V/Q scan principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for V/Q scan principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
V/Q scan principles US Medical PG Question 1: A 50-year-old man presents to the urgent care clinic for 3 hours of worsening cough, shortness of breath, and dyspnea. He works as a long-haul truck driver, and he informs you that he recently returned to the west coast from a trip to Arkansas. His medical history is significant for gout, hypertension, hypercholesterolemia, diabetes mellitus type 2, chronic obstructive pulmonary disease (COPD), and mild intellectual disability. He currently smokes 1 pack of cigarettes/day, drinks a 6-pack of beer/day, and he endorses a past history of injection drug use but currently denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 23/min. His physical examination shows mild, bilateral, coarse rhonchi, but otherwise clear lungs on auscultation, grade 2/6 holosystolic murmur, and a benign abdominal physical examination. He states that he ran out of his albuterol inhaler 6 days ago and has been meaning to follow-up with his primary care physician (PCP) for a refill. Complete blood count (CBC) and complete metabolic panel are within normal limits. He also has a D-dimer result within normal limits. Which of the following is the most appropriate next step in evaluation?
- A. Chest computed tomography (CT) with contrast
- B. Chest radiographs (Correct Answer)
- C. Pulmonary function tests
- D. Sputum gram stain and culture
- E. Arterial blood gas
V/Q scan principles Explanation: ***Chest radiographs***
- A **chest X-ray** is the most appropriate initial imaging study for evaluating acute respiratory symptoms in a patient with a history of COPD and recent exacerbating factors (running out of albuterol). It can help identify common causes like **pneumonia**, **pneumothorax**, or **acute exacerbation of COPD**.
- The patient's presentation with worsening cough, shortness of breath, and dyspnea, particularly in the context of running out of his albuterol inhaler, suggests a primary pulmonary issue that a chest X-ray can quickly assess.
*Chest computed tomography (CT) with contrast*
- A **chest CT with contrast** is more detailed but not the initial diagnostic study in this scenario, especially with a normal D-dimer ruling out pulmonary embolism as a high probability.
- It exposes the patient to **higher radiation** and risks associated with contrast, making it less suitable as a first-line investigation unless the chest X-ray is inconclusive or more specific findings are suspected.
*Pulmonary function tests*
- **Pulmonary function tests (PFTs)** are used to diagnose and monitor chronic lung conditions like COPD, but they are generally not performed in an acute urgent care setting for patients presenting with acute respiratory distress.
- PFTs require patient cooperation and are designed to assess baseline lung function, not to identify the **acute cause** of respiratory decompensation.
*Sputum gram stain and culture*
- A **sputum gram stain and culture** might be considered if there's strong suspicion of a bacterial infection (e.g., fever, purulent sputum), but the patient's current symptoms are more aligned with a COPD exacerbation or other acute pulmonary issue.
- Without clear signs of bacterial infection, this test is **not the most immediate or appropriate first step** in evaluating acute dyspnea, as it requires time for results and may delay more crucial diagnostic steps.
*Arterial blood gas*
- An **arterial blood gas (ABG)** can provide information on oxygenation, ventilation, and acid-base status, which is useful in assessing the severity of respiratory failure.
- However, it's typically ordered after an initial clinical and imaging assessment to quantify the physiological impact of the respiratory distress, rather than being the **very first diagnostic step** to identify the cause.
V/Q scan principles US Medical PG Question 2: A 60-year-old male is admitted to the ICU for severe hypertension complicated by a headache. The patient has a past medical history of insulin-controlled diabetes, hypertension, and hyperlipidemia. He smokes 2 packs of cigarettes per day. He states that he forgot to take his medications yesterday and started getting a headache about one hour ago. His vitals on admission are the following: blood pressure of 160/110 mmHg, pulse 95/min, temperature 98.6 deg F (37.2 deg C), and respirations 20/min. On exam, the patient has an audible abdominal bruit. After administration of antihypertensive medications, the patient has a blood pressure of 178/120 mmHg. The patient reports his headache has increased to a 10/10 pain level, that he has trouble seeing, and he can't move his extremities. After stabilizing the patient, what is the best next step to diagnose the patient's condition?
- A. Doppler ultrasound of the carotids
- B. CT head with intravenous contrast
- C. MRI head without intravenous contrast
- D. CT head without intravenous contrast (Correct Answer)
- E. MRI head with intravenous contrast
V/Q scan principles Explanation: ***CT head without intravenous contrast***
- The sudden onset of severe headache, visual disturbances, and neurological deficits (inability to move extremities), coupled with uncontrolled severe hypertension despite initial treatment, is highly suggestive of an **intracranial pathology**, most likely a **hemorrhagic stroke**.
- A **non-contrast CT scan of the head** is the **gold standard** for rapidly identifying acute intracranial hemorrhage, as it can be performed quickly and is readily available in emergency settings.
*Doppler ultrasound of the carotids*
- This test is primarily used to evaluate **carotid artery stenosis** due to atherosclerosis, which can lead to ischemic stroke.
- While the patient has risk factors for atherosclerosis, his acute presentation with severe central neurological symptoms points more towards an acute intracranial event rather than carotid disease.
*CT head with intravenous contrast*
- While a contrast CT can be useful for identifying tumors, abscesses, or vascular malformations, it is **contraindicated in the initial assessment of acute stroke** if an intracranial hemorrhage is suspected.
- Contrast can sometimes obscure subtle bleeds or complicate the interpretation of acute hemorrhage, and it also carries a risk of **contrast-induced nephropathy**, especially in a patient with diabetes.
*MRI head without intravenous contrast*
- An MRI provides superior soft tissue resolution compared to CT and is excellent for detecting ischemic strokes in later stages, as well as subtle hemorrhages, tumors, and other conditions.
- However, it is **less available, takes longer to perform**, and is often not the first choice in an acute neurological emergency where time is critical, particularly when differentiating between ischemic and hemorrhagic stroke.
*MRI head with intravenous contrast*
- Similar to a contrast CT, an MRI with contrast is generally **not the initial imaging choice for acute stroke** due to time constraints and the need to quickly rule out hemorrhage before considering contrast administration.
- Contrast agents for MRI, such as gadolinium, have their own risks, including **nephrogenic systemic fibrosis** in patients with renal impairment, which is a concern in a diabetic patient.
V/Q scan principles US Medical PG Question 3: Four days after undergoing an elective total hip replacement, a 65-year-old woman develops a DVT that embolizes to the lung. Along with tachypnea, tachycardia, and cough, the patient would most likely present with a PaO2 of what?
- A. 120 mmHg
- B. 100 mmHg
- C. 85 mmHg (Correct Answer)
- D. 110 mmHg
- E. 60 mmHg
V/Q scan principles Explanation: ***85 mmHg***
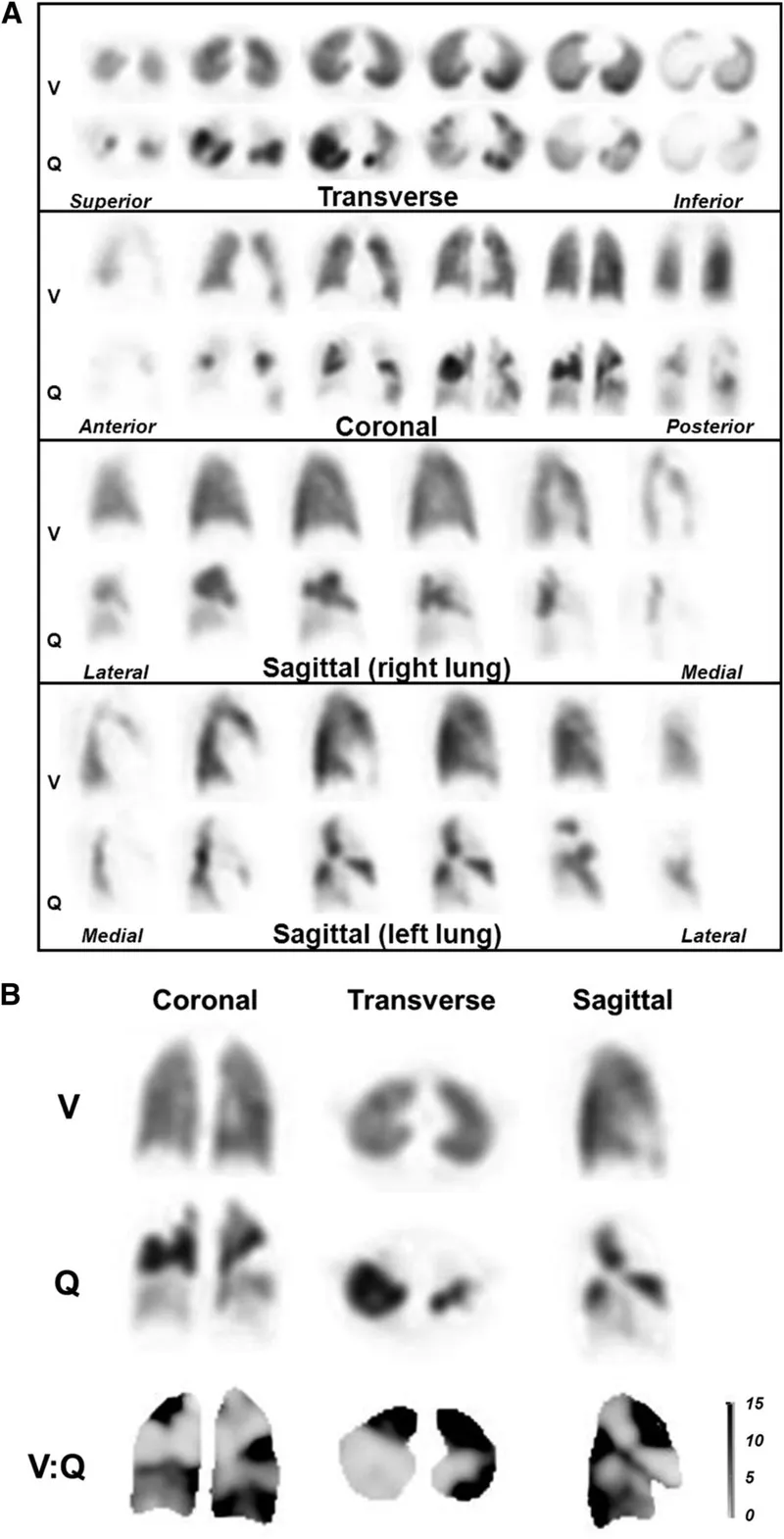
- A pulmonary embolism (PE) causes a **ventilation-perfusion (V/Q) mismatch**, leading to **hypoxemia** and a reduced PaO2.
- While exact values vary, a PaO2 of 85 mmHg indicates **mild to moderate hypoxemia**, which is common in PE, especially with accompanying symptoms like tachypnea and tachycardia.
*120 mmHg*
- This value is significantly **higher than normal (75-100 mmHg)** and would indicate **hyperoxia**, which is inconsistent with acute pulmonary embolism causing respiratory distress.
- A patient with PE would typically have **reduced oxygenation**, not supernormal levels, unless receiving high-flow supplemental oxygen.
*100 mmHg*
- A PaO2 of 100 mmHg is at the **upper end of the normal range** (75-100 mmHg) and would imply **no significant hypoxemia**.
- Given the patient's symptoms of tachypnea, tachycardia, and cough following a DVT with embolization, a normal or high-normal PaO2 is unlikely without aggressive oxygen therapy (which is not stated).
*110 mmHg*
- This value is **above the normal range** and suggests **hyperoxia**, which is contrary to the pathophysiology of a pulmonary embolism.
- A PE impairs gas exchange, leading to a decrease in PaO2, not an increase.
*60 mmHg*
- A PaO2 of 60 mmHg indicates **significant hypoxemia**, which might occur in a severe, large pulmonary embolism or in a patient with underlying lung disease.
- While possible, 85 mmHg represents a more common, moderate hypoxemia seen in PE, especially given the prompt presentation of symptoms.
V/Q scan principles US Medical PG Question 4: A 71-year-old man presents to the emergency department for shortness of breath. The patient was returning from a business trip to China, when he suddenly felt short of breath during the taxi ride home from the airport. The patient has a past medical history of poorly controlled diabetes mellitus and a 50 pack-year smoking history. The patient is non-compliant with his medications and is currently only taking ibuprofen. An initial ECG demonstrates sinus tachycardia. A chest radiograph is within normal limits. Laboratory values are notable for a creatinine of 2.4 mg/dL and a BUN of 32 mg/dL as compared to his baseline creatinine of 0.9 mg/dL. His temperature is 98.8°F (37.1°C), pulse is 122/min, blood pressure is 145/90 mmHg, respirations are 19/min, and oxygen saturation is 93% on room air. On physical exam, you note an older gentleman in distress. Cardiac exam is notable only for tachycardia. Pulmonary exam is notable for expiratory wheezes. Which of the following is the best confirmatory test for this patient?
- A. Ventilation perfusion scan
- B. Lower extremity ultrasound with Doppler
- C. CT angiogram (Correct Answer)
- D. Arterial blood gas
- E. D-dimer
V/Q scan principles Explanation: ***CT angiogram***
- This patient presents with multiple risk factors for **pulmonary embolism (PE)**, including a recent long-haul flight and acute onset of dyspnea with tachycardia and hypoxemia. CT pulmonary angiography (CTPA) is the **gold standard confirmatory test** for PE, directly visualizing thrombi in the pulmonary arteries with high sensitivity (>90%) and specificity.
- While this patient has **acute kidney injury** (creatinine elevated from 0.9 to 2.4 mg/dL), raising concerns about contrast-induced nephropathy, the **high clinical probability of PE** (recent long flight, acute dyspnea, tachycardia, hypoxemia) makes urgent diagnosis critical. In hemodynamically stable patients with intermediate-to-high PE probability and renal insufficiency, CTPA with appropriate precautions (IV hydration, minimizing contrast dose, avoiding nephrotoxic agents) is still preferred as it provides the most definitive diagnosis.
- The patient's hemodynamic stability (BP 145/90) allows time for renal protective measures before contrast administration.
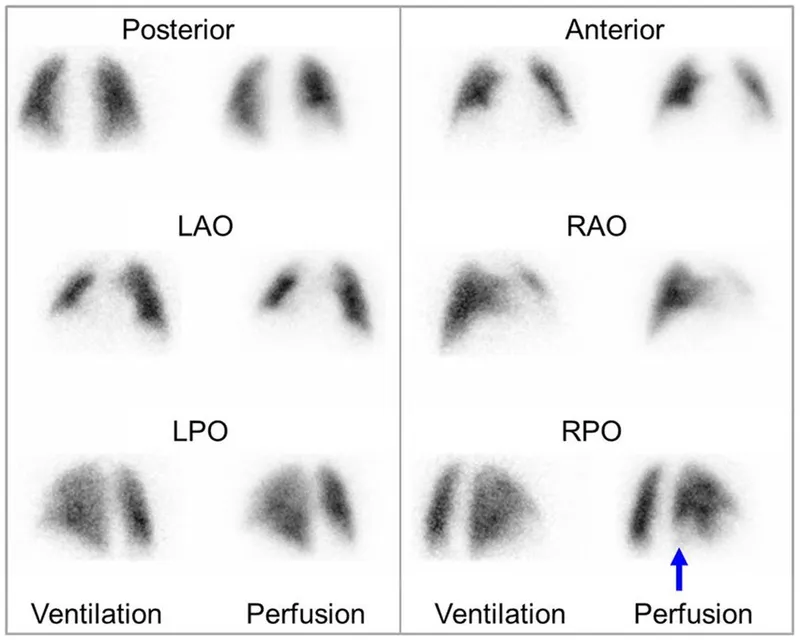
*Ventilation perfusion scan*
- A V/Q scan is an important **alternative** for diagnosing PE, particularly valuable in patients with severe renal insufficiency (CKD Stage 4-5) or contrast allergy where CTPA is truly contraindicated.
- However, in this patient with **expiratory wheezes** suggesting possible underlying obstructive lung disease (50 pack-year smoking history), a V/Q scan has higher likelihood of **indeterminate results** (intermediate probability), which would not confirm or exclude PE and might necessitate additional testing anyway.
- V/Q scans also have lower sensitivity than CTPA and require the patient to cooperate with breathing maneuvers, which may be difficult in an acutely dyspneic patient.
*Lower extremity ultrasound with Doppler*
- This test diagnoses **deep vein thrombosis (DVT)**, the most common source of PE. While a positive DVT in a patient with suspected PE would support treatment, a **negative study does not rule out PE** since the thrombus may have already completely embolized.
- This is a supportive test, not a confirmatory test for PE itself. The patient's symptoms require direct assessment of the pulmonary vasculature.
*Arterial blood gas*
- An ABG typically shows **hypoxemia and respiratory alkalosis** in PE due to V/Q mismatch and hyperventilation, but these findings are **non-specific** and occur in many cardiopulmonary conditions (pneumonia, asthma, COPD exacerbation, heart failure).
- ABG is a supportive tool that may guide oxygen therapy but does not confirm PE diagnosis.
*D-dimer*
- D-dimer has excellent **negative predictive value** and is useful to exclude PE in patients with **low clinical probability** (Wells score <2 or PERC rule negative).
- In this patient with **high clinical probability** of PE (recent long flight, acute symptoms, risk factors), D-dimer would almost certainly be elevated and thus **not helpful for confirmation**. Elevated D-dimer occurs in many conditions including infection, inflammation, malignancy, recent surgery, and advanced age, making it non-specific in this context.
V/Q scan principles US Medical PG Question 5: A 72-year-old man with coronary artery disease comes to the emergency department because of chest pain and shortness of breath for the past 3 hours. Troponin levels are elevated and an ECG shows ST-elevations in the precordial leads. Revascularization with percutaneous coronary intervention is performed, and a stent is successfully placed in the left anterior descending artery. Two days later, he complains of worsening shortness of breath. Pulse oximetry on 3L of nasal cannula shows an oxygen saturation of 89%. An x-ray of the chest shows distended pulmonary veins, small horizontal lines at the lung bases, and blunting of the costophrenic angles bilaterally. Which of the following findings would be most likely on a ventilation-perfusion scan of this patient?
- A. Matched ventilation and perfusion bilaterally
- B. Normal ventilation with multiple, bilateral perfusion defects
- C. Normal perfusion with bilateral ventilation defects (Correct Answer)
- D. Normal perfusion with decreased ventilation at the right base
- E. Increased apical ventilation with normal perfusion bilaterally
V/Q scan principles Explanation: ***Normal perfusion with bilateral ventilation defects***
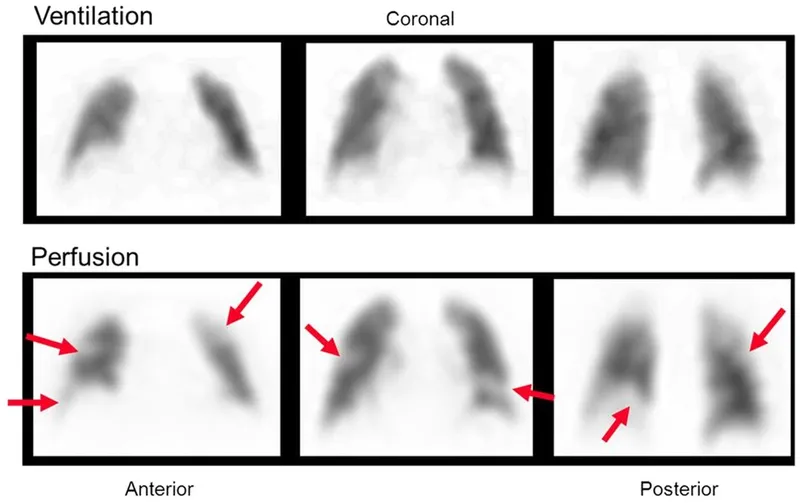
- The patient's presentation with **worsening shortness of breath** after an acute coronary event, along with chest x-ray findings of **distended pulmonary veins, Kerley B lines (small horizontal lines at the lung bases), and blunting of the costophrenic angles**, is highly suggestive of **pulmonary edema** due to heart failure.
- In pulmonary edema, the alveoli fill with fluid, impeding gas exchange. This leads to **impaired ventilation** in the affected areas, while **pulmonary blood flow (perfusion) remains intact**. This results in **ventilation-perfusion (V/Q) mismatch** with impaired ventilation.
*Matched ventilation and perfusion bilaterally*
- This pattern would indicate a **normal ventilation-perfusion scan**, which is inconsistent with the patient's severe shortness of breath, hypoxemia, and radiographic signs of pulmonary edema.
- A matched V/Q scan suggests **healthy lung function** and gas exchange.
*Normal ventilation with multiple, bilateral perfusion defects*
- This pattern is characteristic of **pulmonary embolism**, where blood clots obstruct pulmonary arteries, leading to areas of the lung being ventilated but not perfused.
- The clinical picture and chest x-ray findings in this patient are not consistent with pulmonary embolism.
*Normal perfusion with decreased ventilation at the right base*
- While a focal ventilation defect could occur, the patient's symptoms and chest x-ray findings (distended pulmonary veins, Kerley B lines, bilateral blunting of costophrenic angles) suggest **generalized rather than localized pulmonary edema**.
- This option describes a unilateral and focal issue, whereas heart failure typically causes bilateral findings.
*Increased apical ventilation with normal perfusion bilaterally*
- This finding is not typical in any common pulmonary pathology. Increased apical ventilation is not a characteristic of pulmonary edema or other V/Q mismatch disorders.
- This scenario does not align with the patient's symptoms or imaging findings.
V/Q scan principles US Medical PG Question 6: During a clinical study examining the diffusion of gas between the alveolar compartment and the pulmonary capillary blood, men between the ages of 20 and 50 years are evaluated while they hold a sitting position. After inhaling a water-soluble gas that rapidly combines with hemoglobin, the concentration of the gas in the participant's exhaled air is measured and the diffusion capacity is calculated. Assuming that the concentration of the inhaled gas remains the same, which of the following is most likely to increase the flow of the gas across the alveolar membrane?
- A. Deep exhalation
- B. Entering a cold chamber
- C. Treadmill exercise (Correct Answer)
- D. Standing straight
- E. Assuming a hunched position
V/Q scan principles Explanation: ***Correct: Treadmill exercise***
- **Treadmill exercise** increases cardiac output and pulmonary blood flow, which in turn recruits and distends more **pulmonary capillaries**. This increases the **surface area** available for gas exchange and reduces the diffusion distance, thereby enhancing the flow of gas across the alveolar membrane.
- Exercise also typically leads to deeper and more frequent breaths, increasing the **ventilation-perfusion matching** and overall efficiency of gas exchange.
- According to Fick's law of diffusion (Vgas = A/T × D × ΔP), increasing the surface area (A) directly increases gas flow.
*Incorrect: Deep exhalation*
- **Deep exhalation** would empty the lungs more completely, potentially leading to alveolar collapse in some regions and thus **decreasing the alveolar surface area** available for gas exchange.
- This would also reduce the **driving pressure** for gas diffusion by lowering the alveolar concentration of the inhaled gas.
*Incorrect: Entering a cold chamber*
- Exposure to a **cold chamber** can cause **bronchoconstriction** in some individuals, particularly those with reactive airways, which would increase airway resistance and potentially reduce alveolar ventilation.
- While metabolic rate may slightly increase in the cold, the primary effect on the lungs is unlikely to promote increased gas diffusion in a healthy individual.
*Incorrect: Standing straight*
- **Standing straight** is a normal physiological posture and does not significantly alter the **pulmonary capillary recruitment** or the alveolar surface area in a way that would dramatically increase gas flow compared to a seated position.
- There might be minor gravitational effects on blood flow distribution, but these are generally less impactful than dynamic changes like exercise.
*Incorrect: Assuming a hunched position*
- **Assuming a hunched position** can restrict chest wall expansion and diaphragm movement, leading to **reduced tidal volume** and overall alveolar ventilation.
- This posture, by reducing lung volumes and potentially compressing the lungs, would likely **decrease the effective surface area** for gas exchange and therefore reduce gas flow.
V/Q scan principles US Medical PG Question 7: A 22-year-old man volunteers for a research study on lung function. He has no history of lung disease or allergies and does not smoke. His pulmonary blood flow is measured in the various labeled segments of the lungs while standing. Then the volunteer, still standing, is given very low continuous positive airway pressure and the blood flow measured again. Which of the following sets of findings are most likely to be present in the second measurements relative to the first?
- A. Increased blood flow in zone 2
- B. Reduced blood flow in zone 3
- C. Reduced blood flow in zone 1
- D. Increased blood flow in zone 3
- E. Increased blood flow in zone 1 (Correct Answer)
V/Q scan principles Explanation: ***Increased blood flow in zone 1***
- In healthy standing subjects, **Zone 1** may not exist or is minimal at the apex where alveolar pressure (PA) can exceed arterial pressure (Pa).
- **Very low CPAP** increases alveolar pressure, but when applied at very low levels, it may **recruit collapsed or under-perfused alveoli** by preventing alveolar collapse and improving the pressure gradient.
- The net effect with **very low CPAP** can paradoxically **improve perfusion** in Zone 1 by optimizing alveolar mechanics and reducing vascular resistance through **alveolar recruitment**, particularly in previously under-ventilated apical regions.
*Increased blood flow in zone 2*
- In Zone 2, arterial pressure exceeds alveolar pressure, which exceeds venous pressure (**Pa > PA > Pv**), creating a waterfall effect.
- While CPAP increases alveolar pressure (PA), this would increase the downstream resistance and typically **reduce** the arterial-alveolar pressure gradient (Pa - PA), decreasing flow rather than increasing it.
*Increased blood flow in zone 3*
- **Zone 3** (lung base) normally has the **highest blood flow** where both arterial and venous pressures exceed alveolar pressure (**Pa > Pv > PA**).
- CPAP increases alveolar pressure (PA), which would compress capillaries and **reduce** the pressure gradient, typically decreasing rather than increasing blood flow in this zone.
*Reduced blood flow in zone 1*
- While increasing alveolar pressure with CPAP might be expected to **reduce** Zone 1 perfusion by compressing capillaries, **very low levels of CPAP** can have the opposite effect through **alveolar recruitment** and optimization of lung mechanics.
- The question specifies **very low** CPAP, which is the key—this level improves alveolar patency without significantly compressing capillaries.
*Reduced blood flow in zone 3*
- Zone 3 typically has the highest blood flow due to favorable pressure gradients from gravity.
- CPAP increases PA, which could compress capillaries and reduce the (Pa - PA) gradient, but the **very low level** specified means this effect is minimal and Zone 3 generally maintains adequate perfusion.
V/Q scan principles US Medical PG Question 8: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
V/Q scan principles Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
V/Q scan principles US Medical PG Question 9: A 68-year-old man comes to the emergency room with difficulty in breathing. He was diagnosed with severe obstructive lung disease a few years back. He uses his medication but often has to come to the emergency room for intravenous therapy to help him breathe. He was a smoker for 40 years smoking two packs of cigarettes every day. Which of the following best represents the expected changes in his ventilation, perfusion and V/Q ratio?
- A. Normal ventilation, low or nonexistent perfusion and infinite V/Q ratio
- B. Medium ventilation and perfusion, V/Q that equals 0.8
- C. Higher ventilation and perfusion with lower V/Q ratio
- D. Low ventilation, normal perfusion and low V/Q ratio (Correct Answer)
- E. Lower ventilation and perfusion, but higher V/Q ratio
V/Q scan principles Explanation: ***Low ventilation, normal perfusion and low V/Q ratio***
- In severe **obstructive lung disease** (like COPD), there is airflow limitation, leading to areas of **hypoventilation** in the lungs.
- While ventilation is compromised, blood flow (perfusion) to these areas can remain relatively normal, resulting in a **decreased V/Q ratio**.
*Normal ventilation, low or nonexistent perfusion and infinite V/Q ratio*
- This scenario describes a lung unit with **dead space ventilation**, where there is ventilation but no blood flow (e.g., in a pulmonary embolism).
- The patient's history of **obstructive lung disease** primarily indicates impaired airflow, not a lack of perfusion.
*Medium ventilation and perfusion, V/Q that equals 0.8*
- A **V/Q ratio of 0.8** represents the **ideal normal** ventilation-perfusion matching in a healthy lung.
- The patient has severe obstructive lung disease, which by definition means there is significant mismatch, not normal physiology.
*Higher ventilation and perfusion with lower V/Q ratio*
- While hyperventilation can occur in attempts to compensate, the primary issue in obstructive disease is **impaired ventilation**, not increased ventilation, leading to decreased gas exchange.
- A lower V/Q ratio is expected, but it is driven by **low ventilation**, not higher ventilation and perfusion.
*Lower ventilation and perfusion, but higher V/Q ratio*
- Although both ventilation and perfusion can be affected in severe disease, a **higher V/Q ratio** typically implies areas of increased dead space (more ventilation than perfusion).
- In obstructive disease, the predominant problem is **impaired air entry**, leading to underventilated units with relatively preserved perfusion, thus a **low V/Q ratio**.
V/Q scan principles US Medical PG Question 10: A 2-year-old boy is brought to the physician because of coughing and difficulty breathing that started shortly after his mother found him in the living room playing with his older brother's toys. He appears anxious. Respirations are 33/min and pulse oximetry on room air shows an oxygen saturation of 88%. Physical examination shows nasal flaring and intercostal retractions. Auscultation of the lungs shows a high-pitched inspiratory wheeze and absent breath sounds on the right side. There is no improvement in his oxygen saturation after applying a non-rebreather mask with 100% FiO2. Which of the following terms best describes the most likely underlying mechanism of the right lung's impaired ventilation?
- A. Alveolar hyperventilation
- B. Alveolar dead space
- C. Diffusion limitation
- D. Alveolar hypoventilation (Correct Answer)
- E. Right-to-left shunt
V/Q scan principles Explanation: ***Alveolar hypoventilation***
- The clinical presentation strongly suggests **foreign body aspiration** causing complete obstruction of the right main bronchus, leading to **alveolar hypoventilation** of the entire right lung.
- **Alveolar hypoventilation** means reduced or absent air movement into the alveoli. In this case, the mechanical obstruction prevents ventilation (V/Q = 0), while perfusion continues normally, creating severe V/Q mismatch.
- The **hypoxemia unresponsive to 100% FiO2** occurs because blood perfusing the unventilated right lung remains deoxygenated (shunt-like physiology), but the underlying mechanism is **ventilation failure** (hypoventilation), not an anatomical shunt.
- **Absent breath sounds** on the right confirm no air entry to that lung, which is the definition of regional hypoventilation.
*Right-to-left shunt*
- A **true anatomical right-to-left shunt** refers to blood bypassing the lungs entirely through intracardiac defects (VSD, ASD, PDA with Eisenmenger syndrome) or intrapulmonary arteriovenous malformations.
- While the obstructed lung creates **shunt-like physiology** (blood passes unventilated alveoli), the mechanism is **hypoventilation due to airway obstruction**, not an anatomical shunt.
- The distinction is important: shunt describes the physiological effect (V/Q = 0), but hypoventilation describes the mechanism (airway obstruction preventing ventilation).
*Alveolar hyperventilation*
- This refers to **increased alveolar ventilation** beyond metabolic needs, leading to increased CO2 elimination and respiratory alkalosis.
- The patient shows tachypnea (33/min), which represents compensatory effort, but the right lung has **decreased ventilation** (hypoventilation), not hyperventilation.
*Alveolar dead space*
- **Alveolar dead space** occurs when alveoli are **ventilated but not perfused** (V/Q approaching infinity), as seen in pulmonary embolism.
- This scenario shows the opposite: the right lung is **perfused but not ventilated** due to airway obstruction.
*Diffusion limitation*
- **Diffusion limitation** occurs when gas exchange across the alveolar-capillary membrane is impaired (pulmonary fibrosis, interstitial lung disease).
- This patient has **mechanical obstruction preventing air from reaching the alveoli**, not a problem with diffusion across intact membranes.
- Diffusion limitation typically responds partially to supplemental oxygen, unlike complete obstruction.
More V/Q scan principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.