Bipolar disorder

On this page
🧠 The Bipolar Spectrum: Decoding Mood's Electrical Storm
Bipolar disorder transforms the brain into a battleground where electrical storms of mania clash with depressive undertows, creating one of psychiatry's most dramatic yet treatable conditions. You'll learn to distinguish the full spectrum from explosive mania to subtle hypomania, master evidence-based treatment algorithms that stabilize these dangerous oscillations, and navigate the complex web of comorbidities that often obscure diagnosis. This lesson builds your clinical eye for recognizing mood's electrical signatures and your therapeutic precision in restoring neurochemical balance.
📌 Remember: DIGFAST for manic episodes - Distractibility, Irresponsibility, Grandiosity, Flight of ideas, Activity increase, Sleep decrease, Talkativeness. Each symptom must persist ≥1 week (or require hospitalization) with ≥3 symptoms present during mood disturbance.
The bipolar spectrum encompasses multiple distinct disorders with precise diagnostic thresholds. Bipolar I requires ≥1 manic episode lasting ≥7 days with severe functional impairment. Bipolar II demands ≥1 hypomanic episode (4-6 days) plus ≥1 major depressive episode, but never full mania. Cyclothymic disorder involves ≥2 years of hypomanic and depressive periods without meeting full episode criteria.
| Disorder Type | Manic Episodes | Hypomanic Episodes | Depressive Episodes | Duration Requirement | Functional Impairment |
|---|---|---|---|---|---|
| Bipolar I | ≥1 required | May occur | May occur | ≥7 days | Severe/hospitalization |
| Bipolar II | Never | ≥1 required | ≥1 required | 4-6 days hypo | Mild-moderate |
| Cyclothymic | Never | Subsyndromal | Subsyndromal | ≥2 years | Variable |
| Substance-Induced | Variable | Variable | Variable | During intoxication | Substance-related |
| Medical Condition | Variable | Variable | Variable | Physiological consequence | Medical etiology |
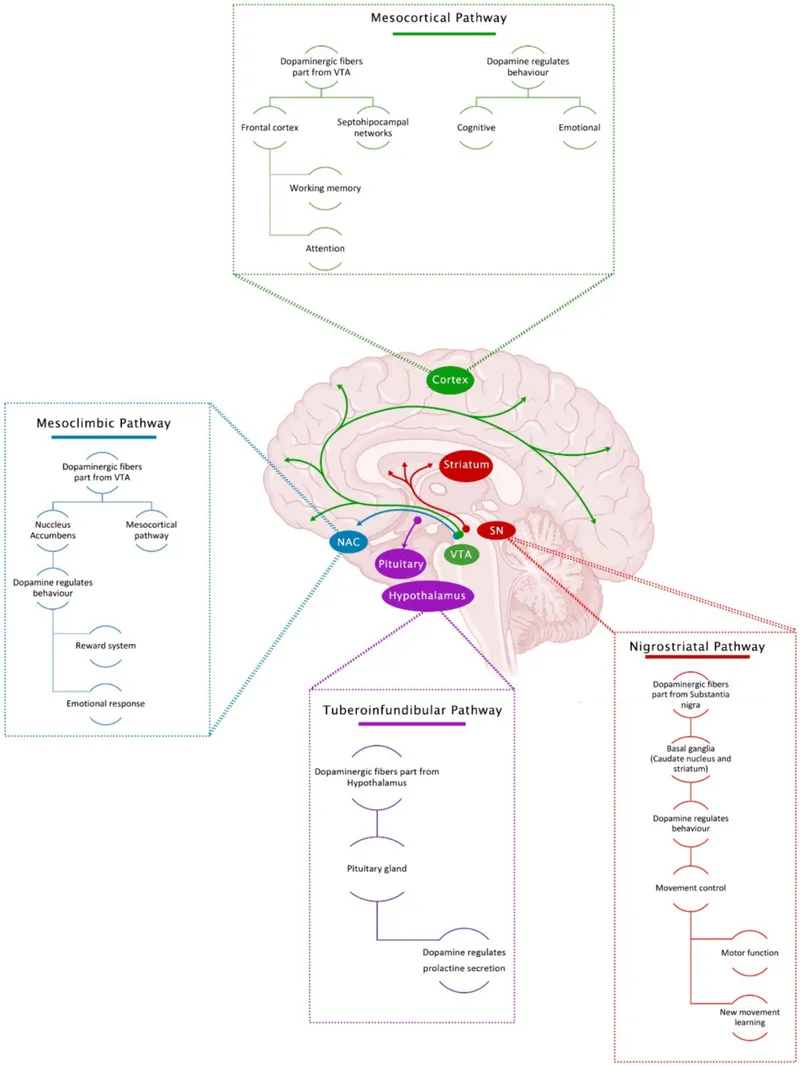
The neurobiological foundation involves dysregulated monoamine systems - particularly dopamine, norepinephrine, and serotonin circuits. Genetic heritability reaches 85%, with first-degree relatives carrying 10-fold increased risk. Neuroimaging reveals enlarged lateral ventricles, reduced prefrontal cortex volume, and hyperactive amygdala during mood episodes.
💡 Master This: Bipolar disorder isn't episodic mood changes - it's chronic brain circuit dysfunction requiring lifelong management. Early recognition and mood stabilizer initiation can prevent progressive brain changes and reduce episode frequency by 60-80%.
Understanding bipolar's complexity transforms clinical assessment from symptom checklists into sophisticated pattern recognition, enabling precise diagnosis and targeted interventions that can dramatically alter disease trajectory.
🧠 The Bipolar Spectrum: Decoding Mood's Electrical Storm
⚡ Manic Episodes: The Brain's Electrical Overdrive
📌 Remember: GSTPAID for mania severity assessment - Grandiosity, Sleep reduction, Talkativeness, Pleasurable activities, Agitation, Irritability, Distractibility. Psychotic features occur in 60% of severe episodes, requiring immediate intervention.
The sleep architecture becomes profoundly disrupted, with REM sleep reduced by 40-60% and total sleep time decreasing to 2-4 hours nightly without fatigue. Cognitive processing accelerates beyond functional capacity, creating flight of ideas where thoughts connect through loose associations rather than logical progression.
- Core Manic Symptoms (≥3 required for diagnosis)
- Elevated/Irritable Mood: Persistent euphoria or irritability lasting ≥7 days
- Decreased Sleep Need: Feeling rested after ≤3 hours sleep for multiple days
- Grandiosity: Inflated self-esteem or unrealistic beliefs about abilities
- Mild: Increased confidence, optimism about capabilities
- Severe: Delusional grandiosity - believing special powers, famous identity
- Pressured Speech: Rapid, excessive talking that's difficult to interrupt
- Racing Thoughts: Subjective experience of accelerated thinking or flight of ideas
- Distractibility: Attention easily drawn to irrelevant stimuli
- Increased Goal-Directed Activity: Hyperactivity in work, social, or sexual domains
- Poor Judgment: Risky behaviors with high potential for negative consequences
⭐ Clinical Pearl: Mixed mania occurs in 40% of episodes, combining manic energy with depressive mood, creating extremely high suicide risk (15-20% lifetime rate). Rapid cycling (≥4 episodes/year) affects 20% of patients and predicts poorer treatment response.
| Mania Severity | Functional Impairment | Psychotic Features | Hospitalization | Duration | Treatment Response |
|---|---|---|---|---|---|
| Mild | Minimal work/social impact | Absent | Rarely required | 7-14 days | 80% response rate |
| Moderate | Significant impairment | Rare (<10%) | Often beneficial | 2-4 weeks | 65% response rate |
| Severe | Complete dysfunction | Common (60%) | Usually required | 4-8 weeks | 45% response rate |
| Psychotic | Total incapacitation | Present (100%) | Always required | 6-12 weeks | 30% response rate |
💡 Master This: Mania isn't happiness - it's pathological brain hyperactivity requiring immediate mood stabilization. Early intervention within 48-72 hours can prevent episode escalation and reduce recovery time by 50%. Antipsychotics provide fastest symptom control (3-7 days), while mood stabilizers prevent future episodes.
Recognizing mania's neurobiological complexity enables targeted interventions that restore normal brain circuit function and prevent the devastating personal and social consequences of untreated episodes.
⚡ Manic Episodes: The Brain's Electrical Overdrive
🎭 Hypomanic Episodes: The Subtle Mood Elevation
The neurobiological substrate involves moderate dopaminergic activation in reward circuits without the excessive overflow seen in full mania. Sleep reduction occurs but typically 4-6 hours nightly rather than the 2-3 hours characteristic of mania. Cognitive enhancement may actually improve work performance and creative output.
📌 Remember: HYPOMANIA criteria - High energy, Yearning for less sleep, Productivity increased, Optimism excessive, Mood elevated, Activity surge, No psychosis, Impairment minimal, At least 4 days duration. Key distinction: observable by others but not severely impairing.
- Hypomanic Recognition Patterns
- Mood Changes: Clearly different from baseline personality but not severely impairing
- Sleep Patterns: Decreased need for sleep (4-6 hours) with maintained energy
- Cognitive Changes: Enhanced focus, increased creativity, rapid thinking
- Positive aspects: Improved work performance, increased social engagement
- Concerning signs: Poor judgment, increased risk-taking, irritability
- Behavioral Shifts: Increased talkativeness, higher activity levels, elevated confidence
- Social Functioning: Enhanced initially, but may become strained with irritability
⭐ Clinical Pearl: 70% of hypomanic episodes are missed during initial assessment because patients report feeling "better than normal". Collateral history from family/friends is essential since patients often lack insight into mood changes. Antidepressant-induced hypomania occurs in 25% of bipolar patients.
| Feature | Hypomania | Mania | Normal Mood | Clinical Significance | Treatment Urgency |
|---|---|---|---|---|---|
| Duration | ≥4 days | ≥7 days | Variable | Diagnostic threshold | Moderate |
| Impairment | Minimal | Severe | None | Functional assessment | Low-Moderate |
| Psychosis | Never | 60% severe | Never | Hospitalization need | High if present |
| Sleep Need | 4-6 hours | 2-3 hours | 7-9 hours | Circadian disruption | Moderate |
| Insight | Often poor | Usually absent | Present | Treatment compliance | Variable |
💡 Master This: Hypomania isn't "feeling good" - it's mild mood circuit dysfunction that predicts future severe episodes. Early recognition enables preventive treatment that can reduce mania risk by 70%. Mood charting helps patients recognize patterns and triggers for proactive management.
The treatment approach focuses on mood stabilization rather than symptom suppression, since hypomania often feels subjectively positive. Lithium or anticonvulsants provide prophylactic benefit, while antipsychotics are typically unnecessary unless rapid cycling or mixed features develop.
Understanding hypomania's subtle presentation enables early intervention that can prevent progression to full mania and reduce the long-term morbidity associated with untreated bipolar disorder.
🎭 Hypomanic Episodes: The Subtle Mood Elevation
🌊 Depressive Episodes: The Bipolar Undertow
The pathophysiology involves dopaminergic hypofunction in reward circuits, serotonergic deficiency in mood regulation centers, and altered HPA axis activity creating cortisol dysregulation. Neuroimaging reveals decreased activity in prefrontal cortex and anterior cingulate, with hyperactive amygdala processing negative emotions.
📌 Remember: SIGECAPS for depression screening - Sleep disturbance, Interest loss, Guilt/worthlessness, Energy decrease, Concentration problems, Appetite changes, Psychomotor changes, Suicidal ideation. ≥5 symptoms for ≥2 weeks with functional impairment required for diagnosis.
- Bipolar Depression Characteristics
- Onset Patterns: Earlier age of onset (average 18-22 years) vs unipolar (25-30 years)
- Episode Features: Shorter duration (6-9 months) but more frequent recurrence
- Symptom Profile: Hypersomnia (60%), hyperphagia (40%), psychomotor retardation (70%)
- Atypical features: Mood reactivity, leaden paralysis, rejection sensitivity
- Psychotic features: 20% of severe episodes, typically mood-congruent
- Cognitive Impact: Executive dysfunction, memory impairment, processing speed reduction
- Suicidal Risk: Lifetime rate 15-20%, highest during mixed episodes and early illness
⭐ Clinical Pearl: Bipolar depression accounts for 50% of total illness burden despite representing 30% of episode time. Rapid cycling increases depression frequency and treatment resistance. Seasonal patterns occur in 25%, typically fall/winter onset.
| Feature | Bipolar Depression | Unipolar Depression | Clinical Implication | Treatment Difference | Prognosis |
|---|---|---|---|---|---|
| Age of Onset | 18-22 years | 25-30 years | Earlier intervention need | Mood stabilizer priority | More episodes |
| Episode Duration | 6-9 months | 12-18 months | Shorter but recurrent | Maintenance therapy | Chronic course |
| Psychotic Features | 20% | 10% | Higher severity | Antipsychotic need | Poorer outcome |
| Suicide Risk | 15-20% | 10-15% | Higher lethality | Crisis intervention | Requires monitoring |
| Treatment Response | 60% response | 70% response | More resistant | Combination therapy | Partial remission |
💡 Master This: Bipolar depression isn't just "sadness" - it's complex mood circuit dysfunction requiring specialized treatment approaches. Antidepressant monotherapy can worsen long-term outcomes by increasing episode frequency. Combination therapy with mood stabilizers provides optimal efficacy while preventing mania induction.
Lamotrigine shows particular efficacy for bipolar depression with minimal mania risk, requiring slow titration (25mg weekly increases) to prevent Stevens-Johnson syndrome (0.1% risk). Quetiapine provides rapid onset (1-2 weeks) for acute episodes with sedating properties beneficial for sleep disturbance.
Understanding bipolar depression's unique characteristics enables targeted treatment that addresses both acute symptoms and long-term mood stabilization while avoiding interventions that could destabilize the underlying mood disorder.
🌊 Depressive Episodes: The Bipolar Undertow
⚖️ Treatment Algorithms: Precision Mood Stabilization
The pharmacological approach targets multiple neurotransmitter systems simultaneously. Lithium modulates inositol signaling and neuroprotection, anticonvulsants stabilize sodium/calcium channels, and antipsychotics block dopamine/serotonin receptors. Therapeutic drug monitoring ensures optimal levels while minimizing toxicity.
📌 Remember: LITHIUM monitoring requirements - Level checks (0.6-1.2 mEq/L), Iodine function (TSH q6mo), Toxicity signs, Heart rhythm (ECG baseline), Interaction awareness, Urine concentration (creatinine q6mo), Mood tracking. Therapeutic window is narrow with toxicity risk at >1.5 mEq/L.
- Acute Mania Treatment Protocol
- First-Line Combinations: Lithium + antipsychotic or valproate + antipsychotic
- Antipsychotic Selection: Olanzapine (15-20mg/day), risperidone (2-6mg/day), quetiapine (400-800mg/day)
- Rapid onset: 3-7 days for behavioral control
- Sedation benefit: Addresses sleep disturbance and agitation
- Mood Stabilizer Dosing: Lithium (900-1200mg/day), valproate (1000-2000mg/day)
- Monitoring Requirements: Weekly levels until therapeutic, then monthly
- Duration: Acute phase (6-8 weeks), continuation (4-6 months), maintenance (≥2 years)
⭐ Clinical Pearl: Combination therapy achieves remission in 70-80% of manic episodes vs 50-60% with monotherapy. Antipsychotic loading (higher initial doses) provides faster control but increases side effect risk. Benzodiazepines (lorazepam 2-4mg) offer adjunctive sedation for severe agitation.
| Medication Class | Mechanism | Onset Time | Efficacy Rate | Major Side Effects | Monitoring Required |
|---|---|---|---|---|---|
| Lithium | Inositol modulation | 7-14 days | 80% mania | Tremor, polyuria, weight gain | Levels, kidney, thyroid |
| Valproate | GABA enhancement | 5-10 days | 75% mania | Weight gain, hair loss, tremor | Levels, liver, CBC |
| Olanzapine | D2/5HT2 blockade | 3-7 days | 85% mania | Weight gain, diabetes risk | Glucose, lipids, weight |
| Quetiapine | Multiple receptors | 1-3 days | 70% depression | Sedation, weight gain | Glucose, lipids, ECG |
| Lamotrigine | Sodium channel block | 4-6 weeks | 65% depression | Rash risk, dizziness | Rash monitoring |
💡 Master This: Bipolar treatment isn't trial-and-error - it's evidence-based algorithm implementation requiring systematic approach and careful monitoring. Early aggressive treatment of first episodes can prevent brain changes and reduce future episode frequency by 60-70%. Maintenance therapy is lifelong for most patients.
Maintenance therapy focuses on episode prevention rather than symptom treatment. Lithium remains gold standard with suicide prevention benefits and neuroprotective effects. Combination maintenance (lithium + anticonvulsant) may provide superior prophylaxis for treatment-resistant cases.
Treatment resistance (<50% symptom reduction) occurs in 30-40% of patients, requiring algorithm advancement to second-line agents (carbamazepine, clozapine) or novel approaches (ECT, ketamine). Adherence optimization through psychoeducation and side effect management improves long-term outcomes.
⚖️ Treatment Algorithms: Precision Mood Stabilization
🔗 Comorbidity Patterns: The Bipolar Complexity Web
The neurobiological overlap involves dysregulated reward circuits, impaired impulse control, and altered stress response systems. Anxiety disorders share amygdala hyperactivity and GABA dysfunction with bipolar disorder. Medical comorbidities including diabetes (2-3x increased risk), cardiovascular disease (2x risk), and thyroid disorders (15% prevalence) complicate treatment selection.
📌 Remember: BIPOLAR COMORBIDITIES - Behavioral addictions, Impulse control disorders, Panic disorder, OCD, Learning disabilities, ADHAD, Reality testing issues. Substance use occurs in 60% of patients and doubles relapse risk while reducing medication adherence by 40%.
- Substance Use Disorder Integration
- Alcohol Use Disorder: 40% lifetime prevalence, worsens mood cycling and medication compliance
- Cannabis Use: 20% prevalence, may trigger mania in vulnerable individuals
- Stimulant Use: 15% prevalence, directly induces mania and psychosis
- Treatment approach: Dual diagnosis programs with integrated care
- Medication considerations: Avoid stimulating agents, monitor for interactions
- Nicotine Dependence: 70% prevalence (3x general population), complicates medical management
- Recovery Impact: Substance use doubles hospitalization rates and triples suicide risk
⭐ Clinical Pearl: Anxiety comorbidity occurs in 50% of bipolar patients and predicts earlier onset, more severe episodes, and poorer treatment response. PTSD co-occurs in 25% and increases rapid cycling risk. Eating disorders affect 15% of bipolar women and complicate medication management.
| Comorbid Condition | Prevalence | Impact on Course | Treatment Modifications | Outcome Effect | Monitoring Needs |
|---|---|---|---|---|---|
| Alcohol Use Disorder | 40% | Worsens cycling | Avoid sedating meds | 2x relapse risk | Liver function |
| Anxiety Disorders | 50% | Earlier onset | Add anxiolytics | Poorer response | Benzodiazepine risk |
| ADHD | 20% | Diagnostic confusion | Stimulant caution | 3x substance risk | Mood monitoring |
| Diabetes | 15% | Medication limits | Avoid weight gain | Increased mortality | Glucose monitoring |
| Thyroid Disease | 15% | Mood destabilization | Hormone replacement | Cycling worsens | TSH monitoring |
ADHD comorbidity creates diagnostic challenges since mania symptoms overlap with ADHD presentation. Stimulant medications can trigger mania in 30% of bipolar patients. Non-stimulant options (atomoxetine, bupropion) provide safer alternatives with mood stabilizer combination.
💡 Master This: Bipolar comorbidity isn't additive - it's multiplicative complexity requiring integrated treatment planning. Substance use doubles treatment failure rates and requires specialized dual-diagnosis approaches. Medical comorbidities limit medication options and increase mortality risk by 2-3 fold.
Integrated care models combining psychiatric, addiction, and medical specialties improve outcomes significantly. Collaborative care with primary care providers ensures comprehensive monitoring of metabolic effects, drug interactions, and medical complications. Psychosocial interventions addressing multiple conditions simultaneously provide superior long-term outcomes.
The treatment hierarchy prioritizes mood stabilization first, then addresses comorbidities systematically. Medication selection considers all conditions to minimize interactions and maximize therapeutic benefit. Regular monitoring protocols track multiple parameters to detect complications early and adjust treatment accordingly.
🔗 Comorbidity Patterns: The Bipolar Complexity Web
🎯 Clinical Mastery Arsenal: Bipolar Expertise Tools
📌 Remember: BIPOLAR MASTERY essentials - Biomarker monitoring, Integrated care approach, Patient education, Outcome tracking, Lifelong maintenance, Adherence optimization, Risk assessment. Early intervention within first 5 years can alter disease trajectory and prevent 60-70% of future episodes.
- Rapid Assessment Protocol (5-minute screening)
- Mood Disorder Questionnaire (MDQ): Sensitivity 85%, specificity 75% for bipolar screening
- Previous episode history: Age of onset, episode frequency, hospitalization history
- Family psychiatric history: First-degree relatives with mood disorders or suicide
- Substance use screening: Current use, temporal relationship to mood episodes
- Medication response patterns: Antidepressant-induced mania, mood stabilizer response
| Clinical Tool | Application | Time Required | Sensitivity | Specificity | Clinical Value |
|---|---|---|---|---|---|
| MDQ | Bipolar screening | 2 minutes | 85% | 75% | Initial assessment |
| YMRS | Mania severity | 5 minutes | 90% | 85% | Treatment monitoring |
| MADRS | Depression severity | 10 minutes | 85% | 80% | Outcome tracking |
| CGI-BP | Global improvement | 2 minutes | 80% | 90% | Treatment response |
| Mood charts | Pattern recognition | Daily | 95% | 70% | Long-term monitoring |
Treatment Response Predictors enable personalized medicine approaches:
- Rapid response (<7 days): Antipsychotic monotherapy for acute mania
- Gradual response (2-4 weeks): Mood stabilizer combinations for complex presentations
- Treatment resistance (<50% improvement): Algorithm advancement to second-line agents
- Maintenance success: Adherence >80%, regular monitoring, psychosocial support
💡 Master This: Bipolar expertise isn't memorizing facts - it's systematic pattern recognition combined with evidence-based decision-making. Early accurate diagnosis can prevent 15-20 years of misdiagnosis and inappropriate treatment. Maintenance therapy adherence reduces episode recurrence by 70-80% and prevents progressive brain changes.
Essential Clinical Thresholds for immediate action:
- Lithium >1.5 mEq/L: Hold medication, check kidney function, assess toxicity symptoms
- Mania severity >25 YMRS: Consider hospitalization, antipsychotic initiation, safety assessment
- Depression with suicidal ideation: Risk assessment, safety planning, intensive monitoring
- Mixed episode presentation: High suicide risk, avoid antidepressants, antipsychotic priority
The bipolar mastery mindset transforms complex presentations into systematic assessments using validated tools and evidence-based protocols. Expert clinicians achieve superior outcomes through early recognition, aggressive initial treatment, and meticulous long-term monitoring that prevents relapse and optimizes functional recovery.
🎯 Clinical Mastery Arsenal: Bipolar Expertise Tools
Practice Questions: Bipolar disorder
Test your understanding with these related questions
A 35-year-old man is brought to the emergency department by his wife. She was called by his coworkers to come and pick him up from work after he barged into the company’s board meeting and was being very disruptive as he ranted on about all the great ideas he had for the company. When they tried to reason with him, he became hostile and insisted that he should be the CEO as he knew what was best for the future of the company. The patient’s wife also noted that her husband has been up all night for the past few days but assumed that he was handling a big project at work. The patient has no significant past medical or psychiatric history. Which of the following treatments is most likely to benefit this patient’s condition?













