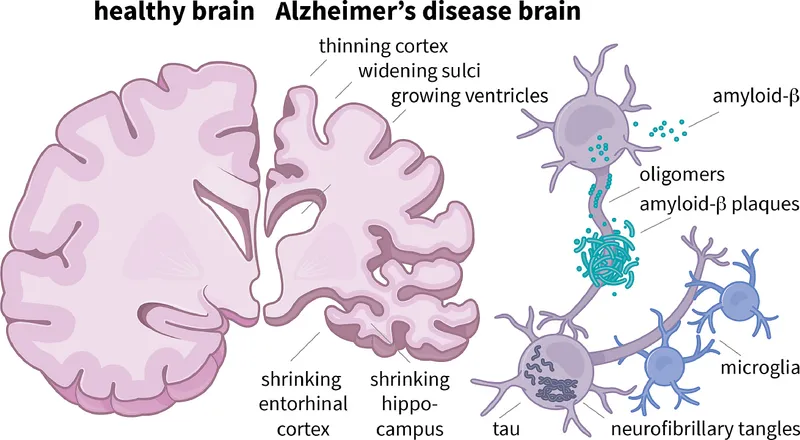
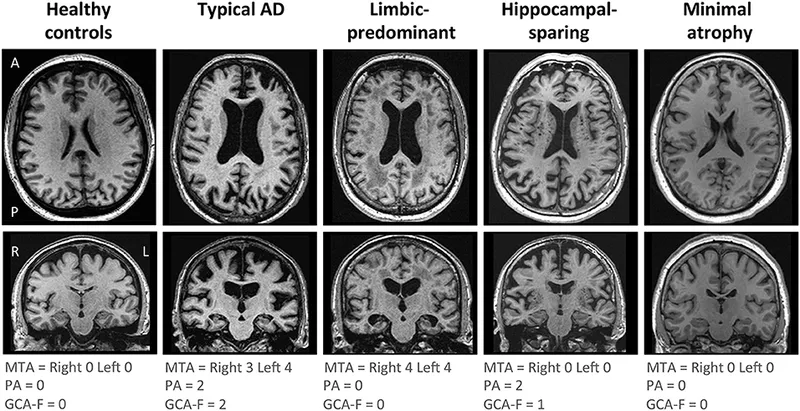
- This patient presents with symptoms and signs consistent with **Alzheimer's disease**, including gradual onset of **cognitive decline** impacting daily activities and diffuse cortical atrophy on MRI.
- **Rivastigmine** is an **acetylcholinesterase inhibitor** indicated for mild-to-moderate Alzheimer's disease, which works by increasing acetylcholine levels in the brain.
*Memantine*
- **Memantine** is an **NMDA receptor antagonist** typically used for **moderate-to-severe Alzheimer's disease**, often in combination with acetylcholinesterase inhibitors.
- While it can be beneficial, it is generally not considered the *initial* treatment for mild-to-moderate cases where acetylcholinesterase inhibitors are preferred.
*Bromocriptine*
- **Bromocriptine** is a **dopamine agonist** primarily used in the treatment of **Parkinson's disease** or hyperprolactinemia.
- It is not indicated for the management of Alzheimer's disease and would not address the underlying cholinergic deficit.
*Pramipexole*
- **Pramipexole** is a **dopamine agonist** used to treat **Parkinson's disease** and restless legs syndrome.
- It does not have a role in the treatment of Alzheimer's disease or other forms of dementia.
*Ropinirole*
- **Ropinirole** is another **dopamine agonist** primarily used for **Parkinson's disease** and restless legs syndrome.
- It is not an appropriate treatment for the cognitive decline seen in Alzheimer's disease.
Alzheimer's disease US Medical PG Question 4: A 53-year-old woman is brought to the physician by her husband for the evaluation of progressive memory loss, which he reports began approximately 2 weeks ago. During this time, she has had problems getting dressed and finding her way back home after running errands. She has also had several episodes of jerky, repetitive, twitching movements that resolved spontaneously. She is oriented only to person and place. She follows commands and speaks fluently. She is unable to read and has difficulty recognizing objects. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Mutant prion accumulation (Correct Answer)
- B. Copper accumulation
- C. Severe cerebral ischemia
- D. Increased number of CAG repeats
- E. Extracellular senile plaques
Alzheimer's disease Explanation: ***Mutant prion accumulation***
- The rapid progression of **dementia** (2 weeks), coupled with **myoclonus** (jerky, repetitive, twitching movements), is highly suggestive of **Creutzfeldt-Jakob disease (CJD)**, which is caused by mutant prion accumulation.
- CJD presents with a **spongiform encephalopathy** characterized by neuronal loss, astrocytosis, and vacuolation in the grey matter.
*Copper accumulation*
- **Copper accumulation** is characteristic of **Wilson's disease**, which typically presents with liver disease, neurological symptoms (e.g., dyskinesias, dystonia, tremor, psychiatric changes), and Kayser-Fleischer rings.
- The onset and rapid progression of symptoms, particularly the presence of myoclonus, are not typical for Wilson's disease.
*Severe cerebral ischemia*
- **Severe cerebral ischemia** can lead to sudden neurological deficits, but a diffuse, rapidly progressive cognitive decline and myoclonus like this is not typical of a single ischemic event.
- While strokes can cause dementia, the presentation here points to a more widespread and rapidly progressive neurodegenerative process.
*Increased number of CAG repeats*
- An increased number of **CAG repeats** is associated with **Huntington's disease**, which typically presents with chorea, psychiatric symptoms, and a more insidious onset of cognitive decline, usually without myoclonus as a prominent early feature.
- The rapid progression described in the patient is not typical of Huntington's disease.
*Extracellular senile plaques*
- **Extracellular senile plaques** (amyloid-beta) are a hallmark of **Alzheimer's disease**, which is characterized by a slowly progressive memory loss and cognitive decline over years, not weeks.
- While Alzheimer's eventually leads to severe cognitive impairment, the rapid onset and myoclonus make this diagnosis unlikely.
Alzheimer's disease US Medical PG Question 5: A 73-year-old woman is brought in by her daughter stating that her mom has become increasingly forgetful and has trouble remembering recent events. Her memory for remote events is remarkably intact. The patient is no longer able to cook for herself as she frequently leaves the stove on unattended. She has recently been getting lost in her neighborhood even though she has lived there for 30 years. Her mood is not depressed. Decreased activity in which of the following areas of the brain is known to be involved in the pathogenesis of Alzheimer's disease?
- A. Raphe nucleus
- B. Ventral tegmentum
- C. Nucleus basalis (Correct Answer)
- D. Locus ceruleus
- E. Nucleus accumbens
Alzheimer's disease Explanation: ***Nucleus basalis***
- The **nucleus basalis of Meynert** is a key cholinergic nucleus that projects widely to the cerebral cortex.
- **Loss of cholinergic neurons** in the nucleus basalis is a hallmark of Alzheimer's disease and is associated with cognitive decline, particularly in memory.
*Raphe nucleus*
- The raphe nuclei are the primary source of **serotonin** in the brain, playing a crucial role in mood, sleep, and appetite regulation.
- While serotonin dysregulation can occur in neurodegenerative diseases, core Alzheimer's pathology is not primarily linked to decreased activity here.
*Ventral tegmentum*
- The **ventral tegmental area (VTA)** is a major source of **dopamine** in the brain, involved in the reward system, motivation, and addiction.
- Decreased activity in the VTA is not a primary pathological feature of Alzheimer's disease, though dopaminergic pathways can be indirectly affected.
*Locus ceruleus*
- The **locus ceruleus** is the main source of **norepinephrine** in the brain, involved in arousal, attention, and stress responses.
- While it can be affected in Alzheimer's, especially later in the disease, primary pathogenesis is not attributed to its decreased activity.
*Nucleus accumbens*
- The **nucleus accumbens** is part of the **limbic system** and plays a central role in reward, pleasure, and motivation.
- While brain regions involved in motivation can be affected as dementia progresses, it is not a primary site of degeneration in Alzheimer's pathology.
Alzheimer's disease US Medical PG Question 6: A 69-year-old woman is brought to the physician by her daughter because of increasing forgetfulness and generalized fatigue over the past 4 months. She is unable to remember recent events and can no longer recognize familiar people. She lives independently, but her daughter has hired a helper in the past month since the patient has found it difficult to shop or drive by herself. She has stopped attending family functions and refuses to visit the neighborhood clubhouse, where she used to conduct game nights for the residents. She has had a 7-kg (15-lb) weight gain over this period. She is alert and oriented to time, place, and person. Her temperature is 36°C (97.6°F), pulse is 54/min, and blood pressure is 122/80 mm Hg. Mental status examination shows impaired attention and concentration; she has difficulty repeating seven digits forward and five in reverse sequence. She cannot recall any of the 3 objects shown to her after 10 minutes. She has no delusions or hallucinations. Further evaluation is most likely to show which of the following?
- A. Ventriculomegaly on CT scan of the head
- B. Elevated serum WBC count
- C. Decreased serum vitamin B12
- D. Elevated serum TSH (Correct Answer)
- E. Diffuse cortical atrophy on brain MRI
Alzheimer's disease Explanation: ***Elevated serum TSH***
- The patient's symptoms, including **forgetfulness**, generalized **fatigue**, weight gain, and **bradycardia** (pulse 54/min), are highly suggestive of **hypothyroidism**.
- **Hypothyroidism** can present with cognitive dysfunction (often mistaken for dementia), depression-like symptoms (withdrawal from social activities), and metabolic changes like weight gain.
*Ventriculomegaly on CT scan of the head*
- **Ventriculomegaly** is often associated with conditions like **Normal Pressure Hydrocephalus (NPH)**, which presents with a triad of gait disturbance, urinary incontinence, and dementia.
- While cognitive impairment is present, the absence of gait issues and incontinence makes NPH less likely, and other symptoms point away from it.
*Elevated serum WBC count*
- An **elevated WBC count** indicates an **infection** or inflammatory process.
- The patient's symptoms are chronic (4 months), subacute, and lack specific signs of infection such as fever (temperature is normal) or acute inflammation.
*Decreased serum vitamin B12*
- **Vitamin B12 deficiency** can cause cognitive impairment, fatigue, and neurological symptoms.
- However, it is typically associated with **anemia** and/or peripheral neuropathy, which are not mentioned in this patient's presentation.
*Diffuse cortical atrophy on brain MRI*
- **Diffuse cortical atrophy** is a common finding in various forms of **dementia**, such as **Alzheimer's disease**.
- While it's a possibility, other more treatable causes of cognitive decline, like hypothyroidism, should be investigated first given the constellation of symptoms.
Alzheimer's disease US Medical PG Question 7: A 53-year-old man is brought to the clinic by his son for the evaluation of unusual behavior. He is a shopkeeper by profession and sometimes behaves very rudely to the customers. Recently, he accused one of the customers of using black magic over his shop. He has been increasingly irritable, forgetting things, and having problems managing his finances over the past 8 months. He is also having difficulty finding words and recalling the names of objects during the conversation. There is no history of recent head trauma, fever, hallucinations, or abnormal limb movements. Past medical history is significant for a well-controlled type 2 diabetes mellitus. Family history is unremarkable. He does not smoke or use illicit drugs. Vital signs are stable with a blood pressure of 134/76 mm Hg, a heart rate of 88/min, and a temperature of 37.0°C (98.6°F). On physical examination, he has problems naming objects and planning tasks. Mini-mental state examination (MMSE) score is 26/30. Cranial nerve examination is normal. Muscle strength is normal in all 4 limbs with normal muscle tone and deep tendon reflexes. Sensory examination is also normal. What is the most likely diagnosis?
- A. Huntington’s disease
- B. Pick’s disease (Correct Answer)
- C. Creutzfeldt–Jakob disease
- D. Lewy body dementia
- E. Alzheimer’s disease
Alzheimer's disease Explanation: ***Pick’s disease***
* This patient presents with prominent **behavioral changes** (rudeness, irritability, accusation of black magic) and **language difficulties** (finding words, recalling names of objects), along with impaired financial management—these are characteristic features of **frontotemporal dementia (FTD)**, of which Pick's disease is a subtype.
* The early onset of behavioral symptoms and language deficits, with relative preservation of memory in the initial stages (MMSE 26/30), points towards FTD rather than Alzheimer's.
*Huntington’s disease*
* This condition is primarily characterized by **chorea** (involuntary jerky movements) and **psychiatric symptoms** often preceding motor dysfunction, which are not described in the patient.
* While dementia can occur, it typically manifests later in the disease course and is often overshadowed by prominent motor symptoms.
*Creutzfeldt–Jakob disease*
* This rapidly progressive neurodegenerative disorder presents with quickly worsening dementia, often accompanied by **myoclonus**, ataxia, and other neurological signs, which are absent in this patient's slower progression and symptoms.
* The patient's symptoms have been ongoing for 8 months without the rapid global decline typical of CJD.
*Lewy body dementia*
* Key features of Lewy body dementia include **fluctuating cognition**, recurrent **visual hallucinations**, and **parkinsonism** (rigidity, bradykinesia), none of which are reported in this case.
* Psychiatric symptoms are common, but the specific type of behavioral disinhibition and language deficits presented here are less typical.
*Alzheimer’s disease*
* **Memory impairment** is typically the most prominent early symptom in Alzheimer's disease, whereas this patient's presentation is dominated by **behavioral changes** and **language difficulties**.
* While severe behavior changes can occur, they usually manifest in later stages; significant executive dysfunction and language problems without prominent initial memory loss are more indicative of frontotemporal dementia.
Alzheimer's disease US Medical PG Question 8: A 72-year-old woman is brought to the physician by her son for an evaluation of cognitive decline. Her son reports that she has had increased difficulty finding her way back home for the last several months, despite having lived in the same city for 40 years. He also reports that his mother has been unable to recall the names of her relatives and been increasingly forgetting important family gatherings such as her grandchildren's birthdays over the last few years. The patient has hypertension and type 2 diabetes mellitus. She does not smoke or drink alcohol. Her current medications include enalapril and metformin. Her temperature is 37°C (98.6°F), pulse is 70/min, and blood pressure is 140/80 mm Hg. She is confused and oriented only to person and place. She recalls 2 out of 3 words immediately and 1 out of 3 after 5 minutes. Her gait and muscle strength are normal. Deep tendon reflexes are 2+ bilaterally. The remainder of the examination shows no abnormalities. Further evaluation is most likely to reveal which of the following findings?
- A. Generalized cerebral atrophy (Correct Answer)
- B. Myoclonic movements
- C. Hallucinations
- D. Urinary incontinence
- E. Resting tremor
Alzheimer's disease Explanation: ***Generalized cerebral atrophy***
- The patient's symptoms of progressive **cognitive decline**, including difficulty with navigation and memory, are classic signs of **Alzheimer's disease**.
- **Generalized cerebral atrophy**, particularly of the **hippocampus** and **temporal lobes**, is a hallmark pathological finding in Alzheimer's disease due to neuronal loss and synaptic dysfunction.
*Myoclonic movements*
- **Myoclonic movements** are sudden, brief, involuntary muscle jerks, most commonly associated with **Creutzfeldt-Jakob disease** or certain types of dementia with Lewy bodies, which are not suggested by the patient's presentation.
- While some rare forms of early-onset Alzheimer's can have atypical features, myoclonus is not a typical or early finding in the more common late-onset presentation described.
*Hallucinations*
- **Hallucinations**, particularly visual hallucinations, are frequently seen in **dementia with Lewy bodies** and **Parkinson's disease dementia**, often preceding or co-occurring with cognitive decline.
- While hallucinations can occur in late-stage Alzheimer's, they are not a prominent or early feature differentiating it from other dementias.
*Urinary incontinence*
- **Urinary incontinence** can be a symptom of various conditions, including **normal pressure hydrocephalus (NPH)**, which presents with a triad of gait instability, dementia, and urinary incontinence.
- In Alzheimer's disease, incontinence typically appears in the **later stages**, after significant cognitive impairment and functional decline have occurred.
*Resting tremor*
- A **resting tremor** is a characteristic symptom of **Parkinson's disease** and is often seen in **Parkinson's disease dementia** or **dementia with Lewy bodies**.
- The patient's neurological examination, including normal gait and muscle strength, does not suggest Parkinsonian features.
Alzheimer's disease US Medical PG Question 9: A 78-year-old man is brought to the physician by his daughter for a follow-up examination. The daughter noticed that he has gradually become more forgetful and withdrawn over the last year. He frequently misplaces his car keys and forgets the names of his neighbors, whom he has known for 30 years. He has difficulty recalling his address and telephone number. He recently had an episode of urinary and fecal incontinence. Last week, his neighbor found him wandering the parking lot of the grocery store. He has hypertension and hyperlipidemia. He had smoked one pack of cigarettes daily for 40 years but quit 18 years ago. His current medications include hydrochlorothiazide and atorvastatin. He appears healthy; BMI is 23 kg/m2. His temperature is 37.2°C (99.0°F), pulse is 86/min, respirations are 14/min, and blood pressure is 136/84 mm Hg. Mini-mental state examination score is 19/30. He is not bothered by his forgetfulness. Cranial nerves II–XII are intact. He has 5/5 strength and full sensation to light touch in all extremities. His patellar, Achilles, and biceps reflexes are 2+ bilaterally. His gait is steady. MRI scan of the brain shows ventriculomegaly and prominent cerebral sulci. Which of the following is the most appropriate pharmacotherapy?
- A. Acetazolamide
- B. Sertraline
- C. Memantine
- D. Thiamine
- E. Donepezil (Correct Answer)
Alzheimer's disease Explanation: ***Donepezil***
- The patient exhibits features consistent with **Alzheimer's disease**, including gradual memory loss, difficulty with daily tasks, episodes of incontinence, and a Mini-Mental State Examination (MMSE) score of 19/30. Donepezil, a **cholinesterase inhibitor**, is a first-line treatment for mild to moderate Alzheimer's to slow cognitive decline.
- The MRI findings of **ventriculomegaly and prominent cerebral sulci** are consistent with general cerebral atrophy often seen in Alzheimer's disease, not hydrocephalus requiring shunting or other specific brain pathologies (normal pressure hydrocephalus would have gait disturbance as a prominent feature, which is absent here).
*Acetazolamide*
- **Acetazolamide** is a **carbonic anhydrase inhibitor** used to treat conditions like glaucoma, altitude sickness, and idiopathic intracranial hypertension.
- There is no indication of elevated intracranial pressure or hydrocephalus that would warrant the use of acetazolamide in this patient.
*Sertraline*
- **Sertraline** is a **selective serotonin reuptake inhibitor (SSRI)** primarily used to treat depression, anxiety disorders, and obsessive-compulsive disorder.
- While depression can coexist with dementia, the primary cognitive symptoms described here are not primarily depressive; therefore, an antidepressant is not the most appropriate initial pharmacotherapy for cognitive decline.
*Memantine*
- **Memantine** is an **NMDA receptor antagonist** used in moderate to severe Alzheimer's disease, often in combination with cholinesterase inhibitors or when cholinesterase inhibitors are not tolerated.
- While appropriate for moderate to severe Alzheimer's, **cholinesterase inhibitors** are typically the initial treatment for mild to moderate stages, and the patient's MMSE score of 19/30 often falls into the mild-moderate category where donepezil is usually favored first.
*Thiamine*
- **Thiamine** (vitamin B1) supplementation is primarily used to treat **Wernicke-Korsakoff syndrome**, which is associated with chronic alcohol abuse and presents with ataxia, ophthalmoplegia, and confusion, none of which are the primary presenting symptoms here.
- There is no evidence of **nutritional deficiency** or alcohol abuse in this patient to suggest thiamine deficiency as the cause of his cognitive decline.
Alzheimer's disease US Medical PG Question 10: A 68-year-old man seeks evaluation by a physician with complaints of worsening forgetfulness and confusion for 1 year. According to his wife, he has always been in good health and is generally very happy; however, he has started to forget important things. He recently had his driving license revoked because of multiple tickets, but he cannot recall having done anything wrong. This morning, he neglected to put on his socks and was quite agitated when she pointed this out to him. He denies having a depressed mood, sleep problems, or loss of interest. He occasionally has a glass of wine with dinner and has never smoked or used recreational drugs. His medical history and family medical history are unremarkable. His pulse is 68/min, respirations are 14/min, and blood pressure is 130/84 mm Hg. Except for a mini-mental state examination (MMSE) score of 20/30, the remainder of the physical examination is unremarkable. Imaging studies, including a chest X-ray and CT of the brain, reveal no pathologic findings. An electrocardiogram (ECG) is also normal. Laboratory testing showed the following:
Serum glucose (fasting) 76 mg/dL
Serum electrolytes:
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Serum creatinine 0.9 mg/dL
Blood urea nitrogen 11 mg/dL
Cholesterol, total: 180 mg/dL
HDL-cholesterol 45 mg/dL
LDL-cholesterol 75 mg/dL
Triglycerides 135 mg/dL
Hemoglobin (Hb%) 16 g/dL
Mean corpuscular volume (MCV) 85 fL
Reticulocyte count 0.9%
Erythrocyte count 5 million/mm³
Thyroid-stimulating hormone 3.5 µU/mL
Urinalysis
Glucose Negative
Ketones Negative
Leucocytes Negative
Nitrite Negative
RBCs Negative
Casts Negative
Which of the following is the most likely diagnosis?
- A. Alzheimer’s dementia (Correct Answer)
- B. Creutzfeldt-Jakob disease
- C. Lewy body dementia
- D. Parkinson’s disease
- E. Vascular dementia
Alzheimer's disease Explanation: ***Alzheimer’s dementia***
- The patient presents with **progressive memory loss** and **confusion** that has worsened over a year, along with **agitational behavior** and difficulty with daily tasks (neglecting to put on socks), which are classic symptoms of Alzheimer's dementia.
- The **MMSE score of 20/30** indicates cognitive impairment, and the absence of other neurological findings or clear vascular risk factors supports this diagnosis.
*Creutzfeldt-Jakob disease*
- This is a rare, rapidly progressive, and fatal neurodegenerative disease that typically presents with **rapidly progressive dementia**, **myoclonus**, and other neurological signs, which are not described in this case.
- The patient's symptoms have progressed over a year, which is not as rapid as the typical course of CJD.
*Lewy body dementia*
- Characterized by **fluctuating cognition**, **recurrent visual hallucinations**, and **spontaneous parkinsonism**, which are not reported in this patient.
- While agitation can occur, the core features of Lewy body dementia are absent.
*Parkinson’s disease*
- Primarily a **movement disorder** characterized by **bradykinesia**, **rigidity**, **tremor**, and **postural instability**. While dementia can occur in later stages (Parkinson's disease dementia), the initial presentation in this patient is predominantly cognitive decline without prominent motor symptoms.
- The patient's physical examination is "unremarkable," suggesting an absence of parkinsonian motor signs.
*Vascular dementia*
- Typically associated with a history of **stroke** or significant **vascular risk factors** (e.g., uncontrolled hypertension, diabetes) and often presents with a **step-wise decline** in cognitive function.
- This patient has a largely unremarkable medical history, controlled blood pressure, and normal cholesterol, and a CT scan showed no pathological findings (e.g., infarcts), making vascular dementia less likely.
More Alzheimer's disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.