V/Q mismatch in COPD US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for V/Q mismatch in COPD. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
V/Q mismatch in COPD US Medical PG Question 1: A 48-year-old man comes to the physician because of a 3-month history of worsening shortness of breath and cough productive of frothy, whitish sputum. One year ago, he had a similar episode lasting 6 months. He has smoked a pack of cigarettes daily for 25 years. Physical examination shows bluish discoloration of the tongue and lips. Scattered expiratory wheezing and rhonchi are heard throughout both lung fields. Further evaluation of this patient is most likely to show which of the following findings?
- A. Increased FEV1/FVC ratio
- B. Increased diffusing capacity for carbon monoxide
- C. Increased pulmonary capillary wedge pressure
- D. Increased serum hematocrit (Correct Answer)
- E. Normal FEV1
V/Q mismatch in COPD Explanation: ***Increased serum hematocrit***
- This patient presents with symptoms highly suggestive of **chronic bronchitis**, a form of COPD, characterized by a **chronic productive cough** and **hypoxemia**.
- **Chronic hypoxemia** stimulates the kidneys to release **erythropoietin**, leading to secondary **polycythemia** (increased red blood cell mass) and thus an **increased hematocrit** to improve oxygen-carrying capacity.
*Increased FEV1/FVC ratio*
- This patient's symptoms (shortness of breath, productive cough, wheezing, smoking history) are classic for **chronic obstructive pulmonary disease (COPD)**, which is an **obstructive lung disease**.
- Obstructive lung diseases are characterized by **decreased FEV1/FVC ratio** due to airflow limitation, not an increased ratio.
*Increased diffusing capacity for carbon monoxide*
- In COPD, particularly chronic bronchitis and emphysema, the **diffusing capacity for carbon monoxide (DLCO)** is typically **decreased** due to destruction of alveolar-capillary membranes (emphysema) and ventilation-perfusion mismatch (chronic bronchitis).
- An increased DLCO is more commonly seen in conditions like **pulmonary hemorrhage** or **asthma**.
*Increased pulmonary capillary wedge pressure*
- **Increased pulmonary capillary wedge pressure (PCWP)** is characteristic of **left-sided heart failure**, indicating elevated left atrial and pulmonary venous pressures.
- While patients with severe COPD can develop **pulmonary hypertension** and eventually **right-sided heart failure (cor pulmonale)**, the primary pathology described here points to lung disease, not left ventricular dysfunction.
*Normal FEV1*
- In COPD, there is **airflow obstruction** that manifests as a **reduced forced expiratory volume in 1 second (FEV1)**.
- A normal FEV1 would be inconsistent with the clinical presentation of significant, worsening shortness of breath and airflow limitation.
V/Q mismatch in COPD US Medical PG Question 2: A 65-year-old woman presents to her physician with chronic breathlessness. Her condition has been progressively worsening over the last 20 years despite treatment with inhaled salbutamol, inhaled corticosteroids, and multiple courses of antibiotics. She has a 30-pack-year smoking history but quit 20 years ago. Her pulse is 104/min and respirations are 28/min. Physical examination shows generalized wasting. Chest auscultation reveals expiratory wheezes bilaterally and distant heart sounds. Pulmonary function testing shows a non-reversible obstructive pattern. Her carbon monoxide diffusion capacity of the lungs (DLCO) is markedly reduced. Which of the following explains the underlying mechanism of her condition?
- A. Decreased partial pressure of alveolar oxygen
- B. Contraction of pulmonary smooth muscles
- C. Inflammation of the pulmonary bronchi
- D. Diminished surface area for gas exchange (Correct Answer)
- E. Accumulation of fluid in the alveolar space
V/Q mismatch in COPD Explanation: ***Diminished surface area for gas exchange***
- The patient's history of **30-pack-year smoking** and **non-reversible obstructive pattern** with **markedly reduced DLCO** strongly indicates **emphysema**, a form of COPD.
- **Emphysema** is characterized by the destruction of alveolar walls, leading to enlarged air spaces and a significant **reduction in the surface area available for gas exchange.**
*Decreased partial pressure of alveolar oxygen*
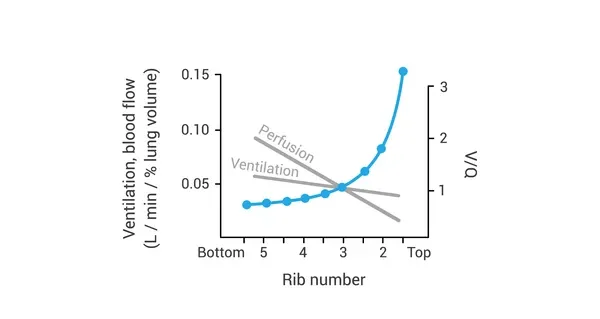
- While a **decreased partial pressure of alveolar oxygen (PAO2)** can occur in severe lung disease due to **ventilation-perfusion mismatch** and hypoventilation, it is not the primary *underlying mechanism* of destruction seen in this patient's presentation.
- The reduced DLCO points directly to an issue with **gas transfer capacity**, which is mainly driven by surface area and membrane thickness, not solely PAO2.
*Contraction of pulmonary smooth muscles*
- **Bronchoconstriction**, or the contraction of pulmonary smooth muscles, is a hallmark of **asthma** and can contribute to the obstructive component in COPD.
- However, the patient's condition is described as **non-reversible** despite bronchodilator treatment, and the severe reduction in **DLCO** suggests a more structural issue than just smooth muscle contraction.
*Inflammation of the pulmonary bronchi*
- **Inflammation of the pulmonary bronchi** is characteristic of **chronic bronchitis**, another component of COPD, which contributes to airway obstruction and mucus production.
- While present, the **markedly reduced DLCO** points more strongly to the **alveolar destruction** of emphysema rather than predominantly bronchial inflammation.
*Accumulation of fluid in the alveolar space*
- **Accumulation of fluid in the alveolar space** occurs in conditions like **pulmonary edema** or **acute respiratory distress syndrome (ARDS)**.
- This would typically present with crackles on auscultation and acute respiratory distress, rather than the chronic, progressive course and wheezing described, and would likely cause a different pattern of DLCO reduction.
V/Q mismatch in COPD US Medical PG Question 3: A 22-year-old man volunteers for a research study on lung function. He has no history of lung disease or allergies and does not smoke. His pulmonary blood flow is measured in the various labeled segments of the lungs while standing. Then the volunteer, still standing, is given very low continuous positive airway pressure and the blood flow measured again. Which of the following sets of findings are most likely to be present in the second measurements relative to the first?
- A. Increased blood flow in zone 2
- B. Reduced blood flow in zone 3
- C. Reduced blood flow in zone 1
- D. Increased blood flow in zone 3
- E. Increased blood flow in zone 1 (Correct Answer)
V/Q mismatch in COPD Explanation: ***Increased blood flow in zone 1***
- In healthy standing subjects, **Zone 1** may not exist or is minimal at the apex where alveolar pressure (PA) can exceed arterial pressure (Pa).
- **Very low CPAP** increases alveolar pressure, but when applied at very low levels, it may **recruit collapsed or under-perfused alveoli** by preventing alveolar collapse and improving the pressure gradient.
- The net effect with **very low CPAP** can paradoxically **improve perfusion** in Zone 1 by optimizing alveolar mechanics and reducing vascular resistance through **alveolar recruitment**, particularly in previously under-ventilated apical regions.
*Increased blood flow in zone 2*
- In Zone 2, arterial pressure exceeds alveolar pressure, which exceeds venous pressure (**Pa > PA > Pv**), creating a waterfall effect.
- While CPAP increases alveolar pressure (PA), this would increase the downstream resistance and typically **reduce** the arterial-alveolar pressure gradient (Pa - PA), decreasing flow rather than increasing it.
*Increased blood flow in zone 3*
- **Zone 3** (lung base) normally has the **highest blood flow** where both arterial and venous pressures exceed alveolar pressure (**Pa > Pv > PA**).
- CPAP increases alveolar pressure (PA), which would compress capillaries and **reduce** the pressure gradient, typically decreasing rather than increasing blood flow in this zone.
*Reduced blood flow in zone 1*
- While increasing alveolar pressure with CPAP might be expected to **reduce** Zone 1 perfusion by compressing capillaries, **very low levels of CPAP** can have the opposite effect through **alveolar recruitment** and optimization of lung mechanics.
- The question specifies **very low** CPAP, which is the key—this level improves alveolar patency without significantly compressing capillaries.
*Reduced blood flow in zone 3*
- Zone 3 typically has the highest blood flow due to favorable pressure gradients from gravity.
- CPAP increases PA, which could compress capillaries and reduce the (Pa - PA) gradient, but the **very low level** specified means this effect is minimal and Zone 3 generally maintains adequate perfusion.
V/Q mismatch in COPD US Medical PG Question 4: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
V/Q mismatch in COPD Explanation: ***Pulmonary embolism***
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
V/Q mismatch in COPD US Medical PG Question 5: A 72-year-old obese man presents as a new patient to his primary care physician because he has been feeling tired and short of breath after recently moving to Denver. He is a former 50 pack-year smoker and has previously had deep venous thrombosis. Furthermore, he previously had a lobe of the lung removed due to lung cancer. Finally, he has a family history of a progressive restrictive lung disease. Laboratory values are obtained as follows:
Oxygen tension in inspired air = 130 mmHg
Alveolar carbon dioxide tension = 48 mmHg
Arterial oxygen tension = 58 mmHg
Respiratory exchange ratio = 0.80
Respiratory rate = 20/min
Tidal volume = 500 mL
Which of the following mechanisms is consistent with these values?
- A. Shunt physiology
- B. High altitude
- C. V/Q mismatch
- D. Pulmonary fibrosis
- E. Hypoventilation (Correct Answer)
V/Q mismatch in COPD Explanation: ***Hypoventilation***
- The arterial oxygen tension (PaO2) of 58 mmHg is consistent with hypoxemia, and the alveolar carbon dioxide tension (PACO2) of 48 mmHg (normal 35-45 mmHg) indicates **hypercapnia**, a hallmark of hypoventilation.
- The **alveolar-arterial (A-a) gradient** can be calculated using the alveolar gas equation: PAO2 = PiO2 - PACO2/R. Here, PAO2 = 130 mmHg - 48 mmHg/0.8 = 130 - 60 = 70 mmHg. The A-a gradient is PAO2 - PaO2 = 70 - 58 = 12 mmHg, which is within the normal range (5-15 mmHg), indicating that the hypoxemia is primarily due to **decreased alveolar ventilation**.
*Shunt physiology*
- A shunt would cause a significant reduction in PaO2 and a **widened A-a gradient** (typically >15 mmHg) due to deoxygenated blood bypassing ventilated areas.
- While shunts do not typically cause hypercapnia unless very severe, the normal A-a gradient here rules out a significant shunt as the primary mechanism for hypoxemia.
*High altitude*
- Moving to a high altitude (like Denver) causes a decrease in **inspired oxygen tension (PiO2)**, leading to hypoxemia.
- However, the provided inspired oxygen tension (130 mmHg) is above what would be expected for significant high-altitude hypoxemia at sea level equivalent, and the hypoxemia here is associated with hypercapnia, which is not a direct result of high altitude itself.
*V/Q mismatch*
- A V/Q mismatch leads to hypoxemia and a **widened A-a gradient**, as some areas of the lung are either underventilated or underperfused.
- While it can cause hypoxemia, a V/Q mismatch is typically associated with **normal or low PaCO2** due to compensatory hyperventilation, not hypercapnia, and the A-a gradient would be elevated.
*Pulmonary fibrosis*
- Pulmonary fibrosis is a restrictive lung disease that leads to impaired gas exchange, causing hypoxemia primarily due to **V/Q mismatch** and **diffusion limitation**.
- This would result in a **widened A-a gradient** and often a **low PaCO2** due to compensatory hyperventilation, rather than the elevated PaCO2 observed in this patient.
V/Q mismatch in COPD US Medical PG Question 6: A 55-year-old man with a 60 pack-year smoking history is referred by his primary care physician for a pulmonary function test (PFT). A previously obtained chest x-ray is shown below. Which of the following will most likely appear in his PFT report?
- A. Residual volume increased, total lung capacity decreased
- B. Residual volume normal, total lung capacity decreased
- C. Residual volume normal, total lung capacity normal
- D. Residual volume decreased, total lung capacity increased
- E. Residual volume increased, total lung capacity increased (Correct Answer)
V/Q mismatch in COPD Explanation: ***Residual volume increased, total lung capacity increased***
- The chest X-ray shows **hyperinflation** and a **flattened diaphragm**, which are classic signs of **emphysema**, a type of COPD.
- In emphysema, destruction of alveolar walls leads to air trapping, resulting in an **increased residual volume** and **total lung capacity**.
*Residual volume increased, total lung capacity decreased*
- An increased residual volume suggests **air trapping**, typical of obstructive lung diseases like emphysema.
- However, a **decreased total lung capacity** is characteristic of restrictive lung diseases, which would contradict the clinical and radiological findings for emphysema.
*Residual volume normal, total lung capacity decreased*
- A **normal residual volume** indicates no significant air trapping, which is inconsistent with emphysema.
- A **decreased total lung capacity** is seen in restrictive lung diseases, not obstructive diseases like emphysema.
*Residual volume normal, total lung capacity normal*
- **Normal lung volumes** would indicate healthy lung function, which is not expected in a patient with a heavy smoking history and radiological evidence of emphysema.
- The patient's 60 pack-year smoking history strongly points towards significant lung pathology.
*Residual volume decreased, total lung capacity increased*
- A **decreased residual volume** would suggest improved exhalation and less air trapping, which is contrary to the pathophysiology of emphysema.
- While total lung capacity can be increased in emphysema, the decrease in residual volume makes this option incorrect.
V/Q mismatch in COPD US Medical PG Question 7: Two days after undergoing left hemicolectomy for a colonic mass, a 62-year-old man develops shortness of breath. His temperature is 38.1°C (100.6°F), pulse is 80/min, respirations are 22/min, and blood pressure is 120/78 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 88%. Cardiopulmonary examination shows decreased breath sounds and decreased fremitus at both lung bases. Arterial blood gas analysis on room air shows:
pH 7.35
PaO2 70 mm Hg
PCO2 40 mm Hg
An x-ray of the chest shows a collapse of the bases of both lungs. Which of the following is the most likely underlying mechanism of this patient's hypoxemia?
- A. Increased anatomic dead space
- B. Decreased hemoglobin oxygen-binding capacity
- C. Decreased chest wall compliance
- D. Increased tidal volume
- E. Decreased ratio of ventilated alveoli (Correct Answer)
V/Q mismatch in COPD Explanation: ***Decreased ratio of ventilated alveoli***
- The patient's presentation with **shortness of breath**, **decreased breath sounds and fremitus at both lung bases**, and **collapsed lung bases on chest x-ray** points to **atelectasis**.
- **Atelectasis** is a common cause of hypoxemia post-surgery. It occurs when alveoli collapse, leading to areas of the lung that are perfused but not ventilated, resulting in a **ventilation-perfusion (V/Q) mismatch** with a decreased ratio of ventilated alveoli.
*Increased anatomic dead space*
- **Anatomic dead space** refers to the conducting airways where gas exchange does not occur. This value is relatively constant and would not increase significantly to cause such profound hypoxemia in this context.
- Conditions like chronic obstructive pulmonary disease (COPD) can increase dead space, but the patient's acute postoperative presentation and chest X-ray findings do not support this as the primary cause.
*Decreased hemoglobin oxygen-binding capacity*
- This would involve issues like **carbon monoxide poisoning** or specific hemoglobinopathies, which are not indicated by the clinical picture or ABG results (normal pH, PaO2 70 mmHg, PCO2 40 mmHg).
- The PaO2 and SaO2 values indicate a problem with oxygen uptake, not oxygen transport by hemoglobin once bound.
*Decreased chest wall compliance*
- While surgery can cause **pain leading to splinting** and reduced chest wall expansion, which impacts compliance, the primary mechanism of hypoxemia in atelectasis is the **collapse of alveoli**, not solely reduced chest wall movement.
- The **collapsed lung bases** on X-ray directly point to alveolar collapse rather than a general decrease in chest wall compliance as the primary problem.
*Increased tidal volume*
- **Increased tidal volume** would typically improve ventilation and oxygenation, not lead to hypoxemia.
- The patient's **hypoxemia (SaO2 88%, PaO2 70 mmHg)** clearly indicates a problem with oxygen uptake, not an enhancement of respiratory function.
V/Q mismatch in COPD US Medical PG Question 8: A 64-year-old man presents to his primary care physician for follow-up of a severe, unrelenting, productive cough of 2 years duration. The medical history includes type 2 diabetes mellitus, which is well-controlled with insulin. He has a 25-pack-year smoking history and is an active smoker. The blood pressure is 135/88 mm Hg, the pulse is 94/min, the temperature is 36.9°C (98.5°F), and the respiratory rate is 18/min. Bilateral wheezes and crackles are heard on auscultation. A chest X-ray reveals cardiomegaly, increased lung markings, and a flattened diaphragm. Which of the following is most likely in this patient?
- A. Increased pH of the arterial blood
- B. Increased cerebral vascular resistance
- C. Increased pulmonary arterial resistance (Correct Answer)
- D. Decreased carbon dioxide content of the arterial blood
- E. Increased right ventricle compliance
V/Q mismatch in COPD Explanation: ***Increased pulmonary arterial resistance***
- This patient's long-standing **smoking history**, chronic productive cough, **wheezes**, and **crackles** suggest **Chronic Obstructive Pulmonary Disease (COPD)**, likely including chronic bronchitis and emphysema.
- **COPD** often leads to **hypoxia**, causing **pulmonary vasoconstriction** and subsequent increase in **pulmonary arterial resistance**, eventually leading to **pulmonary hypertension** and **cor pulmonale** (right-sided heart failure).
*Increased pH of the arterial blood*
- Patients with severe COPD and chronic respiratory insufficiency often develop **chronic hypercapnia** (increased **PaCO2**), leading to **respiratory acidosis** and a tendency towards a **decreased pH** or a normal pH with compensation.
- An **increased pH** (alkalosis) would be less likely in the context of chronic ventilatory compromise.
*Increased cerebral vascular resistance*
- In chronic hypercapnia and hypoxia, **cerebral blood vessels** typically **dilate** to maintain cerebral perfusion, leading to **decreased cerebral vascular resistance**, not increased.
- This vasodilation can contribute to symptoms like headaches and altered mental status in severe cases.
*Decreased carbon dioxide content of the arterial blood*
- Patients with chronic obstructive lung disease often have impaired gas exchange, leading to **CO2 retention** (**hypercapnia**).
- Therefore, the **arterial carbon dioxide content** would typically be **increased**, not decreased.
*Increased right ventricle compliance*
- In the setting of chronic **pulmonary hypertension**, the right ventricle is subjected to increased pressure overload, leading to **ventricular hypertrophy** and eventually **decreased compliance** and **ventricular dysfunction**.
- **Increased compliance** (meaning the ventricle stretches more easily) is contrary to the expected response in chronic pressure overload.
V/Q mismatch in COPD US Medical PG Question 9: A 68-year-old man comes to the emergency room with difficulty in breathing. He was diagnosed with severe obstructive lung disease a few years back. He uses his medication but often has to come to the emergency room for intravenous therapy to help him breathe. He was a smoker for 40 years smoking two packs of cigarettes every day. Which of the following best represents the expected changes in his ventilation, perfusion and V/Q ratio?
- A. Normal ventilation, low or nonexistent perfusion and infinite V/Q ratio
- B. Medium ventilation and perfusion, V/Q that equals 0.8
- C. Higher ventilation and perfusion with lower V/Q ratio
- D. Low ventilation, normal perfusion and low V/Q ratio (Correct Answer)
- E. Lower ventilation and perfusion, but higher V/Q ratio
V/Q mismatch in COPD Explanation: ***Low ventilation, normal perfusion and low V/Q ratio***
- In severe **obstructive lung disease** (like COPD), there is airflow limitation, leading to areas of **hypoventilation** in the lungs.
- While ventilation is compromised, blood flow (perfusion) to these areas can remain relatively normal, resulting in a **decreased V/Q ratio**.
*Normal ventilation, low or nonexistent perfusion and infinite V/Q ratio*
- This scenario describes a lung unit with **dead space ventilation**, where there is ventilation but no blood flow (e.g., in a pulmonary embolism).
- The patient's history of **obstructive lung disease** primarily indicates impaired airflow, not a lack of perfusion.
*Medium ventilation and perfusion, V/Q that equals 0.8*
- A **V/Q ratio of 0.8** represents the **ideal normal** ventilation-perfusion matching in a healthy lung.
- The patient has severe obstructive lung disease, which by definition means there is significant mismatch, not normal physiology.
*Higher ventilation and perfusion with lower V/Q ratio*
- While hyperventilation can occur in attempts to compensate, the primary issue in obstructive disease is **impaired ventilation**, not increased ventilation, leading to decreased gas exchange.
- A lower V/Q ratio is expected, but it is driven by **low ventilation**, not higher ventilation and perfusion.
*Lower ventilation and perfusion, but higher V/Q ratio*
- Although both ventilation and perfusion can be affected in severe disease, a **higher V/Q ratio** typically implies areas of increased dead space (more ventilation than perfusion).
- In obstructive disease, the predominant problem is **impaired air entry**, leading to underventilated units with relatively preserved perfusion, thus a **low V/Q ratio**.
V/Q mismatch in COPD US Medical PG Question 10: A 62-year-old man is brought to the emergency department with a 2-day history of cough productive of yellowish sputum. He has had fever, chills, and worsening shortness of breath over this time. He has a 10-year history of hypertension and hyperlipidemia. He does not drink alcohol or smoke cigarettes. His current medications include atorvastatin, amlodipine, and metoprolol. His temperature is 38.9°C (102.0°F), pulse is 105/min, respirations are 27/min, and blood pressure is 110/70 mm Hg. He appears in mild distress. He has rales over the left lower lung field. The remainder of the examination shows no abnormalities. Leukocyte count is 15,000/mm3 (87% segmented neutrophils). Arterial blood gas analysis on room air shows:
pH 7.44
pO2 68 mm Hg
pCO2 28 mm Hg
HCO3- 24 mEq/L
O2 saturation 91%
An x-ray of the chest shows a consolidation in the left lower lobe. Asking the patient to lie down in the left lateral decubitus position would most likely result in which of the following?
- A. Decreased ventilation of the left lung
- B. Worsen the hypocapnia
- C. Increase in A-a gradient (Correct Answer)
- D. Increased perfusion of right lung
- E. Improve the hypoxemia
V/Q mismatch in COPD Explanation: ***Increase in A-a gradient***
- Placing the patient in the **left lateral decubitus position** would worsen V/Q mismatch because the **diseased left lung** (with consolidation) would receive increased perfusion due to gravity.
- This increased perfusion to a poorly ventilated area would further impair gas exchange, leading to a larger **alveolar-arterial (A-a) gradient**.
*Decreased ventilation of the left lung*
- While lying on the left side might slightly restrict the expansion of the left lung, the primary issue is the **consolidation** itself, which already severely impairs ventilation.
- The main problem with positioning is not a further decrease in ventilation but rather the **redistribution of blood flow** to an already compromised lung.
*Worsen the hypocapnia*
- The patient has **hypocapnia (pCO2 28 mm Hg)** due to tachypnea as compensation for hypoxemia, indicating increased minute ventilation.
- While worsening the V/Q mismatch will worsen hypoxemia, it's unlikely to directly worsen hypocapnia further; the body would still try to compensate through increased respiratory drive unless the respiratory muscles become fatigued.
*Increased perfusion of right lung*
- In the left lateral decubitus position, **perfusion due to gravity** would increase in the dependent (left) lung, not the non-dependent (right) lung.
- The right lung would experience relatively decreased perfusion compared to the left lung in this position.
*Improve the hypoxemia*
- Lying on the side of the **diseased lung** (left) typically **worsens hypoxemia** because gravity directs more blood flow to the poorly ventilated, consolidated lung.
- To improve hypoxemia, the patient should be positioned with the **healthy lung dependent** (e.g., right lateral decubitus or semi-Fowler's with the right lung lower) to optimize V/Q matching.
More V/Q mismatch in COPD US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.