Antipsychotics in bipolar disorder US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antipsychotics in bipolar disorder. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antipsychotics in bipolar disorder US Medical PG Question 1: A 35-year-old man is brought to the emergency department by his wife. She was called by his coworkers to come and pick him up from work after he barged into the company’s board meeting and was being very disruptive as he ranted on about all the great ideas he had for the company. When they tried to reason with him, he became hostile and insisted that he should be the CEO as he knew what was best for the future of the company. The patient’s wife also noted that her husband has been up all night for the past few days but assumed that he was handling a big project at work. The patient has no significant past medical or psychiatric history. Which of the following treatments is most likely to benefit this patient’s condition?
- A. Antidepressants
- B. Valproic acid (Correct Answer)
- C. Haloperidol
- D. Psychotherapy
- E. Clozapine
Antipsychotics in bipolar disorder Explanation: ***Valproic acid***
- This patient presents with symptoms highly suggestive of a **manic episode**, including grandiosity (believing he should be CEO), decreased need for sleep (up all night for days), pressured speech (ranting), and impulsivity with poor judgment (disruptive behavior at a board meeting).
- **Valproic acid** is a **first-line, guideline-recommended mood stabilizer** for acute mania. It is particularly effective for managing the core symptoms of mania including mood elevation, irritability, and impulsivity.
- It has a relatively rapid onset of action and a favorable side effect profile compared to typical antipsychotics, making it an excellent choice for initial management of acute mania in the emergency setting.
*Antidepressants*
- Administering **antidepressants** during a manic or hypomanic episode can exacerbate symptoms, potentially leading to a rapid cycling pattern or worsening mania.
- Antidepressants are primarily used for depressive episodes in bipolar disorder, typically in conjunction with a mood stabilizer, never as monotherapy in a patient presenting with mania.
*Haloperidol*
- **Haloperidol** is a typical antipsychotic that can be used for acute agitation in mania, but it does not address the underlying mood dysregulation.
- While it may help with immediate behavioral control, mood stabilizers like valproic acid or lithium are preferred as primary treatments because they target the core pathophysiology of bipolar disorder.
- Haloperidol also has a higher risk of extrapyramidal symptoms and does not prevent future mood episodes.
*Psychotherapy*
- **Psychotherapy** is a crucial component of long-term management for bipolar disorder but is not effective as a sole treatment for acute mania.
- Patients in acute mania are often too agitated, impulsive, and lack sufficient insight to meaningfully engage in therapeutic interventions.
- Psychotherapy should be initiated after mood stabilization with pharmacotherapy.
*Clozapine*
- **Clozapine** is an atypical antipsychotic reserved for treatment-resistant schizophrenia or treatment-resistant bipolar disorder, particularly with prominent psychotic features that have not responded to multiple other medications.
- Given its significant side effect profile, including agranulocytosis requiring regular blood monitoring, it is not a first-line or even second-line treatment for an initial presentation of mania.
- This patient has no psychiatric history and requires standard first-line treatment, not a medication reserved for refractory cases.
Antipsychotics in bipolar disorder US Medical PG Question 2: A 22-year-old male with a history of difficult-to-treat bipolar disorder with psychotic features is undergoing a medication adjustment under the guidance of his psychiatrist. The patient was previously treated with lithium and is transitioning to clozapine. Which of the following tests will the patient need routinely?
- A. Thyroid-stimulating hormone, prior to introducing the medication
- B. Basic metabolic panel, weekly
- C. Hemoglobin A1c, weekly
- D. Dexamethasone suppression test, monthly
- E. Complete blood count, weekly (Correct Answer)
Antipsychotics in bipolar disorder Explanation: ***Complete blood count, weekly***
- **Clozapine** can cause **agranulocytosis** (a severe drop in white blood cell count), which is a potentially life-threatening side effect.
- Due to this risk, initial treatment with clozapine requires **weekly complete blood count (CBC)** monitoring to detect early signs of agranulocytosis.
*Thyroid-stimulating hormone, prior to introducing the medication*
- While initial thyroid function tests might be considered in the workup for bipolar disorder, routine and specific monitoring of **TSH** is not a primary requirement for **clozapine** initiation.
- **Lithium**, not clozapine, is more directly associated with thyroid dysfunction, so monitoring would be more relevant to the patient's previous medication.
*Basic metabolic panel, weekly*
- A **basic metabolic panel (BMP)** assesses **electrolyte levels**, **kidney function**, and **glucose**, which can be affected by various psychotropic medications.
- While important for overall health monitoring, a **weekly BMP** is not specifically mandated for **clozapine** due to the specific and severe risk of agranulocytosis.
*Hemoglobin A1c, weekly*
- **Clozapine** is associated with a risk of **metabolic side effects**, including **weight gain**, **dyslipidemia**, and **new-onset diabetes**.
- While **HbA1c** is used to monitor long-term glycemic control, it's typically checked less frequently (e.g., quarterly or annually) for metabolic monitoring, not weekly, and is not the primary immediate safety concern for clozapine.
*Dexamethasone suppression test, monthly*
- The **dexamethasone suppression test (DST)** is used to assess **adrenal gland function** and can be relevant in certain psychiatric conditions like **depression with melancholic features** or to rule out **Cushing's syndrome**.
- It is **not a routine monitoring test** for patients starting or on **clozapine** therapy.
Antipsychotics in bipolar disorder US Medical PG Question 3: A 45-year-old obese man is evaluated in a locked psychiatric facility. He was admitted to the unit after he was caught running through traffic naked while tearing out his hair. His urine toxicology screening was negative for illicit substances and after careful evaluation and additional history, provided by his parents, he was diagnosed with schizophrenia and was treated with aripiprazole. His symptoms did not improve after several dosage adjustments and he was placed on haloperidol, but this left him too lethargic and slow and he was placed on loxapine. After several dosage adjustments today, he is still quite confused. He describes giant spiders and robots that torture him in his room. He describes an incessant voice screaming at him to run away. He also strongly dislikes his current medication and would like to try something else. Which of the following is indicated in this patient?
- A. Haloperidol
- B. Olanzapine
- C. Chlorpromazine
- D. Fluphenazine
- E. Clozapine (Correct Answer)
Antipsychotics in bipolar disorder Explanation: ***Clozapine***
- This patient has **treatment-resistant schizophrenia**, indicated by a lack of response to multiple trials of antipsychotics, including aripiprazole (atypical), haloperidol (typical), and loxapine (atypical).
- **Clozapine** is the only antipsychotic proven effective for treatment-resistant schizophrenia, significantly reducing psychotic symptoms and suicidality.
*Haloperidol*
- Haloperidol is a **first-generation antipsychotic** that the patient has already tried and found to be too sedating and slow.
- Continuing with haloperidol would likely result in persistent side effects and inadequate symptom control given his prior negative experience.
*Olanzapine*
- Olanzapine is a **second-generation atypical antipsychotic**; however, it is not typically indicated as a first-line treatment for treatment-resistant schizophrenia after failure of multiple agents.
- While effective for schizophrenia, it would be less effective than clozapine in a patient who has failed several previous antipsychotic trials.
*Chlorpromazine*
- Chlorpromazine is a **first-generation antipsychotic** that carries a higher risk of sedation, extrapyramidal symptoms, and anticholinergic side effects.
- It is unlikely to be more effective than haloperidol, which the patient already found too sedating and slow, and would not be the preferred choice for treatment-resistant schizophrenia.
*Fluphenazine*
- Fluphenazine is a **first-generation antipsychotic** with potent dopamine D2 receptor blockade, often leading to significant extrapyramidal side effects.
- Like other first-generation antipsychotics, it is not indicated as the next step for treatment-resistant schizophrenia after failure of multiple trials.
Antipsychotics in bipolar disorder US Medical PG Question 4: A 35-year-old woman comes to the physician accompanied by her husband after he started noticing strange behavior. He first noticed her talking to herself 8 months ago. For the past 6 months, she has refused to eat any packaged foods out of fear that the government is trying to poison her. She has no significant past medical history. She smoked marijuana in college but has not smoked any since. She appears restless. Mental status examination shows a flat affect. Her speech is clear, but her thought process is disorganized with many loose associations. The patient is diagnosed with schizophrenia and started on olanzapine. This patient is most likely to experience which of the following adverse effects?
- A. Dyslipidemia (Correct Answer)
- B. Diabetes insipidus
- C. Agranulocytosis
- D. Myoglobinuria
- E. Seizures
Antipsychotics in bipolar disorder Explanation: ***Dyslipidemia***
- **Olanzapine** is a **second-generation antipsychotic** commonly associated with significant **metabolic side effects**, including **weight gain**, **dyslipidemia**, and **insulin resistance**.
- These metabolic disturbances increase the risk of cardiovascular disease.
*Diabetes insipidus*
- This is a rare side effect, not typically associated with **olanzapine** or other **second-generation antipsychotics**.
- **Lithium** is an antimanic agent that can cause **nephrogenic diabetes insipidus**, but it is not relevant here.
*Agranulocytosis*
- While a serious side effect of some antipsychotics, **agranulocytosis** is most notably associated with **clozapine**,
- **Olanzapine** has a much lower risk of causing **agranulocytosis** compared to clozapine.
*Myoglobinuria*
- **Myoglobinuria** is associated with conditions like significant muscle damage (e.g., rhabdomyolysis).
- It is not a direct or common adverse effect of **olanzapine** therapy.
*Seizures*
- While some antipsychotics can lower the **seizure threshold**, **olanzapine** generally has a relatively low risk of inducing seizures.
- The risk is higher with certain other antipsychotics, particularly at high doses, or in patients with pre-existing seizure disorders.
Antipsychotics in bipolar disorder US Medical PG Question 5: A 24-year-old man with a history of schizophrenia presents for follow-up. The patient says that he is still having paranoia and visual hallucinations on his latest atypical antipsychotic medication. Past medical history is significant for schizophrenia diagnosed 1 year ago that failed to be adequately controlled on 2 separate atypical antipsychotic medications. The patient is switched to a typical antipsychotic medication. Which of the following is the mechanism of action of the medication that was most likely prescribed for this patient?
- A. Dopaminergic receptor antagonist (Correct Answer)
- B. Dopaminergic partial agonist
- C. Serotonergic receptor agonist
- D. Serotonergic receptor antagonist
- E. Cholinergic receptor agonist
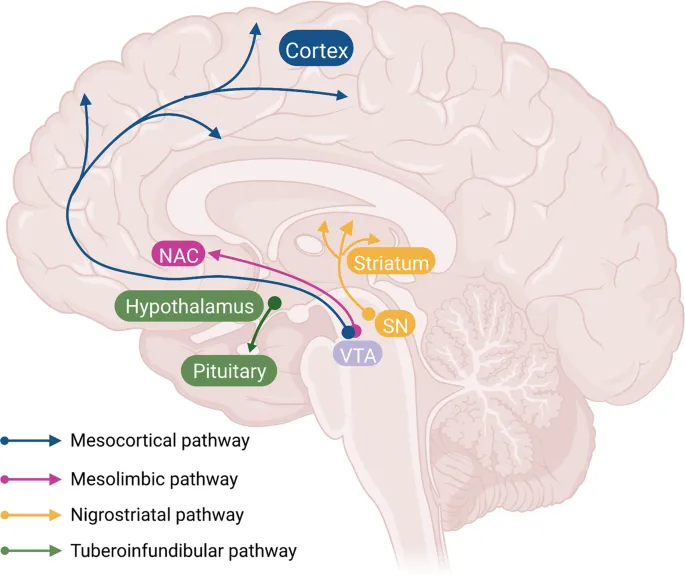
Antipsychotics in bipolar disorder Explanation: ***Dopaminergic receptor antagonist***
- The patient has **treatment-resistant schizophrenia**, indicated by failure to respond to two different atypical antipsychotics.
- Typical antipsychotics like **haloperidol** or **fluphenazine** are primarily **D2 dopamine receptor antagonists**, which may be used when a patient has not responded to atypical agents.
- The **primary mechanism** of typical (first-generation) antipsychotics is **potent D2 receptor blockade** in the mesolimbic pathway, which reduces positive symptoms of schizophrenia.
- Note: Clozapine would be the preferred choice for true treatment-resistant schizophrenia, but typical antipsychotics may still be considered in some clinical scenarios.
*Dopaminergic partial agonist*
- **Dopamine partial agonists**, such as **aripiprazole** or **brexpiprazole**, are **atypical antipsychotics** used for schizophrenia.
- The patient has failed to respond to atypical antipsychotics already, making it unlikely that another atypical agent would be the next choice.
- The question specifically states the patient is switched to a **typical antipsychotic**.
*Serotonergic receptor agonist*
- **Serotonin receptor agonists**, like LSD or psilocybin, are **not used** in the treatment of schizophrenia; they can, in fact, **induce psychotic symptoms**.
- While some antipsychotics modulate serotonin receptors, their therapeutic effect is not through agonism of these receptors.
*Serotonergic receptor antagonist*
- Many **atypical antipsychotics** have significant **serotonin 5-HT2A receptor antagonist** activity, in addition to D2 antagonism.
- However, the question states that the patient is being switched to a **typical antipsychotic**, whose primary and defining mechanism is **D2 antagonism**, not combined serotonin-dopamine antagonism.
*Cholinergic receptor agonist*
- **Cholinergic receptor agonists** are **not used** to treat schizophrenia and would likely worsen symptoms or cause significant side effects.
- These agents would have no therapeutic benefit in psychosis and are not part of the antipsychotic drug class.
Antipsychotics in bipolar disorder US Medical PG Question 6: A 23-year-old college student presents with his parents for a follow-up appointment. He was recently diagnosed with schizophrenia and was started on risperidone approx. 2 months ago. He reports a significant improvement since the start of treatment. His parents report that their son’s symptoms of delusions, hallucinations, and paranoid behavior have been ameliorated. On physical examination, the patient seems uncomfortable. He frequently fidgets and repeatedly crosses and uncrosses his legs. When asked if something is troubling him, he gets up and starts pacing. He says, “It’s always like this. I cannot sit still. It is frustrating.” What is the most likely diagnosis?
- A. Generalized anxiety disorder
- B. Tardive dyskinesia
- C. Ataxia
- D. Akathisia (Correct Answer)
- E. Restless legs syndrome
Antipsychotics in bipolar disorder Explanation: ***Akathisia***
- This patient presents with **motor restlessness** (fidgeting, pacing, inability to sit still) that emerged after starting an antipsychotic medication, risperidone. These are classic symptoms of **akathisia**, a medication side effect.
- The patient's verbalization, "I cannot sit still. It is frustrating," further supports the internal experience of restlessness characteristic of akathisia.
*Generalized anxiety disorder*
- While anxiety can cause restlessness, the specific description of physical agitation and the strong temporal relationship with starting a new antipsychotic make **akathisia** a more likely diagnosis.
- Generalized anxiety disorder typically involves chronic, excessive worry and is not primarily characterized by an irresistible urge to move.
*Tardive dyskinesia*
- Tardive dyskinesia involves **involuntary, repetitive body movements**, often in the face (e.g., grimacing, tongue protrusion) or limbs.
- It usually develops after **long-term use** of antipsychotics (months to years), whereas akathisia can occur shortly after initiation or dose changes.
*Ataxia*
- Ataxia refers to a lack of **voluntary coordination** of muscle movements, leading to an unsteady gait or impaired balance.
- The patient's symptoms are of restlessness and an uncontrollable urge to move, not a lack of coordination.
*Restless legs syndrome*
- Restless legs syndrome is characterized by an **uncomfortable sensation in the legs** with an urge to move them, typically worse at rest and relieved by movement.
- This patient's restlessness is more pervasive, involving whole-body agitation and an inability to simply sit still, not just an uncomfortable sensation primarily in the legs.
Antipsychotics in bipolar disorder US Medical PG Question 7: A 34-year-old woman presents with recurrent panic attacks that have been worsening over the past 5 weeks. She also says she has been seeing things that are not present in reality and is significantly bothered by a short attention span which has badly affected her job in the past 6 months. No significant past medical history. No current medications. The patient is afebrile and vital signs are within normal limits. Her BMI is 34 kg/m2. Physical examination is unremarkable. The patient is prescribed antipsychotic medication. She expresses concerns about any effects of the new medication on her weight. Which of the following medications would be the best course of treatment in this patient?
- A. Ziprasidone (Correct Answer)
- B. Clozapine
- C. Chlorpromazine
- D. Olanzapine
- E. Clonazepam
Antipsychotics in bipolar disorder Explanation: ***Ziprasidone***
- **Ziprasidone** causes minimal **weight gain** and has a lower risk of metabolic side effects compared to other antipsychotics, making it a good choice for a patient concerned about weight, especially with a BMI of 34 kg/m2.
- It treats psychotic symptoms like hallucinations and can help manage anxiety associated with panic attacks.
*Clozapine*
- **Clozapine** is known for causing significant **weight gain** and metabolic disturbances, which would be a concern for this patient.
- It is typically reserved for treatment-resistant schizophrenia due to its potential for serious side effects like **agranulocytosis**.
*Chlorpromazine*
- **Chlorpromazine** is a first-generation antipsychotic associated with a high risk of **extrapyramidal symptoms** (EPS) and sedation.
- It can also lead to moderate **weight gain** and is generally not preferred as a first-line treatment if metabolic concerns are present.
*Olanzapine*
- **Olanzapine** is associated with a high risk of **weight gain** and metabolic syndrome, which would exacerbate the patient's existing weight concerns.
- While effective for psychosis, its metabolic side effect profile makes it a less suitable choice in this scenario.
*Clonazepam*
- **Clonazepam** is a **benzodiazepine** primarily used for anxiety and panic attacks, but it is not an antipsychotic.
- It would not address the patient's psychotic symptoms (seeing things not present in reality), which require an antipsychotic medication.
Antipsychotics in bipolar disorder US Medical PG Question 8: A 30-year-old man presents to his psychiatrist for a follow-up visit. He was diagnosed with schizophrenia 6 months ago and has been taking fluphenazine. He says that his symptoms are well controlled by the medication, and he no longer has auditory hallucinations. The psychiatrist also notes that his delusions and other psychotic symptoms have improved significantly. However, the psychiatrist notices something while talking to the patient that prompts him to say, “I know the drug has effectively controlled your symptoms but I think you should discontinue it now otherwise this side effect is likely to be irreversible.” Which of the following did the psychiatrist most likely notice in this patient?
- A. Choreoathetoid movements of face (Correct Answer)
- B. Crossing and uncrossing legs constantly
- C. Involuntary sustained twisting of neck
- D. Resting tremors
- E. Reduced spontaneous movements while walking
Antipsychotics in bipolar disorder Explanation: ***Choreoathetoid movements of face***
- The psychiatrist is concerned about **tardive dyskinesia (TD)**, a late-onset side effect of dopamine receptor blocking agents like fluphenazine. Its hallmark symptoms include **choreoathetoid (involuntary, jerky, writhing) movements**, often affecting the face (e.g., lip smacking, grimacing, tongue protrusion).
- TD can become **irreversible** if the offending medication is continued, necessitating drug discontinuation to prevent permanent motor dysfunction.
*Reduced spontaneous movements while walking*
- This symptom, along with a "shuffling gait" and **bradykinesia**, is characteristic of drug-induced **Parkinsonism**.
- While concerning, Parkinsonism is generally **reversible** upon dose reduction or discontinuation of the antipsychotic, or with the addition of anticholinergic agents, making the psychiatrist's urgent warning about irreversibility less likely for this specific side effect.
*Crossing and uncrossing legs constantly*
- This behavior is indicative of **akathisia**, an inner sense of restlessness that manifests as an inability to sit still.
- Akathisia is a common extrapyramidal side effect that is typically **reversible** with dose reduction, medication change, or treatment with beta-blockers, and is not usually considered irreversible like tardive dyskinesia.
*Involuntary sustained twisting of neck*
- This describes **dystonia**, an extrapyramidal side effect characterized by sustained or repetitive muscle contractions leading to abnormal postures, such as **torticollis** (twisting of the neck).
- Dystonia, while distressing, is usually **reversible** with acute treatment (e.g., anticholinergics like benztropine) and medication adjustment, rarely becoming irreversible.
*Resting tremors*
- **Resting tremors** are a feature of drug-induced **Parkinsonism**, often accompanied by rigidity and bradykinesia.
- Similar to other Parkinsonian symptoms, these tremors are generally **reversible** with appropriate medication management and are not typically considered an irreversible side effect if the offending drug is discontinued promptly.
Antipsychotics in bipolar disorder US Medical PG Question 9: A 19-year-old female college student is brought into the emergency department by her boyfriend. The boyfriend reports that the patient got caught stealing from the company she works for and subsequently got fired. The boyfriend received a text that evening saying “I’ll miss you.” When he arrived at her dorm room, the patient was slumped in the shower covered in blood. The patient agreed to be driven to the emergency room. When asked about what happened, the patient replies “I just want out of this life.” The patient has bipolar disorder, and takes lithium as prescribed. She has a psychiatrist she sees every week, which the boyfriend confirms. She has never had a prior suicide attempt nor has she ever been hospitalized for a psychiatric disorder. The patient’s vitals are stable. Upon physical examination, a 4 centimeter vertical incision is noted on the patient’s left forearm. During the patient’s laceration repair, she asks if she will be admitted. She states, “these ups and downs are common for me, but I feel better now.” She verbalizes that she understands that she overreacted. She asks to go home, and her boyfriend insists that he will stay with her. They both confirm that neither of them have guns or know any peers with access to guns. Which of the following is the most appropriate management for the patient?
- A. Have the patient sign a suicide contract before discharge
- B. Set up a next-day appointment with the patient’s psychiatrist
- C. Involuntarily admit the patient (Correct Answer)
- D. Call the patient’s parents
- E. Discontinue lithium and start valproate
Antipsychotics in bipolar disorder Explanation: ***Involuntarily admit the patient***
- The patient's statement "I just want out of this life" combined with the **suicide attempt** (cutting her forearm after a text expressing suicidal ideation) indicates a high risk of self-harm. Despite her current verbalizations of feeling better, the **impulsivity** and severity of the attempt warrant involuntary admission for safety.
- The sudden shift in mood and desire to go home after a serious suicide attempt, stating "these ups and downs are common for me, but I feel better now," suggests potential **lability** and a continued risk that cannot be safely managed with outpatient follow-up alone.
*Have the patient sign a suicide contract before discharge*
- **Suicide contracts** have not been consistently shown to be effective in preventing suicide and can create a false sense of security.
- Given the **actual suicide attempt** and the patient's underlying psychiatric condition, a contract is insufficient to ensure her safety.
*Set up a next-day appointment with the patient’s psychiatrist*
- While follow-up with her psychiatrist is crucial, relying solely on a **next-day appointment** is inadequate given the acute and severe nature of the suicide attempt.
- There is a significant risk of another attempt before the appointment, and the patient needs the **structured environment and constant observation** of an inpatient setting.
*Call the patient’s parents*
- While involving the patient's support system is generally helpful, this action does not directly address the immediate **safety risk** posed by the recent suicide attempt.
- Parental involvement should be considered, but it is not the primary or most appropriate immediate management for a patient at **high risk of self-harm**.
*Discontinue lithium and start valproate*
- Modifying psychotropic medication is a decision made by a psychiatrist after a thorough evaluation, often over time, and is not the immediate or most appropriate "management" in the **emergency setting** for an acute suicide attempt.
- The priority is **safety and stabilization**, not an immediate medication change, especially given that she is already on a mood stabilizer.
Antipsychotics in bipolar disorder US Medical PG Question 10: A 26-year-old female college student is brought back into the university clinic for acting uncharacteristically. The patient presented to the same clinic 6 weeks ago with complaints of depressed mood, insomnia, and weightloss. She had been feeling guilty for wasting her parent’s money by doing so poorly at the university. She felt drained for at least 2 weeks before presenting to the clinic for the first time. She was placed on an antidepressant and was improving but now presents with elevated mood. She is more talkative with a flight of ideas and is easily distractible. Which of the following statements is most likely true regarding this patient’s condition?
- A. The patient may have psychotic features.
- B. Her diagnosis of unipolar depression is incorrect. (Correct Answer)
- C. The patient may have a history of mania.
- D. Antidepressants are inappropriate.
- E. Her new symptoms need to last at least 7 days.
Antipsychotics in bipolar disorder Explanation: ***Correct: Her diagnosis of unipolar depression is incorrect.***
The patient initially presented with symptoms consistent with a **depressive episode**, but the subsequent emergence of **elevated mood, increased talkativeness, flight of ideas, and distractibility after antidepressant use** strongly suggests a shift to a **manic or hypomanic episode**. This antidepressant-induced mood switch is a hallmark feature revealing **bipolar disorder** that was initially misdiagnosed as unipolar depression. This statement most directly addresses **what is true about this patient's condition** - that the fundamental diagnosis is incorrect. Once we establish the correct diagnosis of bipolar disorder, all treatment and management decisions follow from this.
*Incorrect: The patient may have psychotic features.*
While patients with severe **mania** can develop **psychotic features** (e.g., delusions, hallucinations), the provided symptoms (elevated mood, increased talkativeness, flight of ideas, distractibility) do not describe psychotic symptoms. There is no information suggesting the presence of **delusions or hallucinations**, which are necessary to diagnose psychotic features. The word "may" makes this theoretically possible but not supported by the clinical presentation described.
*Incorrect: The patient may have a history of mania.*
While patients with bipolar disorder often have previous undiagnosed episodes, this statement is speculative about her **past history** rather than addressing what is most directly evident from the **current presentation**. The vignette focuses on the antidepressant-induced mood switch, which immediately reveals that the current diagnosis of unipolar depression is incorrect. Whether or not she had previous manic episodes is less relevant than recognizing the misdiagnosis now.
*Incorrect: Antidepressants are inappropriate.*
This statement is clinically **true in principle** - antidepressants as monotherapy are generally inappropriate for bipolar disorder due to the risk of inducing mania or hypomania. However, this option addresses **treatment implications** rather than directly stating what is true about **the patient's condition itself**. The more fundamental and direct truth is that **her diagnosis is wrong** (bipolar, not unipolar depression). Once the correct diagnosis is established, then the inappropriateness of antidepressant monotherapy follows. Additionally, at the time of initial presentation with pure depressive symptoms, the antidepressant prescription was reasonable based on the information available - the inappropriateness only became clear retrospectively after the mood switch occurred.
*Incorrect: Her new symptoms need to last at least 7 days.*
For a diagnosis of **mania**, symptoms must last at least **one week** (or any duration if hospitalization is required). However, for **hypomania**, symptoms need to last only **4 consecutive days**. The vignette does not specify whether this is mania or hypomania, nor does it clearly state the duration of the current symptoms beyond "now presents." Therefore, we cannot definitively say a 7-day duration is required - it could be hypomania requiring only 4 days. This statement is not necessarily true.
More Antipsychotics in bipolar disorder US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.