Anxiety

On this page
🧠 The Anxiety Architecture: Decoding the Mind's Alarm System
Anxiety disorders affect nearly one in three people during their lifetime, yet they remain among the most treatable psychiatric conditions when properly understood. You'll master the neurocircuitry driving pathological fear responses, distinguish seven distinct clinical phenotypes through pattern recognition, and deploy evidence-based interventions ranging from first-line SSRIs to exposure-based psychotherapy. This lesson builds your diagnostic precision through structured assessment tools, then equips you with treatment algorithms that integrate pharmacology, psychotherapy, and systems-based care. By synthesizing neurobiological mechanisms with clinical decision-making, you'll transform anxiety from a vague complaint into a precisely managed condition.
The anxiety spectrum encompasses 8 major disorder categories affecting 40 million adults annually in the United States, with lifetime prevalence rates reaching 28.8%. These conditions represent the most common psychiatric disorders, yet their underlying mechanisms remain among the most sophisticated examples of neural circuit dysfunction.
📌 Remember: FEAR-GASO - Fear circuits, Endocrine dysregulation, Autonomic hyperactivity, Risk factors, Genetic predisposition, Avoidance behaviors, Sympathetic overdrive, Outcome impairment. These eight domains capture the multisystem nature of anxiety pathophysiology.
- Neurobiological Foundation
- Amygdala hyperactivation: 300% increased activity during threat processing
- Prefrontal cortex dysfunction: 40-60% reduced inhibitory control
- Anterior cingulate cortex: emotional regulation center
- Ventromedial prefrontal cortex: fear extinction processing
- Dorsolateral prefrontal cortex: cognitive control mechanisms
- Neurotransmitter Systems
- GABA deficiency: 25-40% reduced inhibitory signaling
- Serotonin dysregulation: 5-HT1A receptor downregulation
- Norepinephrine excess: 2-3x elevated baseline levels
- Dopamine imbalance: reward circuit dysfunction
⭐ Clinical Pearl: Anxiety disorders show 60-80% heritability rates, with first-degree relatives having 4-6x increased risk. The 5-HTTLPR polymorphism affects serotonin transporter function, predisposing to anxiety in 40% of carriers exposed to early life stress.
| Disorder Type | Prevalence | Age of Onset | Genetic Loading | Comorbidity Rate | Treatment Response |
|---|---|---|---|---|---|
| Generalized Anxiety | 3.1% | 31 years | 32% heritability | 90% any disorder | 70% CBT response |
| Panic Disorder | 2.7% | 24 years | 48% heritability | 85% depression | 80% medication response |
| Social Anxiety | 7.1% | 13 years | 51% heritability | 70% depression | 75% combined treatment |
| Specific Phobias | 9.1% | 7 years | 25-35% heritability | 60% other anxiety | 85% exposure therapy |
| Agoraphobia | 1.3% | 20 years | 61% heritability | 95% panic disorder | 65% treatment response |
Connect these foundational anxiety mechanisms through neurobiological circuit analysis to understand how specific brain regions orchestrate the complex symphony of anxiety symptoms.
🧠 The Anxiety Architecture: Decoding the Mind's Alarm System
⚡ Neural Circuit Mastery: The Fear Network Command Center
📌 Remember: AMYGDALA-PFC - Alarm system, Memory consolidation, Yield to emotions, Generates fear, Direct threat response, Automatic processing, Limbic activation, Arousal increase. Prefrontal Fear Control through cognitive regulation, extinction learning, and executive override.
- Amygdala Complex Architecture
- Basolateral nucleus: threat evaluation and fear learning
- Central nucleus: autonomic output and behavioral responses
- Projects to hypothalamus: HPA axis activation
- Connects to brainstem: startle response and respiratory changes
- Links to periaqueductal gray: freezing behaviors
- Prefrontal Regulatory Systems
- Ventromedial PFC: fear extinction and safety learning
- Anterior cingulate: conflict monitoring and emotional regulation
- Dorsal ACC: cognitive control (40-60% reduced in anxiety)
- Rostral ACC: emotional processing and empathy
⭐ Clinical Pearl: Fear extinction deficits characterize most anxiety disorders, with 50-70% impaired extinction recall. The vmPFC-amygdala connectivity shows 30-40% reduced coupling in PTSD and panic disorder, explaining why exposure therapy requires 12-16 sessions for optimal fear memory reconsolidation.
| Circuit Component | Normal Function | Anxiety Dysfunction | Neurotransmitter | Medication Target | Recovery Timeline |
|---|---|---|---|---|---|
| Amygdala | Threat detection | 300% hyperactivity | GABA/Glutamate | Benzodiazepines | 2-4 weeks |
| vmPFC | Fear extinction | 60% hypoactivity | Serotonin | SSRIs | 6-8 weeks |
| Hippocampus | Context memory | 25% volume loss | Norepinephrine | SNRIs | 8-12 weeks |
| Anterior Cingulate | Conflict monitoring | 40% dysfunction | Dopamine | Atypicals | 4-6 weeks |
| Insula | Interoception | 200% hyperactivity | Multiple systems | Combined therapy | 12-16 weeks |
Connect these circuit mechanisms through pattern recognition frameworks to understand how different anxiety presentations emerge from specific neural network dysfunctions.
⚡ Neural Circuit Mastery: The Fear Network Command Center
🎯 Pattern Recognition Mastery: The Clinical Phenotype Matrix
📌 Remember: PANIC-GASO - Physical symptoms, Avoidance patterns, Neurovegetative signs, Impairment severity, Cognitive distortions. Generalized worry, Anticipatory anxiety, Social fears, Obsessive thoughts. This framework captures the core domains for systematic anxiety assessment.
- Temporal Pattern Recognition
- Acute episodic: Panic attacks (4-10 minutes peak intensity)
- Chronic persistent: GAD (6+ months duration requirement)
- Social anxiety: performance-specific vs generalized social fear
- Specific phobias: immediate response (<5 seconds onset)
- Agoraphobia: anticipatory anxiety (hours to days before exposure)
- Somatic Signature Patterns
- Cardiovascular: Palpitations (80-90% panic disorder)
- Respiratory: Dyspnea (70-85% panic attacks)
- Gastrointestinal: Nausea (60-75% generalized anxiety)
- Neurological: Dizziness (65-80% agoraphobia)
⭐ Clinical Pearl: Panic attack symptoms follow a predictable cascade: initial trigger → 30-60 seconds autonomic surge → 2-4 minutes peak intensity → 10-20 minutes gradual resolution. Anticipatory anxiety develops in 80-90% of patients within 4-6 weeks, creating the panic disorder cycle.
| Disorder | Trigger Pattern | Duration | Peak Intensity | Avoidance Type | Functional Impairment |
|---|---|---|---|---|---|
| Panic Disorder | Unpredictable | 4-10 minutes | Immediate | Situational | 70% work impact |
| GAD | Persistent worry | Chronic (6+ months) | Gradual build | Cognitive | 60% social impact |
| Social Anxiety | Performance cues | Variable | Anticipatory | Social situations | 80% career impact |
| Specific Phobia | Object/situation | Immediate | Instant | Specific triggers | 40% lifestyle impact |
| Agoraphobia | Escape concerns | Persistent | Anticipatory | Multiple situations | 90% mobility impact |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | |||||
| flowchart TD |
Start["🧠 Anxiety Symptoms
• Clinical presentation• Patient assessment"]
Dur["📋 Duration Pattern
• Episodic vs.• Persistent states"]
Trig["📋 Episodic Trigger
• Triggered vs.• Spontaneous onset"]
Scope["📋 Scope of Anxiety
• Generalized vs.• Specific focus"]
Phobia["🩺 Specific Phobia
• Social anxiety• Trigger-dependent"]
Panic["🩺 Panic Disorder
• Recurrent attacks• Unexpected onset"]
GAD["🩺 GAD
• Generalized anxiety• Multi-focus worry"]
Avoid["📋 Avoidance Pattern
• Evaluate behaviors• Situation-specific"]
Agora["🩺 Agoraphobia
• Multiple situations• Fear of escape"]
SocAnx["🩺 Social Anxiety
• Public situations• Fear of scrutiny"]
TxExp["💊 Exposure Therapy
• Desensitization• Targeted approach"]
TxCBT["💊 Panic-focused CBT
• Cognitive therapy• Behavioral control"]
TxGAD["💊 GAD Protocol
• Standard treatment• Management plan"]
Start --> Dur Dur -->|Episodic| Trig Dur -->|Persistent| Scope
Trig -->|Triggered| Phobia Trig -->|Spontaneous| Panic
Scope -->|Generalized| GAD Scope -->|Specific| Avoid
Phobia --> TxExp Panic --> TxCBT GAD --> TxGAD
Avoid -->|Multiple| Agora Avoid -->|Social| SocAnx
style Start fill:#F7F5FD, stroke:#6B21A8, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Dur fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Trig fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Scope fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Avoid fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E
style Phobia fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Panic fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style GAD fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Agora fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style SocAnx fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8
style TxExp fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style TxCBT fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style TxGAD fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534
> 💡 **Master This**: **Comorbidity patterns** provide diagnostic clues: **GAD + Depression** (**60-70%** overlap), **Panic + Agoraphobia** (**40-50%** progression), **Social Anxiety + Substance Use** (**30-40%** self-medication). These combinations require **integrated treatment approaches** with **modified timelines** (**12-16 weeks** vs **8-12 weeks** for single disorders).
Connect these recognition patterns through systematic discrimination frameworks to understand how quantitative assessment tools enhance diagnostic precision and treatment monitoring.
🎯 Pattern Recognition Mastery: The Clinical Phenotype Matrix
🔬 Diagnostic Precision: The Assessment Arsenal
📌 Remember: SCALES-BIO - Structured interviews, Clinician ratings, Assessment tools, Laboratory tests, Exam findings, Self-report measures. Biomarkers, Imaging studies, Objective measurements. This systematic approach ensures comprehensive anxiety evaluation.
- Primary Assessment Instruments
- GAD-7: ≥10 indicates moderate anxiety (89% sensitivity, 82% specificity)
- Beck Anxiety Inventory: ≥16 suggests clinical anxiety (92% sensitivity)
- Hamilton Anxiety Rating Scale: ≥18 moderate, ≥25 severe anxiety
- MINI International Interview: 15-20 minutes structured diagnostic tool
- Panic Disorder Severity Scale: 0-28 range, ≥8 clinically significant
- Biomarker Integration
- Cortisol dysregulation: 150-300% elevated morning levels
- Heart rate variability: 30-50% reduced in chronic anxiety
- Inflammatory markers: IL-6 elevated 2-3x baseline
- Neurotransmitter metabolites: 5-HIAA reduced 20-40%
⭐ Clinical Pearl: Medical screening is essential as 15-25% of anxiety presentations have underlying medical causes. Hyperthyroidism (TSH <0.1), cardiac arrhythmias (Holter monitoring), and substance withdrawal (toxicology screening) must be excluded before psychiatric diagnosis.
| Assessment Tool | Administration Time | Sensitivity | Specificity | Clinical Cutoff | Monitoring Frequency |
|---|---|---|---|---|---|
| GAD-7 | 2-3 minutes | 89% | 82% | ≥10 moderate | Weekly during treatment |
| Beck Anxiety Inventory | 5-10 minutes | 92% | 76% | ≥16 clinical | Bi-weekly |
| Hamilton Anxiety Scale | 15-20 minutes | 85% | 88% | ≥18 moderate | Monthly |
| MINI Interview | 15-20 minutes | 94% | 90% | Diagnostic threshold | Initial assessment |
| Panic Severity Scale | 5 minutes | 88% | 85% | ≥8 significant | Weekly for panic |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | |||||
| flowchart TD |
Start["🧠 Initial Anxiety
• New presentation• Patient intake"]
Flags{"🚩 Medical Red Flags
• Physical signs• Atypical age"}
Workup["🔍 Medical Workup
• Rule out organic• Physical exam"]
PsychAssess["📋 Psych Assessment
• DSM-5 criteria• History review"]
Labs["🔬 Lab Panels
• TSH CBC BMP• Thyroid function"]
Cardiac["🫀 Cardiac Tests
• ECG evaluation• Holter monitor"]
Tox["🧪 Tox Screen
• Substance use• Drug screening"]
Results{"⚖️ Results Normal?
• Data review• Findings check"}
PrimaryDx["🩺 Primary Anxiety
• Idiopathic cause• Psych origin"]
MedicalDx["🩺 Medical Anxiety
• Secondary cause• Organic source"]
PsychRx["💊 Psych Treatment
• SSRI therapy• Psychotherapy"]
MedicalRx["💊 Treat Cause
• Specific therapy• Target illness"]
Start --> Flags Flags -->|Present| Workup Flags -->|Absent| PsychAssess Workup --> Labs Workup --> Cardiac Workup --> Tox Labs --> Results Cardiac --> Results Tox --> Results Results -->|Normal| PrimaryDx Results -->|Abnormal| MedicalDx PrimaryDx --> PsychRx MedicalDx --> MedicalRx
style Start fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Flags fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Workup fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style PsychAssess fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Labs fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Cardiac fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Tox fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Results fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style PrimaryDx fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style MedicalDx fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style PsychRx fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style MedicalRx fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534
> 💡 **Master This**: **Treatment response monitoring** requires **weekly GAD-7 scores** during initial **4-6 weeks**, with **≥50% reduction** indicating treatment response and **≥70% reduction** suggesting remission. **Functional improvement** lags symptom reduction by **2-4 weeks**, requiring **patient education** about expected timelines.
Connect these assessment frameworks through evidence-based treatment algorithms to understand how diagnostic precision guides therapeutic decision-making and outcome optimization.
🔬 Diagnostic Precision: The Assessment Arsenal
💊 Treatment Algorithm Mastery: The Therapeutic Command Center
📌 Remember: SSRI-CBT-COMBO - Selective serotonin reuptake inhibitors first-line, Start low go slow dosing, Response in 6-8 weeks, Increase gradually. Cognitive behavioral therapy gold standard, Behavioral activation essential, Thought challenging core. Combination therapy for severe cases, Outcome monitoring weekly, Maintenance 12+ months, Booster sessions quarterly, Optimize before switching.
- First-Line Pharmacotherapy
- SSRIs: Sertraline 25-200mg, Escitalopram 5-20mg daily
- SNRIs: Venlafaxine XR 37.5-225mg, Duloxetine 30-120mg
- Response rates: 60-70% monotherapy, 80-85% combination
- Time to response: 4-6 weeks initial, 8-12 weeks full benefit
- Maintenance duration: 12-24 months minimum after remission
- Evidence-Based Psychotherapy
- CBT protocols: 12-16 sessions standard course
- Exposure therapy: 8-12 sessions for specific phobias
- Acceptance and Commitment Therapy: 12-16 sessions
- Mindfulness-based interventions: 8-week structured programs
⭐ Clinical Pearl: Combination therapy (medication + CBT) shows superior outcomes with 80-85% response rates vs 60-65% for monotherapy. Sequential treatment (CBT first, then medication if needed) is cost-effective but delays improvement by 4-8 weeks compared to simultaneous initiation.
| Treatment Modality | Response Rate | Time to Response | Relapse Rate | Cost-Effectiveness | Maintenance Required |
|---|---|---|---|---|---|
| SSRI Monotherapy | 60-65% | 6-8 weeks | 40-50% | Moderate | 12-24 months |
| CBT Monotherapy | 65-70% | 8-12 weeks | 20-30% | High | Booster sessions |
| Combination Therapy | 80-85% | 4-6 weeks | 15-25% | Highest | 12+ months |
| Benzodiazepines | 85-90% | 30-60 minutes | 60-80% | Low | Taper required |
| Second-line Options | 50-60% | 6-12 weeks | 35-45% | Variable | Extended |
Connect these treatment algorithms through multi-system integration approaches to understand how comprehensive care addresses the complex interplay between anxiety and comorbid conditions.
💊 Treatment Algorithm Mastery: The Therapeutic Command Center
🌐 Integration Mastery: The Comprehensive Care Network
📌 Remember: TEAM-CARE-PLUS - Team-based approach, Evidence-based protocols, Assessment-driven, Measurement-based care. Comorbidity management, Adherence monitoring, Recovery-oriented, Engagement strategies. Psychosocial factors, Lifestyle interventions, Underserved populations, Specialty integration.
- Comorbidity Integration Patterns
- Anxiety + Depression: 60-70% co-occurrence requiring dual-target treatments
- Anxiety + Substance Use: 30-40% prevalence, integrated treatment essential
- Anxiety + Medical conditions: Diabetes (2-3x higher anxiety rates)
- Anxiety + Chronic pain: 50-60% overlap, shared neural circuits
- Anxiety + Sleep disorders: 75-85% comorbidity, bidirectional relationship
- Cutting-Edge Treatment Innovations
- Digital therapeutics: App-based CBT showing 70-80% efficacy
- Precision medicine: Pharmacogenomic testing improving response rates by 20-30%
- Transcranial stimulation: rTMS for treatment-resistant cases
- Virtual reality exposure: 90%+ efficacy for specific phobias
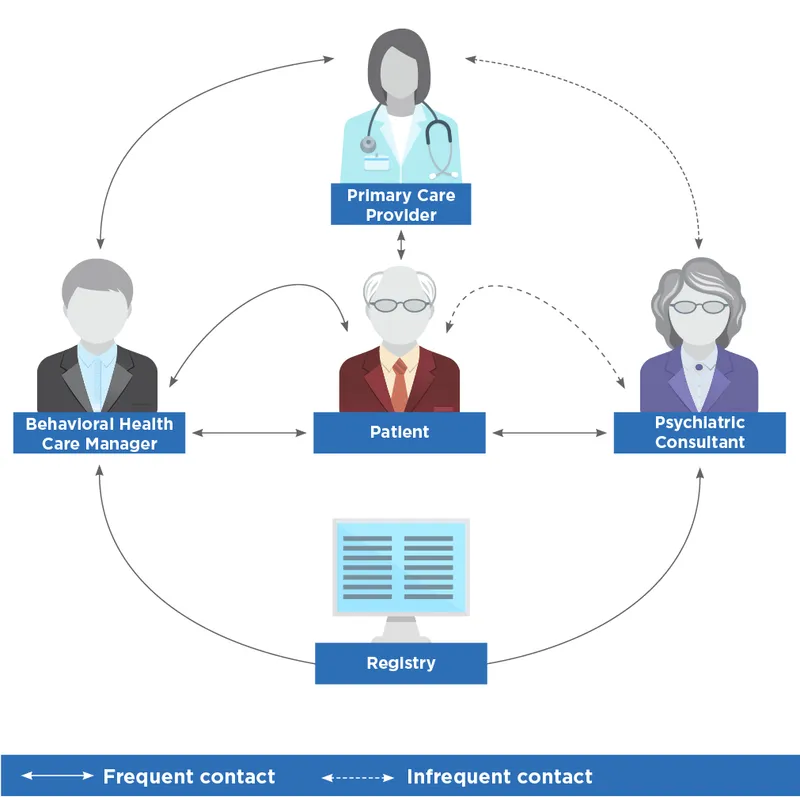
⭐ Clinical Pearl: Collaborative care models improve outcomes by 40-50% compared to usual care, with psychiatric consultants supporting primary care providers through systematic protocols. Measurement-based care with weekly assessments increases remission rates from 45% to 65-70%.
| Integration Domain | Standard Approach | Enhanced Integration | Outcome Improvement | Implementation Cost | Sustainability |
|---|---|---|---|---|---|
| Medical Comorbidity | Separate providers | Integrated clinics | 35-40% better | High initial | High long-term |
| Substance Use | Sequential treatment | Simultaneous care | 50-60% better | Moderate | Moderate |
| Chronic Pain | Independent management | Shared protocols | 45-50% better | Moderate | High |
| Sleep Disorders | Referral-based | Co-located services | 40-45% better | Low | High |
| Social Determinants | Limited addressing | Comprehensive support | 30-35% better | High | Variable |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | |||||
| flowchart TD |
Start["👤 Patient Intake
• Main presentation• Clinical history"]
Assess["📋 Comprehensive
• Full assessment• Initial evaluation"]
Screen{"🔍 Comorbidity
• Screening tool• Identify issues"}
Single["✅ Standard
• Single disorder• Follow protocol"]
Multi["🧩 Integrated
• Multiple issues• Care plan design"]
Team["👥 Team Assign
• Define roles• Multidisciplinary"]
Treat["💊 Coordinated
• Active treatment• Aligned therapy"]
Monitor["👁️ Shared Watch
• Joint monitoring• Progress tracking"]
Resp{"📈 Response
• Assess outcome• Check progress"}
Maint["✅ Maintenance
• Good response• Sustain health"]
Consult["🩺 Consultation
• Poor response• Expert review"]
Mod["🛠️ Modification
• Change protocol• Adjust dosage"]
Start --> Assess Assess --> Screen
Screen -->|Single| Single Screen -->|Multiple| Multi
Multi --> Team Team --> Treat Treat --> Monitor Monitor --> Resp
Resp -->|Good| Maint Resp -->|Poor| Consult Consult --> Mod
style Start fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Assess fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Screen fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Single fill:#F6F5F5, stroke:#E7E6E6, stroke-width:1.5px, rx:12, ry:12, color:#525252 style Multi fill:#EEFAFF, stroke:#DAF3FF, stroke-width:1.5px, rx:12, ry:12, color:#0369A1 style Team fill:#EEFAFF, stroke:#DAF3FF, stroke-width:1.5px, rx:12, ry:12, color:#0369A1 style Treat fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style Monitor fill:#EEFAFF, stroke:#DAF3FF, stroke-width:1.5px, rx:12, ry:12, color:#0369A1 style Resp fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Maint fill:#F6F5F5, stroke:#E7E6E6, stroke-width:1.5px, rx:12, ry:12, color:#525252 style Consult fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Mod fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C
> 💡 **Master This**: **Social determinants** impact anxiety treatment outcomes significantly: **food insecurity** (**2x** higher treatment dropout), **housing instability** (**40-50%** reduced response rates), **transportation barriers** (**30%** missed appointments). **Community health workers** and **peer support specialists** improve **engagement by 25-35%** in underserved populations.
Connect these integration frameworks through rapid mastery tools to understand how systematic approaches enable efficient clinical decision-making and optimal patient outcomes.
🌐 Integration Mastery: The Comprehensive Care Network
🎯 Clinical Mastery Arsenal: The Rapid Response Toolkit
📌 Remember: MASTER-ANXIETY-NOW - Measurement-based care, Assessment protocols, Systematic approach, Treatment algorithms, Evidence-based, Rapid recognition. Acute management, Neurobiological understanding, Xpert consultation, Integrated care, Emergency protocols, Treatment resistance, Yield optimization. Numbers matter, Outcomes tracking, Workflow efficiency.
- Essential Clinical Thresholds
- GAD-7 ≥10: Moderate anxiety requiring active treatment
- Panic frequency ≥4/month: Medication indicated alongside therapy
- Functional impairment ≥50%: Intensive treatment protocols
- Suicidal ideation present: Safety planning and close monitoring
- Substance use comorbidity: Integrated treatment mandatory
- Rapid Assessment Framework
- 2-minute screening: GAD-2 + panic screening questions
- 5-minute evaluation: Severity, impairment, safety, comorbidity
- 15-minute comprehensive: Full diagnostic assessment with treatment planning
- Emergency protocols: Panic attack management, crisis intervention
⭐ Clinical Pearl: Treatment response predictors include early improvement (≥20% reduction by week 2), medication adherence (≥80%), therapy attendance (≥75%), and homework completion (≥60%). Patients meeting 3/4 criteria have 85-90% likelihood of achieving remission.
| Clinical Scenario | Rapid Assessment | First-Line Treatment | Response Timeline | Escalation Trigger | Success Metrics |
|---|---|---|---|---|---|
| Mild GAD | GAD-7: 5-9 | CBT monotherapy | 8-12 weeks | <25% improvement | GAD-7 <5 |
| Moderate GAD | GAD-7: 10-14 | SSRI + CBT | 6-8 weeks | <50% improvement | GAD-7 <7 |
| Severe GAD | GAD-7: 15+ | Combination therapy | 4-6 weeks | <30% improvement | GAD-7 <10 |
| Panic Disorder | Panic frequency | SSRI + panic CBT | 6-8 weeks | Continued attacks | Attack-free |
| Treatment-Resistant | Failed 2+ trials | Augmentation/switch | 8-12 weeks | <25% improvement | Functional return |
🎯 Clinical Mastery Arsenal: The Rapid Response Toolkit
Practice Questions: Anxiety
Test your understanding with these related questions
A 23-year-old man presents to the emergency department with a chief complaint of being assaulted on the street. The patient claims that he has been followed by the government for quite some time and that he was assaulted by a government agent but was able to escape. He often hears voices telling him to hide. The patient has an unknown past medical history and admits to smoking marijuana frequently. On physical exam, the patient has no signs of trauma. When interviewing the patient, he is seen conversing with an external party that is not apparent to you. The patient states that he is afraid for his life and that agents are currently pursuing him. What is the best initial response to this patient’s statement?













