Neurobiological basis of anxiety US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neurobiological basis of anxiety. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neurobiological basis of anxiety US Medical PG Question 1: A 52-year-old woman presents to her primary care physician for her annual checkup. She lost her job 6 months ago and since then she has been feeling worthless because nobody wants to hire her. She also says that she is finding it difficult to concentrate, which is exacerbated by the fact that she has lost interest in activities that she used to love such as doing puzzles and working in the garden. She says that she is sleeping over 10 hours every day because she says it is difficult to find the energy to get up in the morning. She denies having any thoughts about suicide. Which of the following neurotransmitter profiles would most likely be seen in this patient?
- A. Increased dopamine
- B. Decreased serotonin and norepinephrine (Correct Answer)
- C. Increased norepinephrine
- D. Decreased acetylcholine
- E. Decreased gamma-aminobutyric acid
Neurobiological basis of anxiety Explanation: ***Decreased serotonin and norepinephrine***
- The patient's symptoms, including **worthlessness**, difficulty **concentrating**, loss of **interest (anhedonia)**, and **hypersomnia**, are classic for **major depressive disorder**.
- **Depression** is most commonly associated with a deficiency in **monoamine neurotransmitters**, particularly **serotonin** and **norepinephrine**, which play key roles in mood, sleep, appetite, and cognition.
*Increased dopamine*
- **Increased dopamine** activity is more often associated with conditions like **psychosis (e.g., schizophrenia)** or the manic phases of **bipolar disorder**, which are not indicated by the patient's symptoms.
- While dopamine is involved in reward and motivation, a primary increase is not the typical finding in major depression.
*Increased norepinephrine*
- An **increase in norepinephrine** is often seen in conditions like **anxiety disorders**, **panic attacks**, or **mania**, characterized by states of heightened arousal and vigilance.
- The patient's symptoms of **lethargy**, **hypersomnia**, and **lack of energy** point away from an overall increase in norepinephrine.
*Decreased acetylcholine*
- **Decreased acetylcholine** is primarily linked to cognitive deficits seen in conditions like **Alzheimer's disease**, affecting memory and learning.
- While depression can involve cognitive impairment, a primary deficit in acetylcholine is not the hallmark neurotransmitter change in major depressive disorder.
*Decreased gamma-aminobutyric acid*
- **Decreased GABA** (gamma-aminobutyric acid) is primarily associated with conditions of heightened excitability and anxiety, such as **anxiety disorders**, **insomnia**, and **seizure disorders**.
- The patient's presentation of **hypersomnia** and **low energy** is inconsistent with a primary GABA deficiency.
Neurobiological basis of anxiety US Medical PG Question 2: A 52-year-man is brought to the physician because of a 2-week history of memory loss. Three weeks ago, he had a cardiac arrest that required cardiopulmonary resuscitation and intravenous epinephrine. On mental status examination, he cannot recall objects shown to him 20 minutes earlier but vividly recalls memories from before the incident. The remainder of the examination shows no abnormalities. Which of the following structures of the brain is most likely affected?
- A. Internal pyramidal layer of the amygdala
- B. Microglial cells of dorsal midbrain
- C. Purkinje cells of the cerebellum
- D. Pyramidal cells of the hippocampus (Correct Answer)
- E. Astroglial cells of the putamen
Neurobiological basis of anxiety Explanation: ***Pyramidal cells of the hippocampus***
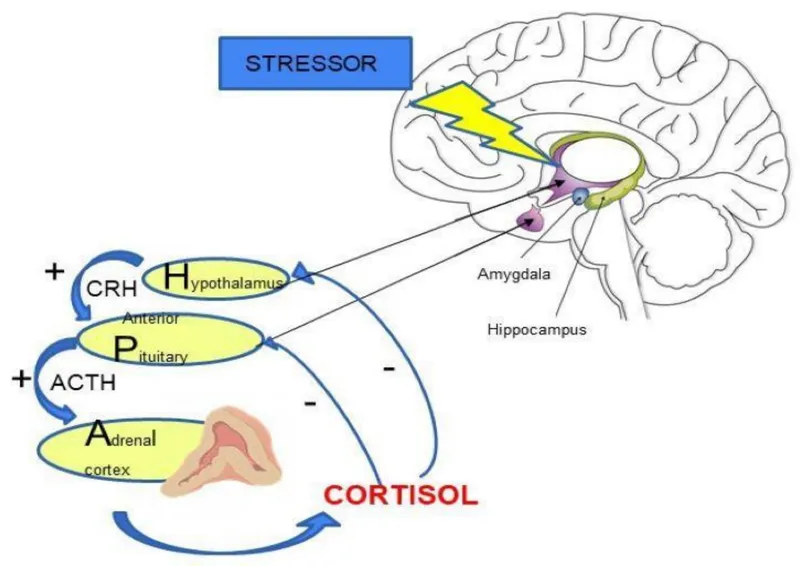
- The patient's inability to form new memories (anterograde amnesia) following a period of **hypoxia** suggests damage to the **hippocampus**, specifically its pyramidal cells.
- The **hippocampus** is highly vulnerable to **ischemic injury** due to the metabolic demands of its pyramidal cells.
*Internal pyramidal layer of the amygdala*
- The amygdala is primarily involved in **emotional processing**, particularly fear and anxiety, not memory encoding directly.
- Damage to the amygdala would likely manifest as altered emotional responses, rather than isolated memory loss.
*Microglial cells of dorsal midbrain*
- Microglial cells are the brain's resident immune cells and proliferate in response to injury, they are not the primary site of memory formation.
- The dorsal midbrain contains structures involved in visual and auditory reflexes, not directly memory consolidation.
*Purkinje cells of the cerebellum*
- Purkinje cells are specialized neurons in the **cerebellum** responsible for **motor coordination** and balance.
- Damage to these cells would result in ataxia and motor dysfunction, not memory deficits.
*Astroglial cells of the putamen*
- Astroglial cells are supportive cells throughout the brain; the putamen is involved in **motor control** and **procedural learning**.
- Dysfunction of the putamen typically leads to movement disorders like Parkinsonism, not specific memory loss.
Neurobiological basis of anxiety US Medical PG Question 3: A 45-year-old woman presents to her primary care physician with complaints of muscle pains, poor sleep, and daytime fatigue. When asked about stressors she states that she "panics" about her job, marriage, children, and finances. When asked to clarify what the "panics" entail, she states that it involves severe worrying. She has had these symptoms since she last saw you one year ago. What is the most likely diagnosis?
- A. Generalized anxiety disorder (Correct Answer)
- B. Social phobia
- C. Adjustment disorder
- D. Obsessive-compulsive disorder
- E. Panic disorder
Neurobiological basis of anxiety Explanation: ***Generalized anxiety disorder***
- This patient presents with **chronic, excessive, and uncontrollable worry** about multiple life circumstances (job, marriage, children, finances), fulfilling the core diagnostic criterion for GAD.
- The associated symptoms of **muscle pains**, **poor sleep**, and **daytime fatigue** are common physical manifestations of GAD, and the duration of symptoms for over a year supports the diagnosis.
*Social phobia*
- **Social phobia**, or social anxiety disorder, involves intense fear and anxiety in **social situations** where one might be scrutinized or judged.
- The patient's reported worries are broad and not limited to social interactions, making social phobia less likely.
*Adjustment disorder*
- **Adjustment disorder** is characterized by emotional or behavioral symptoms developing within **three months of an identifiable stressor**, not diffuse chronic worry.
- The symptoms in adjustment disorder typically resolve within **six months** after the stressor or its consequences have ended, whereas this patient's symptoms are chronic and pervasive.
*Obsessive-compulsive disorder*
- **Obsessive-compulsive disorder (OCD)** involves recurrent, intrusive **obsessions** (thoughts, urges, images) and/or **compulsions** (repetitive behaviors or mental acts) performed to reduce anxiety.
- While the patient experiences severe worrying, there's no mention of specific obsessions or compulsive behaviors aimed at neutralizing those anxieties.
*Panic disorder*
- **Panic disorder** is characterized by recurrent, unexpected **panic attacks**—sudden surges of intense fear or discomfort accompanied by physical and cognitive symptoms.
- While the patient uses the term "panics," she clarifies it involves "severe worrying," not discrete, intense, and short-lived panic attacks.
Neurobiological basis of anxiety US Medical PG Question 4: A 27-year-old man is brought to a psychiatrist by his mother who is concerned that he has become increasingly distant. When asked, he says that he is no longer going out because he is afraid of going outside by himself. He says that ever since he was a teenager, he was uncomfortable in large crowds and on public transportation. He now works from home and rarely leaves his house except on mandatory business. Which of the following personality disorders is most likely genetically associated with this patient's disorder?
- A. Dependent
- B. Schizotypal
- C. Histrionic
- D. Antisocial
- E. Paranoid
- F. Avoidant (Correct Answer)
Neurobiological basis of anxiety Explanation: ***Avoidant***
- This patient exhibits symptoms consistent with **agoraphobia**, which is an **anxiety disorder** characterized by fear of situations where escape might be difficult or help unavailable, often leading to social isolation.
- **Avoidant Personality Disorder** has the strongest genetic association with anxiety disorders, particularly **social anxiety disorder and agoraphobia**, sharing common genetic vulnerability factors related to fear of negative evaluation and social avoidance.
- Studies demonstrate significant genetic overlap between avoidant personality disorder and anxiety spectrum disorders, making this the most likely genetically associated personality disorder.
*Schizotypal*
- **Schizotypal Personality Disorder** is genetically linked to the **schizophrenia spectrum** (not anxiety disorders), characterized by cognitive-perceptual distortions, eccentric behavior, and social deficits.
- While schizotypal patients may avoid social situations, this is due to odd thinking and discomfort with close relationships, not anxiety about specific situations like crowds or public transportation.
*Dependent*
- **Dependent Personality Disorder** is characterized by an excessive need to be taken care of, leading to **submissive and clinging behavior**, and fears of separation.
- This patient's withdrawal is due to fear of public places, not a reliance on others or fear of abandonment.
*Antisocial*
- **Antisocial Personality Disorder** involves a pervasive pattern of **disregard for and violation of the rights of others**, often presenting as deceitful and impulsive behavior.
- The patient's symptoms are rooted in anxiety and social avoidance rather than a lack of empathy or antisocial behavior.
*Paranoid*
- **Paranoid Personality Disorder** is characterized by a pervasive **distrust and suspiciousness of others**, interpreting their motives as malevolent.
- The patient's withdrawal stems from fear of specific situations (crowds, public transport) rather than paranoid ideation or general suspicion of people's intentions.
*Histrionic*
- **Histrionic Personality Disorder** is marked by **excessive emotionality and attention-seeking behavior**, often displaying dramatic and superficial interactions.
- The patient's isolation and fear of public spaces are directly opposite to the attention-seeking nature of histrionic traits.
Neurobiological basis of anxiety US Medical PG Question 5: A 43-year-old woman comes to the physician for an annual health maintenance examination. On questioning, she has had fatigue and headaches for the last month. A few weeks ago, she had to have her wedding ring resized because it had become too small for her finger. She has mild persistent asthma and anxiety disorder. She drinks 2–3 glasses of red wine per night and has smoked one pack of cigarettes daily for 16 years. She works a desk job in accounting and has recently been working long hours due to an upcoming company merger. Her father has a history of a pituitary adenoma. Current medications include alprazolam, a fluticasone inhaler, and an albuterol inhaler. She is 160 cm (5 ft 3 in) tall and weighs 81.6 kg (180 lb); her BMI is 32 kg/m2. Her temperature is 37.2°C (99°F), pulse is 92/min, and blood pressure is 132/80 mm Hg. Examination shows no abnormalities. Fasting laboratory studies show:
Hemoglobin 13 g/dL
Serum
Na+ 135 mEq/L
K+
4.6 mEq/L
Cl- 105 mEq/L
HCO3- 22 mEq/L
Urea nitrogen 17 mg/dL
Glucose 160 mg/dL
Creatinine 0.9 mg/dL
Which of the following is the most likely underlying mechanism of this patient's hyperglycemia?
- A. Decreased insulin production
- B. Adverse effect of medication
- C. Stress
- D. Insulin resistance (Correct Answer)
- E. Hypersecretion of ACTH
Neurobiological basis of anxiety Explanation: ***Insulin resistance***
- The patient's **obesity (BMI 32 kg/m2)**, **sedentary lifestyle**, and **fasting hyperglycemia** (glucose 160 mg/dL) indicate **insulin resistance**, which is the underlying mechanism of hyperglycemia in **type 2 diabetes**.
- The **ring resizing due to finger enlargement**, **fatigue**, **headaches**, and **family history of pituitary adenoma** raise suspicion for **acromegaly** (growth hormone excess), which also causes hyperglycemia through **insulin resistance** - growth hormone antagonizes insulin action at peripheral tissues.
- Regardless of whether this represents type 2 diabetes or acromegaly, **insulin resistance is the direct mechanism** causing the hyperglycemia in this patient.
*Decreased insulin production*
- Decreased insulin production is characteristic of **type 1 diabetes** or late-stage type 2 diabetes with beta-cell exhaustion.
- The patient's **obesity** and typical metabolic risk factors suggest **insulin resistance** rather than decreased production as the primary mechanism.
- No clinical features suggest autoimmune destruction or significant pancreatic damage.
*Adverse effect of medication*
- The patient's medications (**alprazolam**, **fluticasone inhaler**, **albuterol**) are unlikely to cause significant fasting hyperglycemia.
- While high-dose systemic **corticosteroids** can cause hyperglycemia, **inhaled fluticasone** at typical asthma doses has minimal systemic absorption and is not a common cause of sustained hyperglycemia.
- **Alprazolam** and **albuterol** do not typically cause hyperglycemia.
*Stress*
- **Acute stress** can transiently elevate blood glucose through counter-regulatory hormones (cortisol, catecholamines).
- However, the **fasting glucose of 160 mg/dL** suggests a chronic metabolic derangement rather than acute stress response alone.
- Work-related stress may be a contributing factor but is not the primary underlying mechanism.
*Hypersecretion of ACTH*
- **ACTH hypersecretion** (Cushing's disease) causes excess cortisol production, leading to hyperglycemia, weight gain, and fatigue.
- This patient lacks classic features of Cushing's syndrome: **central obesity with thin extremities**, **moon facies**, **buffalo hump**, **purple striae**, **skin thinning**, or **easy bruising**.
- While the patient is obese, the distribution appears generalized rather than the characteristic centripetal pattern of Cushing's syndrome.
Neurobiological basis of anxiety US Medical PG Question 6: A 43-year-old male with a history of thyroid cancer status post total thyroidectomy presents to his primary care physician after repeated bouts of headaches. His headaches are preceded by periods of anxiety, palpitations, and sweating. The patient says he is unable to pinpoint any precipitating factors and instead says the events occur without warning. Of note, the patient's father and uncle also have a history of thyroid cancer. On exam his vitals are: T 36.8 HR 87, BP 135/93, RR 14, and O2 Sat 100% on room air. The patient's TSH is within normal limits, and he reports taking his levothyroxine as prescribed. What is the next best step in diagnosing this patient's chief complaint?
- A. 24-hour urine free cortisol
- B. Plasma aldosterone/renin ratio
- C. Abdominal CT scan with and without IV contrast
- D. Plasma fractionated metanephrines (Correct Answer)
- E. High dose dexamethasone suppression test
Neurobiological basis of anxiety Explanation: ***Plasma fractionated metanephrines***
- The patient's symptoms of **anxiety, palpitations, sweating, and headaches** occurring in discrete "attacks" are classic for a **pheochromocytoma**, a tumor that secretes catecholamines.
- Given the patient's and his family's history of **thyroid cancer**, specifically likely **medullary thyroid cancer** due to the familial link, there is a high suspicion for **Multiple Endocrine Neoplasia type 2 (MEN2)**, which commonly includes pheochromocytoma. **Plasma fractionated metanephrines** are the most sensitive screening test for pheochromocytoma.
*24-hour urine free cortisol*
- This test is used to detect **Cushing's syndrome**, which involves excessive cortisol production.
- Although Cushing's can cause **hypertension**, the paroxysmal symptoms of anxiety, palpitations, and sweating are not typical of Cushing's syndrome.
*Plasma aldosterone/renin ratio*
- This ratio is used to screen for **primary hyperaldosteronism**, a cause of secondary hypertension.
- While the patient has **hypertension (135/93 mm Hg)**, his symptom complex of episodic anxiety, palpitations, and sweating is not characteristic of primary hyperaldosteronism.
*Abdominal CT scan with and without IV contrast*
- An abdominal CT scan can visualize adrenal masses, but it is typically performed *after* biochemical confirmation of a pheochromocytoma to localize the tumor.
- Performing imaging before biochemical testing risks incidentalomas or missing a biochemically active but small tumor, and it is not the most appropriate *next step* in diagnosis given the strong clinical suspicion.
*High dose dexamethasone suppression test*
- This test is specifically used to differentiate between **Cushing's disease** (pituitary ACTH excess) and other causes of Cushing's syndrome.
- The patient's symptoms are not consistent with excessive cortisol production, making this test inappropriate for his chief complaint.
Neurobiological basis of anxiety US Medical PG Question 7: A 42-year-old female complains of feeling anxious and worrying about nearly every aspect of her daily life. She cannot identify a specific cause for these symptoms and admits that this tension is accompanied by tiredness and difficulty falling asleep. To treat this problem, the patient is prescribed sertraline. She endorses a mild improvement with this medication, and over the next several months, her dose is increased to the maximum allowed dose with modest improvement. Her psychiatrist adds an adjunctive treatment, a medication which notably lacks any anticonvulsant or muscle relaxant properties. This drug most likely acts at which of the following receptors?
- A. Beta adrenergic receptor
- B. 5HT-1A receptor (Correct Answer)
- C. GABA receptor
- D. Alpha adrenergic receptor
- E. Glycine receptor
Neurobiological basis of anxiety Explanation: ***5HT-1A receptor***
- The patient's presentation of generalized anxiety disorder, treated with an SSRI (sertraline) and an adjunctive medication that lacks anticonvulsant or muscle relaxant properties, points to **buspirone**.
- **Buspirone** is a 5HT-1A partial agonist, commonly used as an augmenting agent in anxiety disorders, which explains the mechanism of action.
*Beta adrenergic receptor*
- Medications acting on **beta-adrenergic receptors** (e.g., propranolol) are typically used for situational anxiety or performance anxiety, not generalized anxiety disorder, and they primarily reduce physical symptoms like palpitations and tremors.
- While beta-blockers lack anticonvulsant or muscle relaxant properties, they are not typically considered a first-line adjunctive therapy for generalized anxiety after an SSRI failure.
*GABA receptor*
- Drugs acting on **GABA receptors** (e.g., benzodiazepines) are known for their anxiolytic, sedative, anticonvulsant, and muscle relaxant properties.
- The question explicitly states that the adjunctive medication "notably lacks any anticonvulsant or muscle relaxant properties," ruling out GABAergic drugs.
*Alpha adrenergic receptor*
- Medications targeting **alpha-adrenergic receptors** (e.g., clonidine) are sometimes used for anxiety associated with opiate withdrawal or PTSD, but are not a common adjunctive treatment for generalized anxiety disorder in this context.
- While they may lack anticonvulsant or muscle relaxant properties, their primary mechanism involves regulating sympathetic outflow rather than the specific mood and cognitive symptoms of GAD.
*Glycine receptor*
- The **glycine receptor** is an inhibitory ion channel, primarily found in the spinal cord and brainstem, involved in motor control and pain processing.
- Agonists of this receptor are not commonly used to treat anxiety disorders, and the described clinical scenario does not align with its therapeutic applications.
Neurobiological basis of anxiety US Medical PG Question 8: Every time your neighbor in the adjacent apartment flushes the toilet, the water in your shower becomes very hot, causing you to jump out of the way of the water stream. After this has occurred for several months, you note that you reflexively jump back from the water directly after the sound of the flushing toilet but before the water temperature changes. Which of the following situations is the most similar to the conditioning process detailed above?
- A. You consistently check the slots of pay telephones as you have previously found change left there
- B. White coat syndrome (patient anxiety evoked at the sight of a white lab coat) (Correct Answer)
- C. A young child elects to not throw a temper tantrum to avoid being grounded by his parents
- D. A mouse repeatedly presses a red button to avoid receiving an electric shock
- E. You now sleep through the noise of the train running past your apartment that kept you up 1 year ago
Neurobiological basis of anxiety Explanation: ***White coat syndrome (patient anxiety evoked at the sight of a white lab coat)***
- This is an example of **classical conditioning**, where a neutral stimulus (**white coat**) becomes associated with an unconditioned stimulus (pain/anxiety-inducing medical procedures), leading to a conditioned response (anxiety).
- Similarly, the **sound of the flush** (neutral stimulus) became associated with the **hot water** (unconditioned stimulus), leading to a **reflexive jump** (conditioned response).
*You consistently check the slots of pay telephones as you have previously found change left there*
- This scenario represents **operant conditioning**, specifically **positive reinforcement**, where checking the slot is reinforced by the reward of finding change.
- The behavior is strengthened by the **consequence** that follows it, rather than an association between two stimuli.
*A young child elects to not throw a temper tantrum to avoid being grounded by his parents*
- This is an example of **negative punishment** in **operant conditioning**, where the child avoids a negative consequence (being grounded) by refraining from a specific behavior (tantrum).
- The focus is on the **consequences** of an action influencing future behavior, not an involuntary, learned association between stimuli.
*A mouse repeatedly presses a red button to avoid receiving an electric shock*
- This describes **operant conditioning**, specifically **negative reinforcement**, where the mouse performs an action (**pressing the button**) to remove an aversive stimulus (**electric shock**).
- It involves a voluntary action to escape or avoid an unpleasant event, differing from the involuntary, anticipatory reflex seen in classical conditioning.
*You now sleep through the noise of the train running past your apartment that kept you up 1 year ago*
- This is an example of **habituation**, a non-associative learning process where an organism decreases its response to a stimulus after repeated exposure.
- The organism learns to **ignore** an irrelevant or non-threatening stimulus, rather than forming a new association between two stimuli.
Neurobiological basis of anxiety US Medical PG Question 9: An 8-year-old boy is brought to his pediatrician by his mother because she is worried about whether he is becoming ill. Specifically, he has been sent home from school six times in the past month because of headaches and abdominal pain. In fact, he has been in the nurse's office almost every day with various symptoms. These symptoms started when the family moved to an old house in another state about 2 months ago. Furthermore, whenever he is taken care of by a babysitter he also has these symptoms. Despite these occurrences, the boy never seems to have any problems at home with his parents. Which of the following treatments would likely be effective for this patient?
- A. Play therapy (Correct Answer)
- B. Succimer
- C. Supportive only
- D. Clonidine
- E. Methylphenidate
Neurobiological basis of anxiety Explanation: ***Play therapy***
- The boy's symptoms are likely **psychosomatic**, triggered by **stressors** like moving and separation from parents, as they resolve at home.
- **Play therapy** is an effective treatment for children experiencing emotional or behavioral difficulties due to stress, allowing them to express feelings in a non-threatening environment.
*Succimer*
- **Succimer** is a chelating agent used to treat **lead poisoning**.
- While the family moved to an old house, symptoms like headaches and abdominal pain could be associated with lead exposure, but the **situational nature** of his symptoms (occurring only outside the home or with babysitters) makes lead poisoning less likely.
*Supportive only*
- While supportive care is generally helpful, the severity and persistence of the symptoms suggest that a **more targeted intervention** like therapy is needed to address the underlying psychological distress.
- Simply observing or offering general support would likely not resolve the **situational anxiety** contributing to his somatic complaints.
*Clonidine*
- **Clonidine** is typically used to treat conditions like **ADHD**, **hypertension**, or tics, and is not a primary treatment for psychosomatic complaints in children.
- The patient's symptoms are linked to specific psychological triggers rather than a primary medical or neurological condition usually targeted by clonidine.
*Methylphenidate*
- **Methylphenidate** is a stimulant medication commonly used to treat **Attention-Deficit/Hyperactivity Disorder (ADHD)**.
- There is no indication from the provided symptoms (headaches, abdominal pain, situational nature) that the child has ADHD.
Neurobiological basis of anxiety US Medical PG Question 10: A goalkeeper of a famous soccer team gives an interview with a health agency regarding his childhood. He describes how when he was a child, he would constantly clear his throat in class and the teachers would write a note to his mother with advice to go see an ENT doctor. He complained of being restless, fidgety, and sometimes hyperactive in class, disrupting the environment and causing him many social problems. He would blurt out the answer at times and keep repeating it without any control, leading to some embarrassing timeouts. But he was always nice to his teachers, so he calls it a “benign frustration” rather than aggressively causing distress. He also talked about how his symptoms were dramatically improved with medication. Which of the following is an FDA approved drug for this patient’s most likely condition?
- A. Lithium
- B. Clonazepam
- C. Haloperidol (Correct Answer)
- D. Clonidine
- E. Guanfacine
Neurobiological basis of anxiety Explanation: ***Haloperidol***
- The patient's presentation of constant throat clearing (**motor tics**), blurting out answers and repeating words (**vocal tics**), along with restlessness and hyperactivity, is highly suggestive of **Tourette syndrome**.
- **Haloperidol** is one of the **FDA-approved medications** specifically for Tourette syndrome, along with pimozide and aripiprazole.
- It is a **typical antipsychotic** that effectively treats severe tics through **dopamine D2 receptor blockade**, particularly in the nigrostriatal pathway.
- It remains a gold standard treatment despite potential extrapyramidal side effects.
*Lithium*
- **Lithium** is a **mood stabilizer** used primarily for **bipolar disorder** through its effects on intracellular signaling pathways.
- It has no role in treating Tourette syndrome or tic disorders and is not FDA-approved for this indication.
*Clonazepam*
- **Clonazepam** is a **benzodiazepine** with **GABAergic effects** used for **anxiety disorders**, **panic disorder**, and certain seizure disorders.
- While it may help with comorbid anxiety, it is not a primary treatment for tics and is **not FDA-approved** for Tourette syndrome.
*Clonidine*
- **Clonidine** is an **alpha-2 adrenergic agonist** that can reduce tics, particularly in children with mild to moderate symptoms or comorbid ADHD.
- However, it is **off-label** for Tourette syndrome and not FDA-approved for this indication, though commonly used as a second-line agent.
*Guanfacine*
- **Guanfacine** is also an **alpha-2 adrenergic agonist** similar to clonidine, used primarily for ADHD.
- It may help with tics in an **off-label capacity**, especially when ADHD is comorbid, but it is **not FDA-approved** specifically for Tourette syndrome.
More Neurobiological basis of anxiety US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.