Manic episode criteria and features US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Manic episode criteria and features. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Manic episode criteria and features US Medical PG Question 1: A 19-year-old woman is brought to the physician by her parents because of irritable mood that started 5 days ago. Since then, she has been staying up late at night working on a secret project. She is energetic despite sleeping less than 4 hours per day. Her parents report that she seems easily distracted. She is usually very responsible, but this week she spent her paycheck on supplies for her project. She has never had similar symptoms before. In the past, she has had episodes where she felt too fatigued to go to school and slept until 2 pm every day for 2 weeks at a time. During those times, her parents noticed that she cried excessively, was very indecisive, and expressed feelings of worthlessness. Two months ago, she had an asthma exacerbation and was treated with bronchodilators and steroids. She tried cocaine once in high school but has not used it since. Vital signs are within normal limits. On mental status examination, she is irritable but cooperative. Her speech is pressured and her thought process is linear. Which of the following is the most likely diagnosis?
- A. Major depressive disorder
- B. Bipolar I disorder
- C. Bipolar II disorder (Correct Answer)
- D. Schizoaffective disorder
- E. Substance abuse
Manic episode criteria and features Explanation: ***Bipolar II disorder***
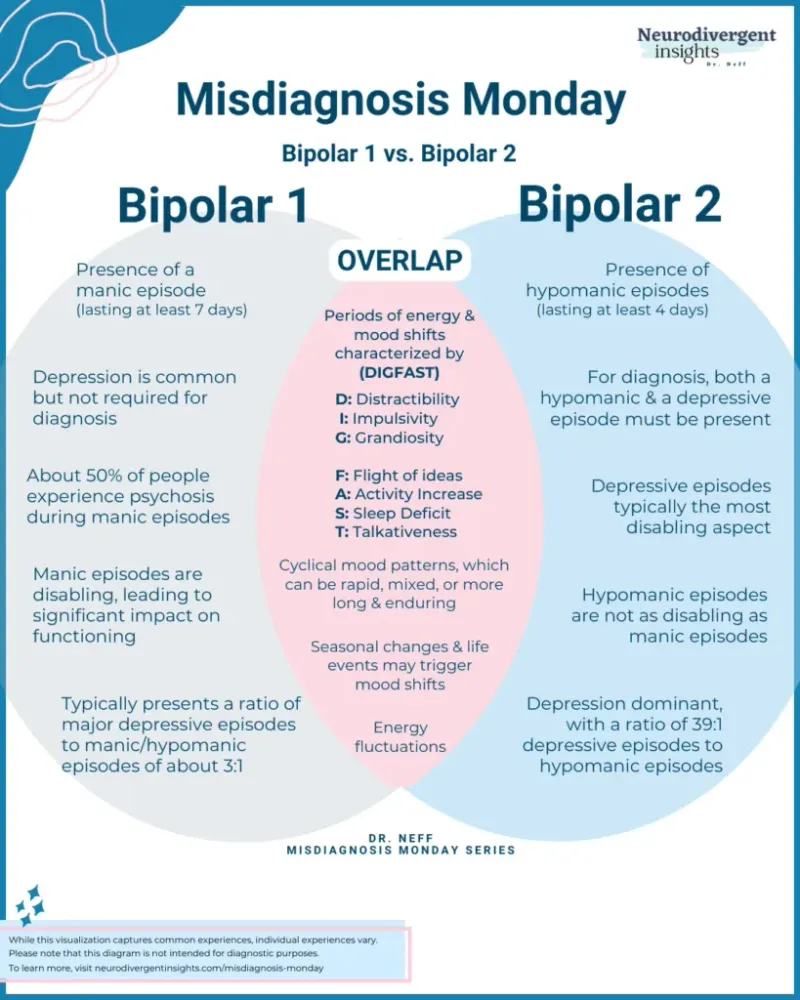
- This patient exhibits symptoms consistent with both **hypomania** (increased energy, decreased need for sleep, irritability, distractibility, spending sprees) and past episodes of **major depression** (fatigue, hypersomnia, crying, indecisiveness, worthlessness). The key distinction for Bipolar II is the presence of at least one hypomanic episode and one major depressive episode, without a full manic episode.
- The current symptoms of increased energy and decreased need for sleep for 5 days, along with a significant change in behavior (spending paycheck on a "secret project"), indicate a level of impairment consistent with hypomania, rather than a full-blown mania as the thought process is described as linear.
*Major depressive disorder*
- While the patient has a history of depressive episodes, the current presentation with **elevated mood, increased energy, and decreased need for sleep** is inconsistent with a unipolar depressive episode.
- Major depressive disorder does not involve periods of elevated or irritable mood or increased activity.
*Bipolar I disorder*
- Bipolar I disorder requires the occurrence of at least one **manic episode**. While the patient's current symptoms are suggestive of a mood elevation, they do not meet the criteria for full mania, which typically involves severe impairment, psychotic features, or hospitalization.
- The patient's speech is pressured but her thought process is described as **linear**, which is less typical for a full manic episode where **flight of ideas** or **tangential/disorganized thinking** might be present.
*Schizoaffective disorder*
- Schizoaffective disorder involves a period of uninterrupted illness during which there is a **major mood episode (depressive or manic) concurrent with symptoms of schizophrenia**, such as delusions or hallucinations.
- The patient's symptoms are primarily mood-related, and there is no mention of psychotic symptoms independent of the mood disturbance.
*Substance abuse*
- Although the patient used cocaine once in high school, there is no evidence of recent substance use that would explain the current symptoms. The symptoms are sustained over days and include a history of recurrent mood disturbances.
- While the patient received steroid treatment 2 months ago (which can precipitate mood episodes), the timing and clinical presentation are more consistent with a primary mood disorder rather than a substance/medication-induced disorder.
Manic episode criteria and features US Medical PG Question 2: A 24-year-old man is brought to your emergency department under arrest by the local police. The patient was found naked at a busy intersection jumping up and down on top of a car. Interviewing the patient, you discover that he has not slept in 2 days because he does not feel tired. He reports hearing voices. The patient was previously hospitalized 1 year ago with auditory hallucinations, paranoia, and a normal mood. What is the most likely diagnosis?
- A. Schizophrenia
- B. Bipolar disorder
- C. Brief psychotic disorder
- D. Schizotypal disorder
- E. Schizoaffective disorder (Correct Answer)
Manic episode criteria and features Explanation: ***Schizoaffective disorder***
- This patient demonstrates the **hallmark feature** of schizoaffective disorder: **psychotic symptoms occurring both during AND independent of mood episodes**.
- **Current presentation**: Clear **manic episode** (decreased need for sleep, grandiose/disinhibited behavior, psychomotor agitation) with psychotic features (auditory hallucinations).
- **Previous hospitalization**: **Psychotic symptoms (hallucinations, paranoia) in the absence of a mood episode** ("normal mood"), requiring hospitalization for at least 2 weeks - this is the **key diagnostic criterion** for schizoaffective disorder.
- The diagnosis requires an **uninterrupted period of illness** with both psychotic symptoms (meeting Criterion A for schizophrenia) and a major mood episode, PLUS psychotic symptoms for **≥2 weeks without prominent mood symptoms**.
*Bipolar disorder*
- In bipolar disorder with psychotic features, psychotic symptoms occur **exclusively during mood episodes** (manic, hypomanic, or depressive).
- This patient's previous hospitalization with psychosis but **"normal mood"** indicates psychotic symptoms independent of mood episodes, which **rules out** bipolar disorder and points to schizoaffective disorder.
- While the current presentation shows mania with psychosis, the longitudinal course is critical for diagnosis.
*Schizophrenia*
- Schizophrenia involves **continuous psychotic symptoms** without prominent mood episodes dominating the clinical picture.
- This patient has **prominent manic symptoms** (decreased sleep, grandiose behavior, agitation) that are central to the current presentation, making schizophrenia less likely.
- The presence of full mood episodes that occupy a **substantial portion** of the illness duration favors schizoaffective disorder over schizophrenia.
*Brief psychotic disorder*
- Brief psychotic disorder involves psychotic symptoms lasting **<1 month** with full return to baseline functioning.
- This patient has a **recurrent course** with hospitalization 1 year ago, indicating a chronic/recurring condition rather than a brief, self-limited episode.
*Schizotypal disorder*
- This is a **personality disorder** characterized by social deficits, cognitive/perceptual distortions, and eccentric behavior, but **NOT overt psychotic episodes**.
- Does not involve acute psychotic breaks with severe symptoms like hallucinations requiring hospitalization or manic episodes.
Manic episode criteria and features US Medical PG Question 3: A 57-year-old man is brought to the emergency department by the police after he was found running around a local park naked and screaming late at night. During intake, the patient talks non-stop about the government spying on him and his family, but provides little useful information besides his name and date of birth. Occasionally he refers to himself in the third person. He refuses to eat anything and will only drink clear fluids because he is afraid of being poisoned. A medical records search reveals that the patient has been treated for psychotic behavior and occasional bouts of severe depression for several years. Today, his heart rate is 90/min, respiratory rate is 19/min, blood pressure is 135/85 mm Hg, and temperature is 37.0°C (98.6°F). On physical exam, he appears gaunt and anxious. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. CMP, CBC, and TSH are normal. A urine toxicology test is negative. What is the most likely diagnosis?
- A. Schizophrenia
- B. Major depressive disorder
- C. Schizoaffective disorder (Correct Answer)
- D. Brief psychotic disorder
- E. Bipolar 1 disorder
Manic episode criteria and features Explanation: ***Schizoaffective disorder***
- The patient exhibits features of both a **mood disorder** (severe depression) and a **psychotic disorder** (delusions, disorganized behavior, referring to himself in the third person), which are key characteristics of schizoaffective disorder.
- The history of **psychotic behavior** and **severe depression** over several years, with current presentation involving both prominent mood symptoms (agitation, gaunt appearance suggesting poor self-care due to mood) and psychotic features (paranoia, disorganized speech), supports this diagnosis over other psychotic or mood disorders.
*Schizophrenia*
- While the patient exhibits **psychotic symptoms** (delusions, disorganization), the history of "occasional bouts of severe depression" suggests a more prominent and recurring mood component than typically seen in schizophrenia.
- In schizophrenia, mood symptoms are often confined to brief periods relative to the duration of the psychotic illness or are not a prominent and defining feature.
*Major depressive disorder*
- This diagnosis is incorrect because the patient displays clear and pervasive **psychotic symptoms** such as paranoia, disorganized speech, and bizarre behavior (running naked, screaming), which are beyond what is typically seen in major depressive disorder with psychotic features (where psychosis is congruent with the depressive theme).
- The historical pattern of **psychotic behavior** occurring separately from or alongside depressive episodes points away from a primary diagnosis of major depressive disorder.
*Brief psychotic disorder*
- This diagnosis is characterized by psychotic symptoms lasting **less than one month**, with an eventual full return to premorbid functioning.
- The patient's history of **several years** of psychotic behavior and severe depression rules out this acute and time-limited condition.
*Bipolar 1 disorder*
- While bipolar 1 disorder can feature **psychotic symptoms** during manic or depressive episodes, the presentation here emphasizes persistent psychotic features (delusions of being spied on, fear of poisoning) that are not always directly tied to mood episodes or are more enduring than typical for bipolar disorder.
- The long-standing history of both **psychotic and depressive episodes** suggests a more integrated condition of mood and psychosis rather than distinct episodes as seen in bipolar 1 disorder.
Manic episode criteria and features US Medical PG Question 4: A 29-year-old man comes to the physician with his wife because she has noticed a change in his behavior over the past 2 weeks. His wife reports that he is very distracted and irritable. His colleagues have voiced concerns that he has not been turning up for work regularly and behaves erratically when he does. Previously, her husband had been a reliable and reasonable person. The patient says that he feels “fantastic”; he only needs 4 hours of sleep each night and wakes up cheerful and full of energy each morning. He thinks that his wife is overreacting. The patient has been healthy except for a major depressive episode 5 years ago that was treated with paroxetine. He currently takes no medications. His pulse is 98/min, respirations are 12/min, and blood pressure is 128/62 mm Hg. Mental status examination shows frenzied speech and a flight of ideas. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Advanced paternal age
- B. Genetic predisposition (Correct Answer)
- C. Higher socioeconomic class
- D. Maternal obstetric complications
- E. Being married
Manic episode criteria and features Explanation: ***Genetic predisposition***
- A strong **genetic predisposition** is a primary predisposing factor for bipolar disorder, as evidenced by a significantly higher concordance rate in monozygotic twins compared to dizygotic twins or the general population.
- The patient's presentation with **manic symptoms** (decreased need for sleep, euphoria, irritability, frenzied speech, flight of ideas, erratic behavior) following a history of a **major depressive episode** is highly suggestive of **bipolar I disorder**.
*Advanced paternal age*
- While advanced paternal age has been associated with an increased risk of some neurodevelopmental disorders like **schizophrenia** and **autism spectrum disorder**, its link to bipolar disorder is less robust and not considered the strongest predisposing factor.
- The primary risk factor for bipolar disorder involves heritability rather than specific parental age.
*Higher socioeconomic class*
- There is **no consistent evidence** to suggest that higher socioeconomic class is a predisposing factor for bipolar disorder.
- Bipolar disorder affects individuals across all socioeconomic levels.
*Maternal obstetric complications*
- Maternal obstetric complications, such as **prenatal infections** or **hypoxia**, have been implicated in the development of certain psychiatric disorders, particularly **schizophrenia**.
- However, for bipolar disorder, genetic factors play a far more significant and direct role than obstetric complications.
*Being married*
- **Marital status** does not serve as a predisposing factor for the development of bipolar disorder.
- While relationship challenges can be a consequence or stressor for individuals with bipolar disorder, marriage itself is not a cause.
Manic episode criteria and features US Medical PG Question 5: A 21-year-old female is brought to the emergency department by her roommate. Her roommate says that the patient has been acting “strangely” for the past 10 days. She has noticed that the patient has been moving and talking on the phone at all hours of the night. She doesn’t think that the patient sleeps more than one to two hours a night. She also spends hours pacing up and down the apartment, talking about “trying to save the world.” She also notices that the patient has been speaking very fast. When asking the patient if anything seems different, the patient denies anything wrong, only adding that, “she’s made great progress on her plans." The patient said she has felt like this on one occasion 2 years ago, and she recalled being hospitalized for about 2 weeks. She denies any history of depression, although she said about a year ago she had no energy and had a hard time motivating herself to go to class and see her friends for months. She denies hearing any voices or any visual hallucinations. What is the most likely diagnosis in this patient?
- A. Bipolar II disorder
- B. Bipolar I disorder (Correct Answer)
- C. Major depressive disorder
- D. Persistent Depressive Disorder
- E. Schizoaffective disorder
Manic episode criteria and features Explanation: ***Bipolar I disorder***
- The patient exhibits clear symptoms of a **manic episode**, including decreased need for sleep, grandiosity ("saving the world"), pressured speech, and increased goal-directed activity, which are characteristic of Bipolar I disorder.
- The history of a prior hospitalization for similar symptoms ("felt like this on one occasion 2 years ago, and she recalled being hospitalized") and self-reported depressive episodes ("she had no energy... for months") further supports the diagnosis of Bipolar I disorder, which requires at least one manic episode.
*Bipolar II disorder*
- Bipolar II disorder involves at least one **hypomanic episode** and at least one major depressive episode.
- The severity of the patient's current symptoms, including significant functional impairment and a prior hospitalization for similar symptoms, indicates a **manic episode**, not a hypomanic episode.
*Major depressive disorder*
- This diagnosis is characterized solely by **major depressive episodes** without any history of manic or hypomanic episodes.
- The patient's presentation clearly includes symptoms of **mania**, ruling out a sole diagnosis of major depressive disorder.
*Persistent Depressive Disorder*
- This disorder is characterized by **chronic, mild depressive symptoms** lasting at least two years.
- The patient's current presentation of severe manic symptoms and past episodes of clear mania differentiates her condition from persistent depressive disorder.
*Schizoaffective disorder*
- Schizoaffective disorder involves a period of uninterrupted illness during which there is a **major mood episode (depressive or manic) concurrent with symptoms of schizophrenia**, such as hallucinations or delusions, for at least two weeks in the absence of a major mood episode.
- The patient **denies hearing any voices or visual hallucinations**, making schizoaffective disorder less likely; her symptoms are primarily mood-related.
Manic episode criteria and features US Medical PG Question 6: A 28-year-old woman presents with continuous feelings of sadness and rejection. She says that over the past couple of weeks, she has been unable to concentrate on her job and has missed several days of work. She also has no interest in any activity and typically rejects invitations to go out with friends. She has no interest in food or playing with her dog. Her husband is concerned about this change in behavior. A few months ago, she was very outgoing and made many plans with her friends. She remembers being easily distracted and also had several ‘brilliant ideas’ on what she should be doing with her life. She did not sleep much during that week, but now all she wants to do is lie in bed all day. She denies any suicidal or homicidal ideations. She has no past medical history and has never been hospitalized. Laboratory tests were normal. Which of the following is the most likely diagnosis in this patient?
- A. Major depressive disorder
- B. Dysthymia
- C. Bipolar disorder, type II (Correct Answer)
- D. Schizoaffective disorder
- E. Bipolar disorder, type I
Manic episode criteria and features Explanation: ***Bipolar disorder, type II***
− This patient's current symptoms of profound **sadness, anhedonia, low energy, and social withdrawal** are indicative of a major depressive episode.
− The history of prior periods of **decreased need for sleep, brilliant ideas, and being easily distracted** suggests a hypomanic episode, a hallmark of bipolar disorder type II.
*Major depressive disorder*
− While the patient is currently experiencing a **major depressive episode**, the history of previous hypomanic symptoms rules out a diagnosis of unipolar major depressive disorder.
− **Major depressive disorder** does not include a history of manic or hypomanic episodes.
*Dysthymia*
− **Dysthymia** (persistent depressive disorder) is characterized by chronic, milder depressive symptoms lasting at least two years.
− The current episode is severe and marked by a clear change from a previous elevated mood state, which is inconsistent with dysthymia.
*Schizoaffective disorder*
− **Schizoaffective disorder** involves episodes of mood disturbance alongside symptoms of schizophrenia (e.g., hallucinations, delusions) that occur at least two weeks without prominent mood symptoms.
− This patient's symptoms are primarily mood-related and do not include psychotic features characteristic of schizophrenia.
*Bipolar disorder, type I*
− **Bipolar disorder type I** is characterized by the occurrence of at least one manic episode, which involves more severe symptoms, significant impairment, and often psychosis.
− The patient's previous "brilliant ideas" and decreased need for sleep describe a **hypomanic episode** rather than a full manic episode and are not associated with marked functional impairment or psychotic features.
Manic episode criteria and features US Medical PG Question 7: A 16-year-old girl presents with multiple manic and hypomanic episodes. The patient says that these episodes started last year and have progressively worsened. She is anxious to start treatment, so this will not impact her school or social life. The patient was prescribed an anticonvulsant drug that is also used to treat her condition. Which of the following is the drug most likely prescribed to this patient?
- A. Lithium
- B. Phenobarbital
- C. Valproic acid (Correct Answer)
- D. Diazepam
- E. Clonazepam
Manic episode criteria and features Explanation: ***Valproic acid***
- **Valproic acid** is an **anticonvulsant** commonly used as a **mood stabilizer** in bipolar disorder, especially for rapid cycling or mixed manic episodes.
- Its broad-spectrum anticonvulsant properties make it effective for various seizure types, in addition to its use in bipolar disorder, fitting the description of a drug used for both.
*Lithium*
- While **lithium** is a first-line treatment for **bipolar disorder**, it is not primarily an **anticonvulsant** drug, making it less likely given the specific prompt.
- It has a narrow therapeutic index and requires regular monitoring, which can be a consideration in treatment compliance.
*Phenobarbital*
- **Phenobarbital** is an older **barbiturate anticonvulsant** and sedative, but it is not typically used for treating **bipolar disorder** due to its significant side effects and potential for dependence.
- Its primary use is in seizure control, not mood stabilization.
*Diazepam*
- **Diazepam** is a **benzodiazepine** used for acute anxiety, seizures, and muscle spasms, but it is not a primary **mood stabilizer** for bipolar disorder.
- It would be used for acute agitation or anxiety symptoms, not long-term mood regulation.
*Clonazepam*
- **Clonazepam** is another **benzodiazepine** with anticonvulsant properties, often used for anxiety and panic disorders, but generally not as a primary mood stabilizer in **bipolar disorder**.
- While it can help with acute agitation, it does not address the underlying mood dysregulation of bipolar disorder.
Manic episode criteria and features US Medical PG Question 8: A 26-year-old female college student is brought back into the university clinic for acting uncharacteristically. The patient presented to the same clinic 6 weeks ago with complaints of depressed mood, insomnia, and weightloss. She had been feeling guilty for wasting her parent’s money by doing so poorly at the university. She felt drained for at least 2 weeks before presenting to the clinic for the first time. She was placed on an antidepressant and was improving but now presents with elevated mood. She is more talkative with a flight of ideas and is easily distractible. Which of the following statements is most likely true regarding this patient’s condition?
- A. The patient may have psychotic features.
- B. Her diagnosis of unipolar depression is incorrect. (Correct Answer)
- C. The patient may have a history of mania.
- D. Antidepressants are inappropriate.
- E. Her new symptoms need to last at least 7 days.
Manic episode criteria and features Explanation: ***Correct: Her diagnosis of unipolar depression is incorrect.***
The patient initially presented with symptoms consistent with a **depressive episode**, but the subsequent emergence of **elevated mood, increased talkativeness, flight of ideas, and distractibility after antidepressant use** strongly suggests a shift to a **manic or hypomanic episode**. This antidepressant-induced mood switch is a hallmark feature revealing **bipolar disorder** that was initially misdiagnosed as unipolar depression. This statement most directly addresses **what is true about this patient's condition** - that the fundamental diagnosis is incorrect. Once we establish the correct diagnosis of bipolar disorder, all treatment and management decisions follow from this.
*Incorrect: The patient may have psychotic features.*
While patients with severe **mania** can develop **psychotic features** (e.g., delusions, hallucinations), the provided symptoms (elevated mood, increased talkativeness, flight of ideas, distractibility) do not describe psychotic symptoms. There is no information suggesting the presence of **delusions or hallucinations**, which are necessary to diagnose psychotic features. The word "may" makes this theoretically possible but not supported by the clinical presentation described.
*Incorrect: The patient may have a history of mania.*
While patients with bipolar disorder often have previous undiagnosed episodes, this statement is speculative about her **past history** rather than addressing what is most directly evident from the **current presentation**. The vignette focuses on the antidepressant-induced mood switch, which immediately reveals that the current diagnosis of unipolar depression is incorrect. Whether or not she had previous manic episodes is less relevant than recognizing the misdiagnosis now.
*Incorrect: Antidepressants are inappropriate.*
This statement is clinically **true in principle** - antidepressants as monotherapy are generally inappropriate for bipolar disorder due to the risk of inducing mania or hypomania. However, this option addresses **treatment implications** rather than directly stating what is true about **the patient's condition itself**. The more fundamental and direct truth is that **her diagnosis is wrong** (bipolar, not unipolar depression). Once the correct diagnosis is established, then the inappropriateness of antidepressant monotherapy follows. Additionally, at the time of initial presentation with pure depressive symptoms, the antidepressant prescription was reasonable based on the information available - the inappropriateness only became clear retrospectively after the mood switch occurred.
*Incorrect: Her new symptoms need to last at least 7 days.*
For a diagnosis of **mania**, symptoms must last at least **one week** (or any duration if hospitalization is required). However, for **hypomania**, symptoms need to last only **4 consecutive days**. The vignette does not specify whether this is mania or hypomania, nor does it clearly state the duration of the current symptoms beyond "now presents." Therefore, we cannot definitively say a 7-day duration is required - it could be hypomania requiring only 4 days. This statement is not necessarily true.
Manic episode criteria and features US Medical PG Question 9: An 11-year-old boy’s parents brought him to a psychologist upon referral from the boy’s school teacher. The boy frequently bullies his younger classmates despite having been punished several times for this. His mother also reported that a year prior, she received complaints that the boy shoplifted from local shops in his neighborhood. The boy frequently stays out at night despite strict instructions by his parents to return home by 10 PM. Detailed history reveals that apart from such behavior, he is usually not angry or irritable. Although his abnormal behavior continues despite warnings and punishments, he neither argues with his parents nor teachers and does not display verbal or physical aggression. Which of the following is the most likely diagnosis?
- A. Attention-deficit/hyperactivity disorder, hyperactivity-impulsivity type
- B. Disruptive mood dysregulation disorder
- C. Intermittent explosive disorder
- D. Conduct disorder (Correct Answer)
- E. Oppositional defiant disorder
Manic episode criteria and features Explanation: ***Conduct disorder***
- The boy's behaviors, including **bullying**, **shoplifting**, and **violating rules** (staying out past curfew), represent a persistent pattern of behavior that violates the basic rights of others or major age-appropriate societal norms, which are core features of **conduct disorder**.
- The history indicates these behaviors have been ongoing for at least a year and are not just isolated incidents, fulfilling the diagnostic criteria for **duration and pervasiveness**.
*Attention-deficit/hyperactivity disorder, hyperactivity-impulsivity type*
- While ADHD involves **hyperactivity** and **impulsivity**, it does not typically manifest with deliberate violations of others' rights or societal norms like **bullying** and **shoplifting**.
- There is no mention of symptoms such as **difficulty sustaining attention**, **fidgeting**, or **excessive talking** which are characteristic of ADHD.
*Disruptive mood dysregulation disorder*
- This disorder is characterized by **severe recurrent temper outbursts** and persistent **irritable or angry mood** between outbursts.
- The case explicitly states the boy is "not angry or irritable" and "neither argues with his parents nor teachers," ruling out this diagnosis.
*Intermittent explosive disorder*
- This disorder involves recurrent behavioral outbursts representing a failure to control aggressive impulses, often with verbal aggression or physical aggression toward property, animals, or other individuals.
- The boy does not display verbal or physical aggression and is not noted to have anger or irritability, which are central to this diagnosis.
*Oppositional defiant disorder*
- ODD involves a pattern of **angry/irritable mood**, **argumentative/defiant behavior**, or **vindictiveness**.
- While violating rules is present, **bullying** and **shoplifting** (which violate the basic rights of others) are more severe behaviors that go beyond the scope of ODD and are characteristic of conduct disorder.
Manic episode criteria and features US Medical PG Question 10: A 25-year-old woman is brought to a psychiatrist's office by her husband who states that he is worried about her recent behavior, as it has become more violent. The patient's husband states that his family drove across the country to visit them and that his wife 'threatened his parents with a knife' at dinner last night. Police had to be called to calm her down. He states that she has been acting 'really crazy' for the last 9 months, and the initial behavior that caused him alarm was her admission that his deceased sister was talking to her through a decorative piece of ceramic art in the living room. Initially, he thought she was joking, but soon realized her complaints of 'hearing ghosts' talking to her throughout the house were persisting and 'getting worse'. Over the past 9 months, she has experienced multiple periods of profound sadness, with persistent insomnia and an unintentional weight loss of 12 pounds over several months. She has been complaining of feeling 'worthless' and has had markedly diminished interest in activities for much of this time period. Her general hygiene has also suffered from her recent lack of motivation and she insists that the 'ghosts' are asking her to kill as many people as she can so they won't be alone in the house. Her husband is extremely concerned that she may harm herself or someone else. He states that she currently does not take any medications or illicit drugs as far as he knows. She does not smoke or drink alcohol. The patient herself does not make eye contact or want to speak to the psychiatrist, allowing her husband to speak on her behalf. Which of the following is the most likely diagnosis in this patient?
- A. Schizophreniform disorder
- B. Schizophrenia
- C. Delusional disorder
- D. Schizoaffective disorder (Correct Answer)
- E. Brief psychotic disorder
Manic episode criteria and features Explanation: ***Schizoaffective disorder***
- This patient exhibits symptoms of both a **major depressive disorder** (multiple periods of profound **sadness**, persistent **insomnia**, **weight loss** over several months, feelings of **worthlessness**, and markedly **diminished interest in activities**) and a **psychotic disorder** (auditory **hallucinations**, command hallucinations, **delusions**, violent behavior).
- The total symptom duration is **9 months**, with **mood symptoms present for the majority of this period**, meeting the key DSM-5 criterion for schizoaffective disorder.
- The patient also demonstrates **psychotic symptoms (hallucinations) that persist throughout**, including periods when mood symptoms may fluctuate, satisfying the requirement for delusions or hallucinations for ≥2 weeks in the absence of a major mood episode.
- The combination of prominent mood episodes concurrent with schizophrenia-spectrum symptoms, with mood symptoms present for the majority of the illness duration, confirms schizoaffective disorder.
*Schizophreniform disorder*
- This disorder involves symptoms characteristic of **schizophrenia** lasting **between 1 and 6 months**.
- The patient's symptoms have been present for **9 months**, exceeding the maximum duration for schizophreniform disorder.
*Schizophrenia*
- Schizophrenia requires persistent psychotic symptoms lasting **at least 6 months**, with at least one month of active-phase symptoms.
- While this patient has psychotic symptoms for 9 months, the **prominent and prolonged depressive symptoms** that are present for the **majority of the illness duration** distinguish this from schizophrenia.
- In schizophrenia, mood symptoms, if present, are **brief relative to the total duration** of the psychotic illness, which is not the case here.
*Delusional disorder*
- Delusional disorder is characterized by **non-bizarre delusions** for at least 1 month, without other prominent psychotic symptoms.
- This patient experiences prominent **auditory hallucinations** ("hearing ghosts," "deceased sister talking to her") and **command hallucinations**, which are not features of delusional disorder.
- The presence of hallucinations rules out this diagnosis.
*Brief psychotic disorder*
- This diagnosis involves sudden onset of psychotic symptoms lasting **more than 1 day but less than 1 month**, with eventual full recovery.
- The patient's symptoms have persisted for **9 months**, far exceeding the duration criterion for brief psychotic disorder.
More Manic episode criteria and features US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.