Normal V/Q distribution US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Normal V/Q distribution. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Normal V/Q distribution US Medical PG Question 1: A 71-year-old man is admitted to the ICU with a history of severe pancreatitis and new onset difficulty breathing. His vital signs are a blood pressure of 100/60 mm Hg, heart rate of 100/min, respirations of 27/min, temperature of 36.7°C (98.1°F), and oxygen saturation of 85% on room air. Physical examination shows a cachectic male in severe respiratory distress. Rales are heard at the base of each lung. The patient is intubated and a Swan-Ganz catheter is inserted. Pulmonary capillary wedge pressure is 8 mm Hg. An arterial blood gas study reveals a PaO2: FiO2 ratio of 180. The patient is diagnosed with acute respiratory distress syndrome. In which of the following segments of the respiratory tract are the cells responsible for the symptoms observed in this patient found?
- A. Alveolar sacs (Correct Answer)
- B. Terminal bronchioles
- C. Bronchi
- D. Respiratory bronchioles
- E. Bronchioles
Normal V/Q distribution Explanation: ***Alveolar sacs***
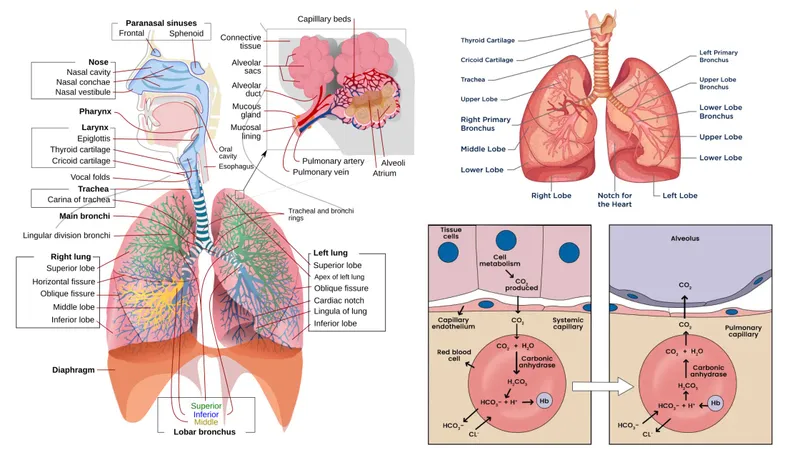
- **Acute respiratory distress syndrome (ARDS)** is characterized by widespread inflammatory injury to the **alveolar-capillary membrane**, leading to increased permeability and fluid accumulation in the alveolar sacs.
- The symptoms, including **severe hypoxemia** (PaO2:FiO2 ratio < 300), **non-cardiogenic pulmonary edema** (PCWP ≤ 18 mmHg), and **bilateral lung infiltrates**, directly result from damage to the **Type I and Type II pneumocytes** and endothelial cells within the alveolar units.
*Terminal bronchioles*
- These are the last airways that **do not contain alveoli**, primarily involved in air conduction rather than gas exchange.
- While inflammation can extend to these structures in severe lung injury, the primary site of impaired gas exchange and fluid accumulation in ARDS occurs distal to them, in the respiratory zone.
*Bronchi*
- The bronchi are primarily involved in **air conduction** and consist of cartilage, smooth muscle, and ciliated epithelium, but they do not participate in gas exchange.
- Injury to the bronchi would manifest as airway obstruction or mucus hypersecretion rather than the diffuse alveolar damage seen in ARDS.
*Respiratory bronchioles*
- These are the first airways that contain a **small number of alveoli** and participate in gas exchange, but their primary role is still more conductive than the alveolar sacs.
- Although they can be affected in ARDS, the most critical damage and symptoms arise from the more extensive gas exchange surface of the alveolar sacs.
*Bronchioles*
- Bronchioles are small airways lacking cartilage, primarily responsible for **airflow regulation** and conduction.
- While they can be affected by inflammation, the extensive impairment of gas exchange and the characteristic pathology of ARDS specifically involves the **alveolar units**, not primarily the bronchioles.
Normal V/Q distribution US Medical PG Question 2: A 71-year-old man is admitted to the hospital one hour after he was found unconscious. His pulse is 80/min and systolic blood pressure is 98 mm Hg; diastolic blood pressure cannot be measured. He is intubated and mechanically ventilated with supplemental oxygen at a tidal volume of 450 mL and a respiratory rate of 10/min. Arterial blood gas analysis shows:
PCO2 43 mm Hg
O2 saturation 94%
O2 content 169 mL/L
Pulmonary artery catheterization shows a pulmonary artery pressure of 15 mm Hg and a pulmonary capillary wedge pressure of 7 mm Hg. Bedside indirect calorimetry shows a rate of O2 tissue consumption of 325 mL/min. Given this information, which of the following additional values is sufficient to calculate the cardiac output in this patient?
- A. Left ventricular end-diastolic volume
- B. Partial pressure of inspired oxygen
- C. End-tidal carbon dioxide pressure
- D. Pulmonary artery oxygen content (Correct Answer)
- E. Total peripheral resistance
Normal V/Q distribution Explanation: ***Pulmonary artery oxygen content***
- Cardiac output can be calculated using the **Fick principle**, which states that **Cardiac Output = (Oxygen Consumption) / (Arteriovenous Oxygen Difference)**.
- We are provided with **O2 tissue consumption (325 mL/min)** and **arterial O2 content (169 mL/L)**. To complete the Fick equation, we need the **mixed venous oxygen content**, which is represented by the **pulmonary artery oxygen content**.
*Left ventricular end-diastolic volume*
- While **left ventricular end-diastolic volume** is a determinant of stroke volume (and thus cardiac output), it alone is not sufficient to calculate cardiac output without knowing heart rate and ejection fraction.
- This value is more relevant for assessing **preload** and ventricular function.
*Partial pressure of inspired oxygen*
- The **partial pressure of inspired oxygen** is used to calculate the **alveolar oxygen partial pressure** and is important for assessing oxygenation and respiratory function.
- It is not directly used in the Fick principle for calculating cardiac output.
*End-tidal carbon dioxide pressure*
- **End-tidal carbon dioxide (ETCO2)** is a measure of the partial pressure of CO2 at the end of exhalation and reflects ventilation and pulmonary perfusion.
- While it can be correlated with cardiac output in certain clinical contexts, it is not a direct input for the **Fick principle** calculation of cardiac output.
*Total peripheral resistance*
- **Total peripheral resistance (TPR)** can be calculated from cardiac output and mean arterial pressure using the formula: **(MAP - CVP) / CO**, but it cannot be used to calculate cardiac output directly without knowing the other variables.
- TPR is a measure of the **resistance to blood flow** in the systemic circulation.
Normal V/Q distribution US Medical PG Question 3: A 35-year-old man presents to pulmonary function clinic for preoperative evaluation for a right pneumonectomy. His arterial blood gas at room air is as follows:
pH: 7.34
PaCO2: 68 mmHg
PaO2: 56 mmHg
Base excess: +1
O2 saturation: 89%
What underlying condition most likely explains these findings?
- A. Cystic fibrosis
- B. Bronchiectasis
- C. Chronic obstructive pulmonary disease (Correct Answer)
- D. Obesity
- E. Acute respiratory distress syndrome
Normal V/Q distribution Explanation: ***Chronic obstructive pulmonary disease***
- This patient exhibits **compensated respiratory acidosis** (low pH, high PaCO2, slightly elevated base excess) and **hypoxemia** (low PaO2), which are characteristic findings in chronic obstructive pulmonary disease (COPD) with underlying respiratory failure.
- The history of a planned **pneumonectomy** also suggests a significant pre-existing lung pathology often seen in patients with severe COPD.
*Cystic fibrosis*
- While cystic fibrosis can lead to chronic lung disease, it typically presents at a younger age and is associated with a history of recurrent infections and exocrine gland dysfunction.
- While it can manifest similarly in ABG, the age and the planned pneumonectomy make COPD a more likely primary cause in this context.
*Bronchiectasis*
- Bronchiectasis involves permanent dilation of the bronchi, often leading to chronic cough, sputum production, and recurrent infections.
- While it can cause respiratory compromise, the ABG findings are more classically associated with the widespread air trapping and V/Q mismatch seen in COPD.
*Obesity*
- Severe obesity can lead to **obesity hypoventilation syndrome**, presenting with hypercapnia and hypoxemia.
- However, the patient's age and the context of a planned pneumonectomy make an underlying primary lung disease like COPD a more focused explanation for the ABG pattern.
*Acute respiratory distress syndrome*
- Acute respiratory distress syndrome (ARDS) is an **acute** and severe form of respiratory failure characterized by severe hypoxemia and bilateral opacities on chest imaging.
- The ABG findings in ARDS typically show **severe hypoxemia** with **respiratory alkalosis** early on, evolving to acidosis, and it is an acute process, not a chronic pre-existing condition suitable for elective surgery.
Normal V/Q distribution US Medical PG Question 4: A 72-year-old obese man presents as a new patient to his primary care physician because he has been feeling tired and short of breath after recently moving to Denver. He is a former 50 pack-year smoker and has previously had deep venous thrombosis. Furthermore, he previously had a lobe of the lung removed due to lung cancer. Finally, he has a family history of a progressive restrictive lung disease. Laboratory values are obtained as follows:
Oxygen tension in inspired air = 130 mmHg
Alveolar carbon dioxide tension = 48 mmHg
Arterial oxygen tension = 58 mmHg
Respiratory exchange ratio = 0.80
Respiratory rate = 20/min
Tidal volume = 500 mL
Which of the following mechanisms is consistent with these values?
- A. Shunt physiology
- B. High altitude
- C. V/Q mismatch
- D. Pulmonary fibrosis
- E. Hypoventilation (Correct Answer)
Normal V/Q distribution Explanation: ***Hypoventilation***
- The arterial oxygen tension (PaO2) of 58 mmHg is consistent with hypoxemia, and the alveolar carbon dioxide tension (PACO2) of 48 mmHg (normal 35-45 mmHg) indicates **hypercapnia**, a hallmark of hypoventilation.
- The **alveolar-arterial (A-a) gradient** can be calculated using the alveolar gas equation: PAO2 = PiO2 - PACO2/R. Here, PAO2 = 130 mmHg - 48 mmHg/0.8 = 130 - 60 = 70 mmHg. The A-a gradient is PAO2 - PaO2 = 70 - 58 = 12 mmHg, which is within the normal range (5-15 mmHg), indicating that the hypoxemia is primarily due to **decreased alveolar ventilation**.
*Shunt physiology*
- A shunt would cause a significant reduction in PaO2 and a **widened A-a gradient** (typically >15 mmHg) due to deoxygenated blood bypassing ventilated areas.
- While shunts do not typically cause hypercapnia unless very severe, the normal A-a gradient here rules out a significant shunt as the primary mechanism for hypoxemia.
*High altitude*
- Moving to a high altitude (like Denver) causes a decrease in **inspired oxygen tension (PiO2)**, leading to hypoxemia.
- However, the provided inspired oxygen tension (130 mmHg) is above what would be expected for significant high-altitude hypoxemia at sea level equivalent, and the hypoxemia here is associated with hypercapnia, which is not a direct result of high altitude itself.
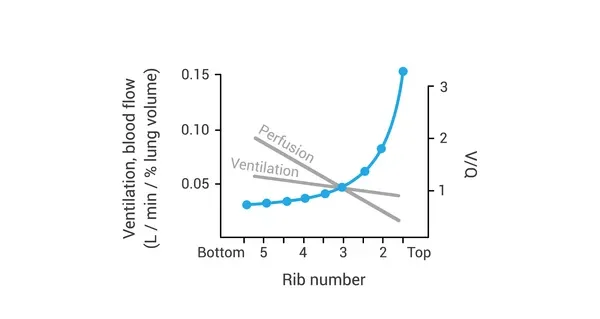
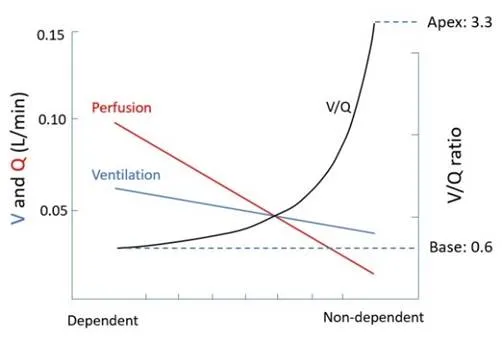
*V/Q mismatch*
- A V/Q mismatch leads to hypoxemia and a **widened A-a gradient**, as some areas of the lung are either underventilated or underperfused.
- While it can cause hypoxemia, a V/Q mismatch is typically associated with **normal or low PaCO2** due to compensatory hyperventilation, not hypercapnia, and the A-a gradient would be elevated.
*Pulmonary fibrosis*
- Pulmonary fibrosis is a restrictive lung disease that leads to impaired gas exchange, causing hypoxemia primarily due to **V/Q mismatch** and **diffusion limitation**.
- This would result in a **widened A-a gradient** and often a **low PaCO2** due to compensatory hyperventilation, rather than the elevated PaCO2 observed in this patient.
Normal V/Q distribution US Medical PG Question 5: A graph shows four different distribution curves labeled A, B, C, and D. Identify the correct sequence of distribution types shown in the graph.
- A. Skewed with outliers, positively skewed, negatively skewed, normal
- B. Normal, positively skewed, negatively skewed, normal with outliers (Correct Answer)
- C. Normal, negatively skewed, positively skewed, skewed with outliers
- D. Normal, negatively skewed, positively skewed, normal with outliers
Normal V/Q distribution Explanation: This question tests the ability to identify different types of **statistical distributions** commonly encountered in biostatistics.
***Correct Answer: Normal, positively skewed, negatively skewed, normal with outliers***
This represents the correct sequence of four fundamental distribution patterns:
**Normal Distribution (A):**
- Symmetrical, bell-shaped curve
- Mean = Median = Mode
- Most data points cluster around the center
- Standard distribution pattern in many biological variables (e.g., height, blood pressure in populations)
**Positively Skewed Distribution (B):**
- Tail extends toward the **right (positive direction)**
- Mean > Median > Mode
- Common in data like: disease incubation periods, hospital length of stay, income distributions
- Clinical example: Most patients recover quickly, but few have prolonged illness
**Negatively Skewed Distribution (C):**
- Tail extends toward the **left (negative direction)**
- Mode > Median > Mean
- Less common in medical data
- Example: Age at death in developed countries (most die at older ages, few die young)
**Normal Distribution with Outliers (D):**
- Generally symmetrical bell shape
- Contains extreme values (outliers) that deviate significantly from the pattern
- Important to identify as outliers can affect statistical analysis
- Clinical example: Most patients respond normally to treatment, but few show extreme responses
---
*Why Other Options Are Incorrect:*
The other options present incorrect sequences of the distribution types. The key is recognizing:
- The direction of skewness (tail direction)
- The difference between basic skewed distributions and those with outliers
- The symmetry of normal distributions
**Clinical Relevance:** Understanding distribution types is essential for:
- Choosing appropriate statistical tests (parametric vs non-parametric)
- Identifying data patterns in epidemiological studies
- Recognizing when data transformation is needed
- Detecting outliers that may represent errors or special cases
Normal V/Q distribution US Medical PG Question 6: During a clinical study examining the diffusion of gas between the alveolar compartment and the pulmonary capillary blood, men between the ages of 20 and 50 years are evaluated while they hold a sitting position. After inhaling a water-soluble gas that rapidly combines with hemoglobin, the concentration of the gas in the participant's exhaled air is measured and the diffusion capacity is calculated. Assuming that the concentration of the inhaled gas remains the same, which of the following is most likely to increase the flow of the gas across the alveolar membrane?
- A. Deep exhalation
- B. Entering a cold chamber
- C. Treadmill exercise (Correct Answer)
- D. Standing straight
- E. Assuming a hunched position
Normal V/Q distribution Explanation: ***Correct: Treadmill exercise***
- **Treadmill exercise** increases cardiac output and pulmonary blood flow, which in turn recruits and distends more **pulmonary capillaries**. This increases the **surface area** available for gas exchange and reduces the diffusion distance, thereby enhancing the flow of gas across the alveolar membrane.
- Exercise also typically leads to deeper and more frequent breaths, increasing the **ventilation-perfusion matching** and overall efficiency of gas exchange.
- According to Fick's law of diffusion (Vgas = A/T × D × ΔP), increasing the surface area (A) directly increases gas flow.
*Incorrect: Deep exhalation*
- **Deep exhalation** would empty the lungs more completely, potentially leading to alveolar collapse in some regions and thus **decreasing the alveolar surface area** available for gas exchange.
- This would also reduce the **driving pressure** for gas diffusion by lowering the alveolar concentration of the inhaled gas.
*Incorrect: Entering a cold chamber*
- Exposure to a **cold chamber** can cause **bronchoconstriction** in some individuals, particularly those with reactive airways, which would increase airway resistance and potentially reduce alveolar ventilation.
- While metabolic rate may slightly increase in the cold, the primary effect on the lungs is unlikely to promote increased gas diffusion in a healthy individual.
*Incorrect: Standing straight*
- **Standing straight** is a normal physiological posture and does not significantly alter the **pulmonary capillary recruitment** or the alveolar surface area in a way that would dramatically increase gas flow compared to a seated position.
- There might be minor gravitational effects on blood flow distribution, but these are generally less impactful than dynamic changes like exercise.
*Incorrect: Assuming a hunched position*
- **Assuming a hunched position** can restrict chest wall expansion and diaphragm movement, leading to **reduced tidal volume** and overall alveolar ventilation.
- This posture, by reducing lung volumes and potentially compressing the lungs, would likely **decrease the effective surface area** for gas exchange and therefore reduce gas flow.
Normal V/Q distribution US Medical PG Question 7: A 22-year-old man volunteers for a research study on lung function. He has no history of lung disease or allergies and does not smoke. His pulmonary blood flow is measured in the various labeled segments of the lungs while standing. Then the volunteer, still standing, is given very low continuous positive airway pressure and the blood flow measured again. Which of the following sets of findings are most likely to be present in the second measurements relative to the first?
- A. Increased blood flow in zone 2
- B. Reduced blood flow in zone 3
- C. Reduced blood flow in zone 1
- D. Increased blood flow in zone 3
- E. Increased blood flow in zone 1 (Correct Answer)
Normal V/Q distribution Explanation: ***Increased blood flow in zone 1***
- In healthy standing subjects, **Zone 1** may not exist or is minimal at the apex where alveolar pressure (PA) can exceed arterial pressure (Pa).
- **Very low CPAP** increases alveolar pressure, but when applied at very low levels, it may **recruit collapsed or under-perfused alveoli** by preventing alveolar collapse and improving the pressure gradient.
- The net effect with **very low CPAP** can paradoxically **improve perfusion** in Zone 1 by optimizing alveolar mechanics and reducing vascular resistance through **alveolar recruitment**, particularly in previously under-ventilated apical regions.
*Increased blood flow in zone 2*
- In Zone 2, arterial pressure exceeds alveolar pressure, which exceeds venous pressure (**Pa > PA > Pv**), creating a waterfall effect.
- While CPAP increases alveolar pressure (PA), this would increase the downstream resistance and typically **reduce** the arterial-alveolar pressure gradient (Pa - PA), decreasing flow rather than increasing it.
*Increased blood flow in zone 3*
- **Zone 3** (lung base) normally has the **highest blood flow** where both arterial and venous pressures exceed alveolar pressure (**Pa > Pv > PA**).
- CPAP increases alveolar pressure (PA), which would compress capillaries and **reduce** the pressure gradient, typically decreasing rather than increasing blood flow in this zone.
*Reduced blood flow in zone 1*
- While increasing alveolar pressure with CPAP might be expected to **reduce** Zone 1 perfusion by compressing capillaries, **very low levels of CPAP** can have the opposite effect through **alveolar recruitment** and optimization of lung mechanics.
- The question specifies **very low** CPAP, which is the key—this level improves alveolar patency without significantly compressing capillaries.
*Reduced blood flow in zone 3*
- Zone 3 typically has the highest blood flow due to favorable pressure gradients from gravity.
- CPAP increases PA, which could compress capillaries and reduce the (Pa - PA) gradient, but the **very low level** specified means this effect is minimal and Zone 3 generally maintains adequate perfusion.
Normal V/Q distribution US Medical PG Question 8: A 21-year-old man is admitted to the intensive care unit for respiratory failure requiring mechanical ventilation. His minute ventilation is calculated to be 7.0 L/min, and his alveolar ventilation is calculated to be 5.1 L/min. Which of the following is most likely to decrease the difference between minute ventilation and alveolar ventilation?
- A. Increasing the partial pressure of inhaled oxygen
- B. Decreasing the affinity of hemoglobin for oxygen
- C. Increasing the respiratory depth
- D. Decreasing the physiologic dead space (Correct Answer)
- E. Increasing the respiratory rate
Normal V/Q distribution Explanation: ***Decreasing the physiologic dead space***
- The difference between **minute ventilation (VE)** and **alveolar ventilation (VA)** is the **dead space ventilation (VD)**, calculated as: VE - VA = VD
- In this case: 7.0 L/min - 5.1 L/min = 1.9 L/min of dead space ventilation
- Decreasing the **physiologic dead space** directly reduces this difference by allowing a greater proportion of each breath to participate in gas exchange
- This is the most direct way to narrow the gap between VE and VA
*Increasing the partial pressure of inhaled oxygen*
- This intervention primarily affects **oxygenation** by increasing the driving pressure for oxygen diffusion into the blood
- It does not directly change the volume of air participating in alveolar ventilation or reduce dead space ventilation
- The distribution of ventilation between alveolar and dead space remains unchanged
*Decreasing the affinity of hemoglobin for oxygen*
- A decrease in hemoglobin affinity for oxygen facilitates **oxygen unloading** to the tissues (rightward shift of the oxygen-hemoglobin dissociation curve)
- This effect is related to **oxygen delivery** and does not alter the proportion of minute ventilation that reaches the alveoli for gas exchange
- Dead space ventilation remains unchanged
*Increasing the respiratory depth*
- Increasing respiratory depth increases **tidal volume (VT)**, which improves the **ratio** of alveolar ventilation to minute ventilation (VA/VE efficiency)
- However, the **absolute difference** (VE - VA) in L/min depends on the **total dead space volume**, which is not changed by increasing tidal volume alone
- While this improves ventilation efficiency, it does not directly reduce the dead space ventilation measured in L/min unless physiologic dead space itself decreases
*Increasing the respiratory rate*
- While increasing respiratory rate increases **minute ventilation (VE)**, it also increases the frequency of ventilating the **dead space** with each breath
- Since dead space ventilation (VD) = respiratory rate × dead space volume, increasing rate while keeping tidal volume constant will proportionally increase both VE and VD
- This can actually widen the absolute gap between VE and VA, making it less efficient
Normal V/Q distribution US Medical PG Question 9: A 62-year-old man is brought to the emergency department with a 2-day history of cough productive of yellowish sputum. He has had fever, chills, and worsening shortness of breath over this time. He has a 10-year history of hypertension and hyperlipidemia. He does not drink alcohol or smoke cigarettes. His current medications include atorvastatin, amlodipine, and metoprolol. His temperature is 38.9°C (102.0°F), pulse is 105/min, respirations are 27/min, and blood pressure is 110/70 mm Hg. He appears in mild distress. He has rales over the left lower lung field. The remainder of the examination shows no abnormalities. Leukocyte count is 15,000/mm3 (87% segmented neutrophils). Arterial blood gas analysis on room air shows:
pH 7.44
pO2 68 mm Hg
pCO2 28 mm Hg
HCO3- 24 mEq/L
O2 saturation 91%
An x-ray of the chest shows a consolidation in the left lower lobe. Asking the patient to lie down in the left lateral decubitus position would most likely result in which of the following?
- A. Decreased ventilation of the left lung
- B. Worsen the hypocapnia
- C. Increase in A-a gradient (Correct Answer)
- D. Increased perfusion of right lung
- E. Improve the hypoxemia
Normal V/Q distribution Explanation: ***Increase in A-a gradient***
- Placing the patient in the **left lateral decubitus position** would worsen V/Q mismatch because the **diseased left lung** (with consolidation) would receive increased perfusion due to gravity.
- This increased perfusion to a poorly ventilated area would further impair gas exchange, leading to a larger **alveolar-arterial (A-a) gradient**.
*Decreased ventilation of the left lung*
- While lying on the left side might slightly restrict the expansion of the left lung, the primary issue is the **consolidation** itself, which already severely impairs ventilation.
- The main problem with positioning is not a further decrease in ventilation but rather the **redistribution of blood flow** to an already compromised lung.
*Worsen the hypocapnia*
- The patient has **hypocapnia (pCO2 28 mm Hg)** due to tachypnea as compensation for hypoxemia, indicating increased minute ventilation.
- While worsening the V/Q mismatch will worsen hypoxemia, it's unlikely to directly worsen hypocapnia further; the body would still try to compensate through increased respiratory drive unless the respiratory muscles become fatigued.
*Increased perfusion of right lung*
- In the left lateral decubitus position, **perfusion due to gravity** would increase in the dependent (left) lung, not the non-dependent (right) lung.
- The right lung would experience relatively decreased perfusion compared to the left lung in this position.
*Improve the hypoxemia*
- Lying on the side of the **diseased lung** (left) typically **worsens hypoxemia** because gravity directs more blood flow to the poorly ventilated, consolidated lung.
- To improve hypoxemia, the patient should be positioned with the **healthy lung dependent** (e.g., right lateral decubitus or semi-Fowler's with the right lung lower) to optimize V/Q matching.
Normal V/Q distribution US Medical PG Question 10: A 52-year-old woman presents to the emergency department with breathlessness for the past 6 hours. She denies cough, nasal congestion or discharge, sneezing, blood in sputum, or palpitation. There is no past history of chronic respiratory or cardiovascular medical conditions, but she mentions that she has been experiencing frequent cramps in her left leg for the past 5 days. She is post-menopausal and has been on hormone replacement therapy for a year now. Her temperature is 38.3°C (100.9°F), the pulse is 116/min, the blood pressure is 136/84 mm Hg, and the respiratory rate is 24/min. Edema and tenderness are present in her left calf region. Auscultation of the chest reveals rales over the left infrascapular and scapular region. The heart sounds are normal and there are no murmurs. Which of the following mechanisms most likely contributed to the pathophysiology of this patient’s condition?
- A. Secretion of vasodilating neurohumoral substances in pulmonary vascular bed
- B. Increased right ventricular preload (Correct Answer)
- C. Decreased physiologic dead space
- D. Alveolar hyperventilation
- E. Decreased alveolar-arterial oxygen tension gradient
Normal V/Q distribution Explanation: ***Increased right ventricular preload***
- The patient's presentation (acute breathlessness, unilateral leg cramps, calf tenderness and edema, rales) combined with risk factors (post-menopausal, hormone replacement therapy) strongly suggests **pulmonary embolism (PE)** from deep vein thrombosis (DVT).
- In PE, thrombus occludes pulmonary vasculature causing **increased pulmonary vascular resistance**, which increases **right ventricular afterload** (the resistance the RV must overcome to eject blood).
- **Note:** While this option states "preload," the primary mechanism is actually increased RV **afterload**. However, this is the most appropriate answer among the given options, as the increased resistance does lead to RV strain and potential backup of blood that can secondarily affect preload.
*Secretion of vasodilating neurohumoral substances in pulmonary vascular bed*
- The primary vascular response in PE is **vasoconstriction**, not vasodilation.
- Hypoxia and mediator release cause **pulmonary vasoconstriction** distal to the embolus, further increasing pulmonary vascular resistance.
*Decreased physiologic dead space*
- In PE, there is **ventilation-perfusion (V/Q) mismatch** where lung regions are ventilated but not perfused due to embolic obstruction.
- This actually **increases physiologic dead space** because these areas are ventilated but cannot participate in gas exchange.
*Alveolar hyperventilation*
- Patients with PE often develop **tachypnea and hyperventilation** due to hypoxia, anxiety, and chest discomfort.
- However, this is a **compensatory response** to hypoxemia, not the primary pathophysiological mechanism causing the condition.
*Decreased alveolar-arterial oxygen tension gradient*
- The **A-a gradient is increased in PE** due to V/Q mismatch and shunting, reflecting impaired gas exchange.
- A decreased A-a gradient would indicate efficient gas exchange, which contradicts the hypoxia and breathlessness seen in PE.
More Normal V/Q distribution US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.