Agoraphobia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Agoraphobia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Agoraphobia US Medical PG Question 1: A 24-year-old male graduate student comes to the physician for a two-month history of repeated thoughts and anxiety that he is going to be harmed by someone on the street. The anxiety worsened after witnessing a pedestrian getting hit by a car two weeks ago. He says, “That was a warning sign.” On his way to school, he now often leaves an hour earlier to take a detour and hide from people that he thinks might hurt him. He is burdened by his coursework and fears that his professors are meaning to fail him. He says his friends are concerned about him but that they do not understand because they were not present at the accident. The patient has no known history of psychiatric illness. On mental status exam, he is alert and oriented, and shows full range of affect. Thought processes and speech are organized. His memory and attention are within normal limits. He denies auditory, visual, or tactile hallucinations. Urine toxicology screening is negative. Which of the following is the most likely diagnosis in this patient?
- A. Avoidant personality disorder
- B. Schizotypal personality disorder
- C. Delusional disorder (Correct Answer)
- D. Generalized anxiety disorder
- E. Acute stress disorder
Agoraphobia Explanation: ***Delusional disorder***
- This patient presents with **persistent non-bizarre delusions** (fear of harm, professors failing him) that have lasted for two months. His functioning is largely intact outside of the delusions, and there are no prominent hallucinations or disorganized thought. The anxiety and behavioral changes (detouring, hiding) are consequences of his delusions.
- The patient's belief that his friends *do not understand* because they were not present at the accident suggests he is trying to rationalize his beliefs and behaviors within his delusional system, which is characteristic of delusional disorder where insight into the delusion is typically absent.
*Avoidant personality disorder*
- Characterized by **social inhibition**, feelings of inadequacy, and **hypersensitivity to negative evaluation**.
- While there is some social withdrawal (hiding from people), his primary motivation is a fear of harm based on fixed beliefs, not a fear of social rejection or embarrassment.
*Schizotypal personality disorder*
- Involves a pervasive pattern of **social and interpersonal deficits** marked by acute discomfort with, and reduced capacity for, close relationships, as well as by **cognitive or perceptual distortions** and eccentricities of behavior.
- This patient does not exhibit the characteristic odd beliefs, magical thinking, unusual perceptual experiences, or eccentric behavior typically seen in schizotypal personality disorder. His thought process is organized, and he denies hallucinations.
*Generalized anxiety disorder*
- Defined by **excessive and uncontrollable worry** about multiple events or activities, often accompanied by physical symptoms like restlessness, fatigue, and muscle tension.
- While the patient experiences anxiety, it is primarily driven by specific, fixed beliefs (delusions) rather than generalized, free-floating worry.
*Acute stress disorder*
- Occurs within **one month of exposure to a traumatic event** and involves dissociative symptoms, intrusion symptoms, negative mood, avoidance symptoms, and arousal symptoms.
- Although he witnessed a traumatic event, the primary features are persistent, non-bizarre delusions rather than a constellation of acute stress symptoms and dissociation. The timeline also extends beyond the typical 1-month duration for acute stress disorder.
Agoraphobia US Medical PG Question 2: A 23-year-old man presents to an outpatient psychiatrist complaining of anxiety and a persistent feeling that “something terrible will happen to my family.” He describes 1 year of vague, disturbing thoughts about his family members contracting a “horrible disease” or dying in an accident. He believes that he can prevent these outcomes by washing his hands of “the contaminants” any time that he touches something and by performing praying and counting rituals each time that he has unwanted, disturbing thoughts. The thoughts and rituals have become more frequent recently, making it impossible for him to work, and he expresses feeling deeply embarrassed by them. Which of the following is the most effective treatment for this patient's disorder?
- A. Psychodynamic psychotherapy and citalopram
- B. Cognitive behavioral therapy and haloperidol
- C. Cognitive behavioral therapy and clonazepam
- D. Cognitive behavioral therapy and fluoxetine (Correct Answer)
- E. Psychodynamic psychotherapy and aripiprazole
Agoraphobia Explanation: ***Cognitive behavioral therapy and fluoxetine***
- This patient presents with symptoms highly suggestive of **obsessive-compulsive disorder (OCD)**, characterized by intrusive, distressing thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed to neutralize the anxiety.
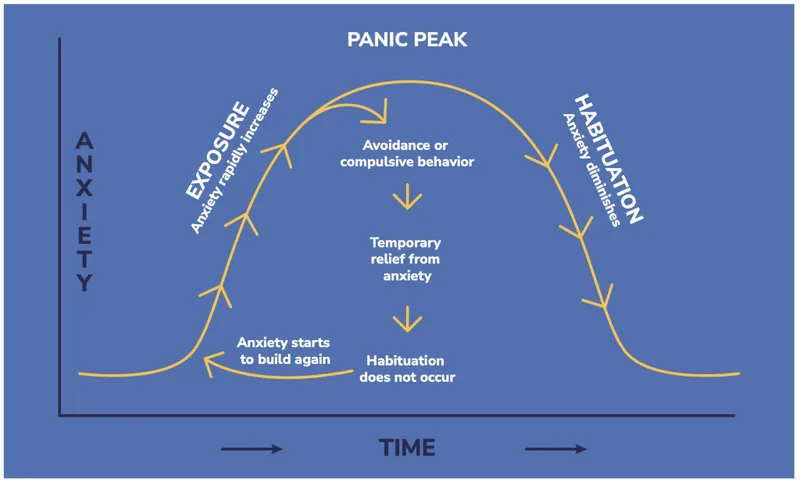
- **Cognitive Behavioral Therapy (CBT)**, specifically Exposure and Response Prevention (ERP), is the most effective psychotherapy for OCD, and **SSRIs** like fluoxetine are the first-line pharmacotherapy.
*Psychodynamic psychotherapy and citalopram*
- While citalopram (an SSRI) is an appropriate pharmacological treatment for OCD, **psychodynamic psychotherapy** is generally not considered first-line or most effective for OCD due to its focus on unconscious conflicts rather than direct symptom reduction.
- This approach may not provide the structured, symptom-focused interventions needed to manage obsessions and compulsions effectively.
*Cognitive behavioral therapy and haloperidol*
- **CBT** is an excellent choice, but **haloperidol**, an antipsychotic, is not a first-line treatment for OCD; it is primarily used for psychotic disorders or as an augmentation strategy in severe, treatment-resistant OCD, which is not indicated here.
- Using an antipsychotic as a primary treatment for OCD without a clear indication of psychosis or severe non-response to SSRIs is inappropriate and can lead to unnecessary side effects.
*Cognitive behavioral therapy and clonazepam*
- **CBT** is appropriate, but **clonazepam**, a benzodiazepine, is generally not recommended as a monotherapy or primary adjunctive treatment for OCD due to its *sedative side effects*, *potential for dependence*, and *lack of efficacy* in addressing the core symptoms of OCD.
- Benzodiazepines may be used for short-term anxiety relief but do not treat the underlying obsessive-compulsive processes.
*Psychodynamic psychotherapy and aripiprazole*
- **Psychodynamic psychotherapy** is not the most effective approach for OCD.
- **Aripiprazole**, an atypical antipsychotic, is typically used as an augmentation strategy for *treatment-resistant OCD* when initial SSRI trials have failed, not as a first-line medication, and this patient's case does not describe treatment resistance.
Agoraphobia US Medical PG Question 3: A 45-year-old woman presents to her primary care physician with complaints of muscle pains, poor sleep, and daytime fatigue. When asked about stressors she states that she "panics" about her job, marriage, children, and finances. When asked to clarify what the "panics" entail, she states that it involves severe worrying. She has had these symptoms since she last saw you one year ago. What is the most likely diagnosis?
- A. Generalized anxiety disorder (Correct Answer)
- B. Social phobia
- C. Adjustment disorder
- D. Obsessive-compulsive disorder
- E. Panic disorder
Agoraphobia Explanation: ***Generalized anxiety disorder***
- This patient presents with **chronic, excessive, and uncontrollable worry** about multiple life circumstances (job, marriage, children, finances), fulfilling the core diagnostic criterion for GAD.
- The associated symptoms of **muscle pains**, **poor sleep**, and **daytime fatigue** are common physical manifestations of GAD, and the duration of symptoms for over a year supports the diagnosis.
*Social phobia*
- **Social phobia**, or social anxiety disorder, involves intense fear and anxiety in **social situations** where one might be scrutinized or judged.
- The patient's reported worries are broad and not limited to social interactions, making social phobia less likely.
*Adjustment disorder*
- **Adjustment disorder** is characterized by emotional or behavioral symptoms developing within **three months of an identifiable stressor**, not diffuse chronic worry.
- The symptoms in adjustment disorder typically resolve within **six months** after the stressor or its consequences have ended, whereas this patient's symptoms are chronic and pervasive.
*Obsessive-compulsive disorder*
- **Obsessive-compulsive disorder (OCD)** involves recurrent, intrusive **obsessions** (thoughts, urges, images) and/or **compulsions** (repetitive behaviors or mental acts) performed to reduce anxiety.
- While the patient experiences severe worrying, there's no mention of specific obsessions or compulsive behaviors aimed at neutralizing those anxieties.
*Panic disorder*
- **Panic disorder** is characterized by recurrent, unexpected **panic attacks**—sudden surges of intense fear or discomfort accompanied by physical and cognitive symptoms.
- While the patient uses the term "panics," she clarifies it involves "severe worrying," not discrete, intense, and short-lived panic attacks.
Agoraphobia US Medical PG Question 4: A 35-year-old man comes to the Veterans Affairs hospital because of a 2-month history of anxiety. He recently returned from his third deployment to Iraq, where he served as a combat medic. He has had difficulty readjusting to civilian life. He works as a taxi driver but had to take a leave of absence because of difficulties with driving. Last week, he hit a stop sign because he swerved out of the way of a grocery bag that was in the street. He has difficulty sleeping because of nightmares about the deaths of some of the other soldiers in his unit and states, “it's my fault, I could have saved them. Please help me.” Mental status examination shows a depressed mood and a restricted affect. There is no evidence of suicidal ideation. Which of the following is the most appropriate initial step in treatment?
- A. Dialectical behavioral therapy
- B. Venlafaxine therapy
- C. Cognitive behavioral therapy (Correct Answer)
- D. Motivational interviewing
- E. Prazosin therapy
Agoraphobia Explanation: ***Cognitive behavioral therapy***
- **Cognitive Behavioral Therapy (CBT)** is considered a first-line psychological treatment for **Post-Traumatic Stress Disorder (PTSD)**, which the patient's symptoms (deployments, intrusive thoughts, nightmares, avoidance, guilt) strongly suggest.
- CBT helps individuals identify and challenge **maladaptive thought patterns** and behaviors related to the trauma, fostering new coping mechanisms.
*Dialectical behavioral therapy*
- **Dialectical Behavioral Therapy (DBT)** is primarily used for individuals with **Borderline Personality Disorder** or severe emotional dysregulation.
- While it can help with emotional regulation, it is not the **first-line therapy** specifically targeting trauma-related cognitive distortions and avoidance behaviors seen in PTSD.
*Venlafaxine therapy*
- **Venlafaxine**, an SNRI, is an antidepressant that can be effective for PTSD symptoms. However, current guidelines recommend **psychotherapy (like CBT)** as the initial step, especially when feasible.
- While pharmacotherapy can be used, it's typically considered **adjunctive** or for cases where psychotherapy alone is insufficient or not preferred.
*Motivational interviewing*
- **Motivational interviewing** is a patient-centered counseling style used to address ambivalence and enhance a person's **intrinsic motivation** for change.
- It is often utilized in substance abuse treatment or when patients are resistant to treatment, but it is not a primary, standalone treatment for the core symptoms of PTSD.
*Prazosin therapy*
- **Prazosin** is an alpha-1 antagonist used off-label to treat **PTSD-related nightmares** and sleep disturbances.
- While it can be helpful for a specific symptom, it does not address the broader spectrum of PTSD symptoms, such as intrusive thoughts, avoidance, or negative cognitions.
Agoraphobia US Medical PG Question 5: A 27-year-old man is brought to a psychiatrist by his mother who is concerned that he has become increasingly distant. When asked, he says that he is no longer going out because he is afraid of going outside by himself. He says that ever since he was a teenager, he was uncomfortable in large crowds and on public transportation. He now works from home and rarely leaves his house except on mandatory business. Which of the following personality disorders is most likely genetically associated with this patient's disorder?
- A. Dependent
- B. Schizotypal
- C. Histrionic
- D. Antisocial
- E. Paranoid
- F. Avoidant (Correct Answer)
Agoraphobia Explanation: ***Avoidant***
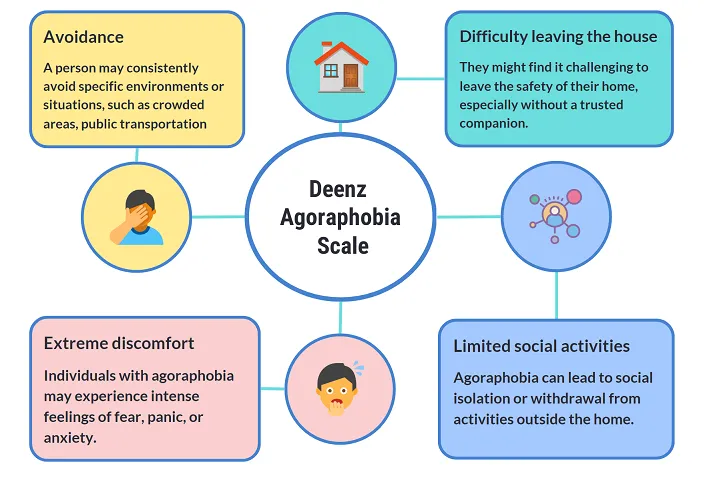
- This patient exhibits symptoms consistent with **agoraphobia**, which is an **anxiety disorder** characterized by fear of situations where escape might be difficult or help unavailable, often leading to social isolation.
- **Avoidant Personality Disorder** has the strongest genetic association with anxiety disorders, particularly **social anxiety disorder and agoraphobia**, sharing common genetic vulnerability factors related to fear of negative evaluation and social avoidance.
- Studies demonstrate significant genetic overlap between avoidant personality disorder and anxiety spectrum disorders, making this the most likely genetically associated personality disorder.
*Schizotypal*
- **Schizotypal Personality Disorder** is genetically linked to the **schizophrenia spectrum** (not anxiety disorders), characterized by cognitive-perceptual distortions, eccentric behavior, and social deficits.
- While schizotypal patients may avoid social situations, this is due to odd thinking and discomfort with close relationships, not anxiety about specific situations like crowds or public transportation.
*Dependent*
- **Dependent Personality Disorder** is characterized by an excessive need to be taken care of, leading to **submissive and clinging behavior**, and fears of separation.
- This patient's withdrawal is due to fear of public places, not a reliance on others or fear of abandonment.
*Antisocial*
- **Antisocial Personality Disorder** involves a pervasive pattern of **disregard for and violation of the rights of others**, often presenting as deceitful and impulsive behavior.
- The patient's symptoms are rooted in anxiety and social avoidance rather than a lack of empathy or antisocial behavior.
*Paranoid*
- **Paranoid Personality Disorder** is characterized by a pervasive **distrust and suspiciousness of others**, interpreting their motives as malevolent.
- The patient's withdrawal stems from fear of specific situations (crowds, public transport) rather than paranoid ideation or general suspicion of people's intentions.
*Histrionic*
- **Histrionic Personality Disorder** is marked by **excessive emotionality and attention-seeking behavior**, often displaying dramatic and superficial interactions.
- The patient's isolation and fear of public spaces are directly opposite to the attention-seeking nature of histrionic traits.
Agoraphobia US Medical PG Question 6: A 24-year-old woman comes to the physician because of a 1-year history of intermittent episodes of shortness of breath, chest tightness, palpitation, dizziness, sweaty hands, and a feeling of impending doom. She says that her symptoms occur when she goes for a walk or waits in line for coffee. She reports that she no longer leaves the house by herself because she is afraid of being alone when her symptoms occur. She only goes out when her boyfriend accompanies her. She does not smoke or use illicit drugs. Within a few hours after each episode, physical examination and laboratory studies have shown no abnormalities. Which of the following is the most likely diagnosis?
- A. Separation anxiety disorder
- B. Generalized anxiety disorder
- C. Agoraphobia (Correct Answer)
- D. Panic disorder
- E. Somatic symptom disorder
Agoraphobia Explanation: ***Agoraphobia***
- The patient's avoidance of leaving the house alone due to fear of symptom recurrence in various situations (e.g., walking, waiting in line), and her reliance on her boyfriend's presence, are classic symptoms of **agoraphobia**.
- Agoraphobia typically involves marked fear or anxiety about being in situations from which escape might be difficult or embarrassing, or in which help might not be available in the event of panic-like symptoms.
- The key feature here is the **pervasive avoidance behavior** that significantly restricts her independence and daily functioning.
*Separation anxiety disorder*
- This disorder is characterized by excessive anxiety concerning separation from home or from those to whom the individual is attached.
- While the patient avoids leaving home, her anxiety is not specifically about separating from an attachment figure, but rather about being alone when panic-like symptoms might occur in situations where escape or help is unavailable.
*Generalized anxiety disorder*
- Generalized anxiety disorder involves persistent and excessive worry about multiple everyday events or activities for at least six months.
- The patient's symptoms are episodic and specifically triggered by certain situations with agoraphobic features, rather than a constant, diffuse worry about various life circumstances.
*Panic disorder*
- Panic disorder is characterized by recurrent, unexpected panic attacks and persistent worry about additional attacks or their consequences.
- While the patient clearly experiences panic attacks, panic disorder alone does not fully explain the **extensive avoidance behavior** and dependence on a companion for routine activities.
- In DSM-5, agoraphobia and panic disorder can co-occur, but when the predominant clinical feature is the situational avoidance and restriction of independence (as seen here), agoraphobia is the more complete diagnosis.
*Somatic symptom disorder*
- This disorder involves one or more somatic symptoms that are distressing or result in significant disruption of daily life, accompanied by excessive thoughts, feelings, or behaviors related to the symptoms.
- Although the patient's physical symptoms are distressing, the primary issue is the fear and avoidance of specific situations where help might not be available, not a preoccupation with the somatic symptoms themselves or excessive healthcare utilization.
Agoraphobia US Medical PG Question 7: A 14-year-old girl presents to the pediatrician for behavior issues. The girl has been having difficulty in school as a result. Every time the girl enters her classroom, she feels the urge to touch every wall before heading to her seat. When asked why she does this, she responds, "I'm not really sure. I just can't stop thinking about it until I have touched each wall." The parents have noticed this behavior occasionally at home but were not concerned. The girl is otherwise healthy, has many friends, eats a balanced diet, does not smoke, and is not sexually active. Her temperature is 98.2°F (36.8°C), blood pressure is 117/74 mmHg, pulse is 80/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam is notable for a healthy young girl. Neurologic exam is unremarkable. There is no observed abnormalities in behavior while the girl is in the office. Which of the following is the most appropriate initial step in management for this patient?
- A. Cognitive behavioral therapy (Correct Answer)
- B. Lorazepam
- C. Risperidone
- D. Clomipramine
- E. Fluoxetine
Agoraphobia Explanation: ***Cognitive behavioral therapy***
- This patient exhibits classic symptoms of **obsessive-compulsive disorder (OCD)**, characterized by intrusive thoughts (obsessions) and repetitive behaviors (compulsions) performed to alleviate anxiety.
- **Exposure and response prevention (ERP)**, a component of cognitive behavioral therapy, is the first-line psychosocial treatment for OCD and has strong evidence for its efficacy in both children and adults.
*Lorazepam*
- **Lorazepam** is a benzodiazepine used for acute anxiety or panic attacks, providing short-term relief.
- It is not a primary treatment for OCD and does not address the underlying obsessive-compulsive cycle; long-term use can lead to dependence.
*Risperidone*
- **Risperidone** is an atypical antipsychotic, primarily used for conditions like schizophrenia, bipolar disorder, or severe behavioral disturbances.
- While sometimes used as an augmentation strategy in refractory OCD, it is not a first-line treatment, especially without prior trials of CBT or SSRIs.
*Clomipramine*
- **Clomipramine** is a tricyclic antidepressant (TCA) with potent serotonin reuptake inhibition, making it effective for OCD.
- However, due to its less favorable side effect profile compared to selective serotonin reuptake inhibitors (SSRIs), it is typically reserved for cases where SSRIs are ineffective.
*Fluoxetine*
- **Fluoxetine** is an SSRI, a first-line pharmacologic treatment for OCD.
- While effective, current guidelines recommend starting with **CBT (specifically ERP)** as the initial treatment for mild to moderate OCD, or combining it with medication for more severe cases.
Agoraphobia US Medical PG Question 8: A previously healthy 36-year-old man is brought to the physician by a friend because of fatigue and a depressed mood for the past few weeks. During this time, he has not been going to work and did not show up to meet his friends for two bowling nights. The friend is concerned that he may lose his job. He spends most of his time alone at home watching television on the couch. He has been waking up often at night and sometimes takes 20 minutes to go back to sleep. He has also been drinking half a pint of whiskey per day for 1 week. His wife left him 4 weeks ago and moved out of their house. His vital signs are within normal limits. On mental status examination, he is oriented to person, place and time. He displays a flattened affect and says that he “doesn't know how he can live without his wife.” He denies suicidal ideation. Which of the following is the next appropriate step in management?
- A. Prescribe a short course of alprazolam
- B. Hospitalize the patient
- C. Initiate cognitive behavioral therapy (Correct Answer)
- D. Initiate disulfiram therapy
- E. Prescribe a short course of duloxetine
Agoraphobia Explanation: ***Initiate cognitive behavioral therapy***
- The patient exhibits features of **adjustment disorder with depressed mood**, characterized by significant distress or impairment in functioning in response to an identifiable stressor (wife leaving).
- **Cognitive behavioral therapy (CBT)** is an effective first-line treatment for adjustment disorders, helping patients develop coping strategies and restructure negative thought patterns.
*Prescribe a short course of alprazolam*
- **Alprazolam**, a benzodiazepine, can provide temporary relief for anxiety but does not address the underlying issues of adjustment disorder and carries risks of **dependence** and withdrawal.
- It would be inappropriate as a sole initial treatment and could exacerbate his **alcohol use**.
*Hospitalize the patient*
- The patient denies **suicidal ideation** and does not present with acute psychosis or severe impairment that would warrant **hospitalization**.
- His orientation and ability to engage in conversation further suggest an outpatient approach is safe and appropriate.
*Initiate disulfiram therapy*
- **Disulfiram** is used for alcohol dependence to deter drinking, but the patient's current alcohol use is a recent development in response to stress, not necessarily full-blown **alcohol dependence** requiring disulfiram.
- Addressing the underlying **adjustment disorder** is the priority, which may in turn reduce his alcohol consumption.
*Prescribe a short course of duloxetine*
- **Duloxetine** is an antidepressant that is not indicated for **adjustment disorder** as a first-line treatment, especially given the short duration and clear precipitating factor.
- **Psychotherapy**, like CBT, is generally the preferred initial intervention for adjustment disorders.
Agoraphobia US Medical PG Question 9: A 36-year-old woman comes to the physician because of an 8-month history of occasional tremor. The tremor is accompanied by sudden restlessness and nausea, which disrupts her daily work as a professional violinist. The symptoms worsen shortly before upcoming concerts but also appear when she goes for a walk in the city. She is concerned that she might have a neurological illness and have to give up her career. The patient experiences difficulty falling asleep because she cannot stop worrying that a burglar might break into her house. Her appetite is good. She drinks one glass of wine before performances "to calm her nerves" and otherwise drinks 2–3 glasses of wine per week. The patient takes daily multivitamins as prescribed. She appears nervous. Her temperature is 36.8°C (98.2°F), pulse is 92/min, and blood pressure is 135/80 mm Hg. Mental status examination shows a full range of affect. On examination, a fine tremor on both hands is noted. She exhibits muscle tension. The remainder of the neurological exam shows no abnormalities. Which of the following is the most likely explanation for this patient's symptoms?
- A. Atypical depressive disorder
- B. Adjustment disorder
- C. Generalized anxiety disorder (Correct Answer)
- D. Panic disorder
- E. Essential tremor
Agoraphobia Explanation: ***Generalized anxiety disorder***
- The patient exhibits persistent and excessive worry about various life circumstances (performance, burglaries, general anxiety), accompanied by physical symptoms like **restlessness**, muscle tension, and sleep disturbances, which are hallmark features of **Generalized Anxiety Disorder (GAD)**.
- The symptoms have been present for **8 months**, exceed the diagnostic duration for GAD (at least 6 months), and are not clearly tied to a specific stressor or episodic panic attacks.
*Atypical depressive disorder*
- Atypical depression is characterized by mood reactivity, increased appetite/weight gain, hypersomnia, leaden paralysis, and interpersonal rejection sensitivity.
- This patient reports difficulty sleeping (*insomnia*) and primarily presents with anxiety symptoms, not depressive mood.
*Adjustment disorder*
- **Adjustment disorder** involves emotional or behavioral symptoms in response to an identifiable stressor, occurring within 3 months of the stressor's onset, and usually resolving within 6 months after the stressor or its consequences have ceased.
- The patient's symptoms are chronic (8 months), excessive, and not solely linked to *one* identifiable recent stressor, but rather a pervasive pattern of worry.
*Panic disorder*
- **Panic disorder** is characterized by recurrent unexpected **panic attacks** with sudden onset of intense fear and physical symptoms (e.g., palpitations, dyspnea, dizziness).
- While she experiences sudden restlessness and nausea related to performances, these are specific triggers and not unexpected, unprovoked panic attacks. The primary pattern is persistent worry, not recurrent panic attacks.
*Essential tremor*
- **Essential tremor** is a neurological condition causing an *action tremor*, often visible when performing daily tasks, and typically improves with alcohol.
- While she has a tremor that improves with alcohol, the presence of marked and pervasive psychological symptoms like severe worrying, restlessness, and insomnia point to an underlying anxiety disorder, not solely an isolated neurological tremor.
Agoraphobia US Medical PG Question 10: A 36-year-old woman complains of difficulty falling asleep over the past 4 months. On detailed history taking, she says that she drinks her last cup of tea at 8:30 p.m. before retiring at 10:30 p.m. She then watches the time on her cell phone on and off for an hour before falling asleep. In the morning, she is tired and makes mistakes at work. Her husband has not noticed excessive snoring or abnormal breathing during sleep. Medical history is unremarkable. She has smoked 5–7 cigarettes daily for 7 years and denies excess alcohol consumption. Her physical examination is normal. Which of the following is the best initial step in the management of this patient’s condition?
- A. Ropinirole
- B. Continuous positive airway pressure
- C. Modafinil
- D. Paroxetine
- E. Proper sleep hygiene (Correct Answer)
Agoraphobia Explanation: ***Proper sleep hygiene***
- The patient's history of difficulty falling asleep, using a cell phone before bed, and tea consumption close to bedtime points towards **poor sleep hygiene** as a primary contributor to her insomnia.
- Addressing these behavioral factors first with **sleep hygiene education** is the most appropriate initial step before considering pharmacologic interventions.
*Ropinirole*
- **Ropinirole** is a dopamine agonist primarily used to treat **Parkinson's disease** and **restless legs syndrome**.
- There are no indications in the patient's presentation, such as an irresistible urge to move the legs, that would suggest restless legs syndrome.
*Continuous positive airway pressure*
- **Continuous positive airway pressure (CPAP)** is the standard treatment for **obstructive sleep apnea (OSA)**.
- The patient's husband has not noticed snoring or abnormal breathing during sleep, making OSA less likely as the primary cause of her insomnia.
*Modafinil*
- **Modafinil** is a wakefulness-promoting agent used to treat **narcolepsy** and other disorders characterized by excessive daytime sleepiness.
- The patient's primary complaint is difficulty *falling asleep* (**insomnia**), not excessive daytime sleepiness, and there's no evidence of narcolepsy.
*Paroxetine*
- **Paroxetine** is a selective serotonin reuptake inhibitor (SSRI) used to treat **depression** and **anxiety disorders**, and sometimes insomnia associated with these conditions.
- There is no mention of symptoms of depression or anxiety in the patient's history that would warrant immediate antidepressant use for her sleep difficulties.
More Agoraphobia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.