Temperature regulation in neonates US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Temperature regulation in neonates. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Temperature regulation in neonates US Medical PG Question 1: A 5-day-old male newborn is brought to the emergency department 1 hour after having a seizure. It lasted approximately 1 minute, and involved blinking and lip-smacking movements as well as left-sided jerking of the hand and foot. His mother says she measured a temperature of 38.2°C (100.7°F) at that time. He has had increasing difficulty feeding since yesterday. He was born at 39 weeks' gestation and weighed 3189 g (7 lb, 1 oz); he currently weighs 2980 g (6 lb, 9 oz). The mother's prenatal course was significant for gonorrhea infection diagnosed early in pregnancy and treated with ceftriaxone and azithromycin combination therapy. The boy appears irritable and lethargic. His temperature is 36.0°C (96.8°F). Examination shows clusters of vesicular lesions with an erythematous base on the patient's face and trunk. There is profuse lacrimation. Laboratory studies show:
Leukocyte count 16,200/mm3
Segmented neutrophils 25%
Bands 5%
Lymphocytes 65%
Monocytes 3%
Eosinophils 2%
Serum
Glucose 80 mg/dL
A lumbar puncture is performed. Cerebrospinal fluid analysis shows a leukocyte count of 117/μL, a protein concentration of 52 mg/dL, and a glucose concentration of 58 mg/dL. Results of blood cultures are pending. Which of the following is the most appropriate pharmacotherapy?
- A. IV acyclovir (Correct Answer)
- B. IV ceftriaxone
- C. Pyrimethamine
- D. IV ganciclovir
- E. IV vancomycin
Temperature regulation in neonates Explanation: ***IV acyclovir***
- The combination of **seizures**, **vesicular lesions** on the face and trunk, **profuse lacrimation**, and **lymphocytic pleocytosis** in the CSF in a newborn is highly suggestive of **Neonatal Herpes Simplex Virus (HSV) infection**.
- **Acyclovir** is the antiviral drug of choice for treating HSV infections, especially severe systemic or CNS forms in neonates, to reduce morbidity and mortality.
*IV ceftriaxone*
- **Ceftriaxone** is a broad-spectrum antibiotic primarily used to treat bacterial infections like neonatal sepsis or meningitis, but it has no activity against viruses.
- The patient's clinical presentation, including vesicular lesions and specific CSF findings, points away from a primary bacterial infection.
*Pyrimethamine*
- **Pyrimethamine** is an antiparasitic drug used in combination with sulfadiazine for treating **toxoplasmosis**.
- The patient's symptoms are not consistent with congenital toxoplasmosis, which typically involves chorioretinitis, hydrocephalus, and intracranial calcifications.
*IV ganciclovir*
- **Ganciclovir** is an antiviral primarily used for treating **cytomegalovirus (CMV) infections**, particularly in immunocompromised patients.
- While CMV can cause CNS disease in neonates, the characteristic **vesicular lesions** and **profuse lacrimation** are far more indicative of HSV.
*IV vancomycin*
- **Vancomycin** is an antibiotic used to treat severe bacterial infections, especially those caused by **methicillin-resistant Staphylococcus aureus (MRSA)** or other gram-positive bacteria.
- It is not effective against viral infections, and the clinical picture does not suggest a bacterial etiology requiring vancomycin.
Temperature regulation in neonates US Medical PG Question 2: A 10-day-old male infant is brought to the emergency room for abdominal distension for the past day. His mother reports that he has been refusing feeds for about 1 day and appears more lethargic than usual. While changing his diaper today, she noticed that the baby felt warm. He has about 1-2 wet diapers a day and has 1-2 seedy stools a day. The mother reports an uncomplicated vaginal delivery. His past medical history is significant for moderate respiratory distress following birth that has since resolved. His temperature is 101°F (38.3°C), blood pressure is 98/69 mmHg, pulse is 174/min, respirations are 47/min, and oxygen saturation is 99% on room air. A physical examination demonstrates a baby in moderate distress with abdominal distension. What is the best initial step in the management of this patient?
- A. Radionuclide scan
- B. Voiding cystourethrogram
- C. Renal ultrasound
- D. Urinary catheterization
- E. Start IV fluids and antibiotics (Correct Answer)
Temperature regulation in neonates Explanation: ***Start IV fluids and antibiotics***
- This infant presents with **fever**, **lethargy**, **abdominal distension**, and poor feeding in the setting of a history of respiratory distress, which is highly concerning for **sepsis** with possible **necrotizing enterocolitis (NEC)** or another serious bacterial infection.
- The infant is **ill-appearing and in moderate distress** - this requires **immediate empiric antibiotic therapy** and supportive care with **IV fluids** to stabilize the patient.
- While cultures (blood, urine, and possibly CSF) should be obtained, **antibiotics must NOT be delayed** in a toxic-appearing neonate. The standard approach is to obtain cultures quickly and start antibiotics immediately.
- **NEC** is a surgical emergency in neonates, especially those with risk factors like prematurity (suggested by the respiratory distress history), and requires urgent broad-spectrum antibiotics, bowel rest (NPO), and IV fluids.
*Urinary catheterization*
- While **urinary catheterization** is important to obtain a sterile urine specimen for culture in a febrile infant, it is **part of the workup**, not the "best initial step" when a child is this ill.
- Cultures should be obtained rapidly, but treatment should begin immediately - you do not delay life-saving antibiotics just to get a urine culture first.
- In this case, the primary concern is **abdominal pathology (NEC)** rather than isolated UTI.
*Radionuclide scan*
- A **radionuclide scan** (DMSA scan) is used to detect renal scarring after a confirmed UTI and has no role in the acute management of a septic neonate.
- This would provide no useful information for immediate diagnosis or treatment.
*Voiding cystourethrogram*
- A **voiding cystourethrogram (VCUG)** evaluates for **vesicoureteral reflux** and is performed weeks after a febrile UTI has been treated, not during acute presentation.
- This is completely inappropriate for an acutely ill neonate with abdominal distension.
*Renal ultrasound*
- A **renal ultrasound** assesses renal anatomy and structural abnormalities but does not diagnose acute infection and does not address the primary concern of abdominal distension.
- While it may be part of a later workup for febrile UTI, it is not the priority in a toxic-appearing infant who needs immediate stabilization and treatment.
Temperature regulation in neonates US Medical PG Question 3: A 27-year-old woman gives birth to a boy at 36 weeks gestational age. The infant weighs 4022 grams at birth, is noted to have a malformed sacrum, and appears to be in respiratory distress. Apgar scores are 5 and 7 at 1 minute and 5 minutes respectively. Hours after birth, the infant is found to be irritable, bradycardic, cyanotic, and hypotonic, and the infant's serum is sent to the laboratory for evaluation. Which of the following abnormalities would you expect to observe in this infant?
- A. Hypoinsulinemia
- B. Hypoglycemia (Correct Answer)
- C. Hyperglycemia
- D. Hypermagnesemia
- E. Hypercalcemia
Temperature regulation in neonates Explanation: ***Hypoglycemia***
- The infant is macrosomic (4022g at 36 weeks), indicating potential **maternal diabetes**, which often leads to fetal **hyperinsulinemia** and subsequent rapid glucose consumption after birth.
- Symptoms like irritability, bradycardia, cyanosis, and hypotonia are classic signs of neonatal hypoglycemia due to inadequate glucose supply for metabolic demands.
*Hypoinsulinemia*
- Maternal diabetes typically causes **fetal hyperglycemia**, leading to reactive fetal **hyperinsulinemia** as the fetal pancreas attempts to regulate glucose.
- After birth, the sudden cessation of maternal glucose supply to a hyperinsulinemic infant rapidly leads to hypoglycemia, not hypoinsulinemia.
*Hyperglycemia*
- While the infant experienced hyperglycemia *in utero* due to maternal diabetes, after birth and the separation from the maternal glucose supply, the infant's own hyperinsulinemia would rapidly consume endogenous glucose, leading to **hypoglycemia**.
- Neonatal hyperglycemia is more common in stressed or very low birth weight infants receiving excessive intravenous glucose, which is not described.
*Hypermagnesemia*
- **Hypermagnesemia** in newborns is typically associated with maternal treatment with magnesium sulfate for preeclampsia, which is not mentioned in the clinical scenario.
- Common symptoms include respiratory depression, hypotonia, and decreased reflexes, but **hypoglycemia** is a more direct and expected complication given the infant's macrosomia and maternal diabetes association.
*Hypercalcemia*
- Neonatal **hypercalcemia** is rare and is often associated with genetic conditions like Williams syndrome or idiopathic infantile hypercalcemia.
- Hypoglycemia is a much more common finding in infants of diabetic mothers, and there is no indication for hypercalcemia in this presentation.
Temperature regulation in neonates US Medical PG Question 4: An infant boy of unknown age and medical history is dropped off in the emergency department. The infant appears lethargic and has a large protruding tongue. Although the infant exhibits signs of neglect, he is in no apparent distress. The heart rate is 70/min, the respiratory rate is 30/min, and the temperature is 35.7°C (96.2°F). Which of the following is the most likely cause of the patient’s physical exam findings?
- A. Autosomal dominant mutation in the SERPING1 gene
- B. Genetic imprinting disorder affecting chromosome 11p15.5
- C. Type I hypersensitivity reaction
- D. Excess growth hormone secondary to pituitary gland tumor
- E. Congenital agenesis of an endocrine gland in the anterior neck (Correct Answer)
Temperature regulation in neonates Explanation: ***Congenital agenesis of an endocrine gland in the anterior neck***
- This description is highly suggestive of **congenital hypothyroidism**, caused by **thyroid dysgenesis** (agenesis or hypoplasia of the thyroid gland).
- Symptoms include **lethargy**, **macroglossia** (large protruding tongue), **hypotonia**, **feeding difficulties**, **umbilical hernia**, and **hypothermia**, all consistent with the clinical picture.
*Autosomal dominant mutation in the SERPING1 gene*
- A mutation in the **SERPING1 gene** causes **hereditary angioedema**, characterized by recurrent episodes of unpredictable swelling in various body parts.
- While swelling can affect the tongue, it is typically episodic, painful, and often triggered, which is not suggested by the chronic lethargy and physical signs described.
*Genetic imprinting disorder affecting chromosome 11p15.5*
- This describes **Beckwith-Wiedemann syndrome**, an overgrowth disorder caused by imprinting defects involving genes like **IGF2**, **H19**, and **CDKN1C** on chromosome 11p15.5.
- Features include **macroglossia**, **macrosomia**, **umbilical hernia**, **hemihyperplasia**, and increased risk of embryonal tumors like **Wilms tumor**.
- However, Beckwith-Wiedemann syndrome does not typically present with profound **lethargy** and **hypothermia** as seen in congenital hypothyroidism.
*Type I hypersensitivity reaction*
- A **Type I hypersensitivity reaction** (e.g., anaphylaxis) could cause acute **angioedema** of the tongue, but this would be an acute, rapidly progressing, and life-threatening event.
- The infant's description of being "in no apparent distress" and exhibiting chronic signs like lethargy and hypothermia makes an acute allergic reaction unlikely.
*Excess growth hormone secondary to pituitary gland tumor*
- **Excess growth hormone** (gigantism in children, acromegaly in adults) can cause **macroglossia** and coarse facial features in the long term.
- However, it does not explain the associated **lethargia**, **hypothermia**, and profound developmental delay seen in congenital hypothyroidism in an infant.
Temperature regulation in neonates US Medical PG Question 5: A 20-year-old woman reports to student health complaining of 5 days of viral symptoms including sneezing and a runny nose. She started coughing 2 days ago and is seeking cough medication. She additionally mentions that she developed a fever 2 days ago, but this has resolved. On exam, her temperature is 99.0°F (37.2°C), blood pressure is 118/76 mmHg, pulse is 86/min, and respirations are 12/min. Changes in the activity of warm-sensitive neurons in which part of her hypothalamus likely contributed to the development and resolution of her fever?
- A. Anterior hypothalamus (Correct Answer)
- B. Paraventricular nucleus
- C. Suprachiasmatic nucleus
- D. Lateral area
- E. Posterior hypothalamus
Temperature regulation in neonates Explanation: ***Anterior hypothalamus***
- The **anterior hypothalamus** contains warm-sensitive neurons that detect increases in body temperature and activate mechanisms for heat dissipation, such as sweating and vasodilation.
- In fever, **prostaglandins** increase the set point in the anterior hypothalamus, causing the body to retain heat and increase heat production until the new set point is reached; resolution of fever involves resetting this set point back to normal.
*Paraventricular nucleus*
- The **paraventricular nucleus** is primarily involved in neuroendocrine functions, stress response, and the regulation of appetite and autonomic nervous system.
- It plays a significant role in releasing hormones like **corticotropin-releasing hormone (CRH)** and **oxytocin**, not direct temperature regulation.
*Suprachiasmatic nucleus*
- The **suprachiasmatic nucleus (SCN)** is the body's main biological clock, regulating **circadian rhythms** including the sleep-wake cycle and daily fluctuations in body temperature.
- While it influences the normal diurnal variation in body temperature, it is not directly responsible for the acute regulation of fever.
*Lateral area*
- The **lateral hypothalamus** primarily functions as the "hunger center," stimulating foraging and feeding behavior.
- Damage to this area can lead to **anorexia** and reduced food intake, not impairments in fever response.
*Posterior hypothalamus*
- The **posterior hypothalamus** is primarily involved in heat conservation and production mechanisms, such as shivering and vasoconstriction, in response to cold.
- It contains cold-sensitive neurons and functions to raise body temperature if it falls below the set point, but it is not where the set point itself is regulated in response to pyrogens.
Temperature regulation in neonates US Medical PG Question 6: Two days after delivery, a 4300-g (9-lb 8-oz) newborn has difficulty feeding and has become increasingly lethargic. His cry has become weak. He was born at term. His mother has a history of intravenous drug use. His temperature is 36.4°C (96.5°F), pulse is 170/min, respirations are 62/min, and blood pressure is 70/48 mm Hg. Examination shows midfacial hypoplasia, diaphoresis, and tremor of the lower extremities. Macroglossia is present. There are folds in the posterior auricular cartilage. The left lower extremity is larger than the right lower extremity. Abdominal examination shows an umbilical hernia. The liver is palpated 4 cm below the right costal margin. Neurological examination shows decreased tone in all extremities. Which of the following is the most appropriate intervention?
- A. Administer naloxone
- B. Administer 3% saline
- C. Administer thyroxine
- D. Administer glucose (Correct Answer)
- E. Administer ampicillin and gentamicin
Temperature regulation in neonates Explanation: ***Administer glucose***
- The presented symptoms, including **lethargy**, **weak cry**, **diaphoresis**, **tremor**, and **hypotonia**, are highly suggestive of **neonatal hypoglycemia**, which requires immediate treatment.
- The physical findings (macroglossia, hemihypertrophy, umbilical hernia, hepatomegaly) suggest **Beckwith-Wiedemann syndrome (BWS)**, a condition associated with **high risk of severe hypoglycemia** in the neonatal period.
- The **large for gestational age (LGA)** birth weight (4300g) further increases hypoglycemia risk.
- **Immediate glucose administration** is life-saving and takes priority over other diagnostic considerations.
*Administer naloxone*
- While the mother has a history of intravenous drug use, the clinical presentation is not consistent with acute opioid toxicity (which would present with respiratory depression, miosis, and decreased consciousness immediately after birth).
- The constellation of dysmorphic features and metabolic symptoms points to **hypoglycemia**, not opioid exposure.
- Naloxone is contraindicated in neonates of opioid-dependent mothers as it may precipitate severe withdrawal.
*Administer 3% saline*
- **Hypertonic saline (3% saline)** is used to treat **severe symptomatic hyponatremia** with seizures or altered mental status.
- There is no clinical indication for hyponatremia in this case; the symptoms are classic for **hypoglycemia**.
- Administering hypertonic saline without documented hyponatremia could cause dangerous complications.
*Administer thyroxine*
- **Macroglossia**, **umbilical hernia**, **hypotonia**, and **posterior auricular folds** can be signs of **congenital hypothyroidism**.
- However, congenital hypothyroidism presents with gradual onset of symptoms over weeks, not acute decompensation at 2 days of life.
- The acute symptoms (diaphoresis, tremors, lethargy) and associated findings (hemihypertrophy, hepatomegaly) are more consistent with **BWS-associated hypoglycemia**.
- Hypothyroidism workup can be pursued after stabilizing the acute hypoglycemia.
*Administer ampicillin and gentamicin*
- **Broad-spectrum antibiotics** are used for suspected **neonatal sepsis**, which can present with lethargy, poor feeding, and temperature instability.
- While sepsis should always be considered in an ill neonate, the specific constellation of dysmorphic features (macroglossia, hemihypertrophy, umbilical hernia) strongly suggests **Beckwith-Wiedemann syndrome**.
- The symptoms of diaphoresis and tremor are more specific for **hypoglycemia** than infection.
- A sepsis workup may be warranted, but **correcting hypoglycemia is the most urgent intervention**.
Temperature regulation in neonates US Medical PG Question 7: Thirty minutes after delivery, a 1780-g (3-lb 15-oz) male newborn develops respiratory distress. He was born at 30 weeks' gestation via vaginal delivery. His temperature is 36.8C (98.2F), pulse is 140/min, respirations are 64/min, and blood pressure is 61/32 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 90%. Examination shows pale extremities. Grunting and moderate subcostal retractions are present. Pulmonary examination shows decreased breath sounds bilaterally. Supplemental oxygen is administered. Ten minutes later, his pulse is 148/min and respirations are 66/min. Pulse oximetry on 60% oxygen shows an oxygen saturation of 90%. Which of the following is the most likely diagnosis?
- A. Meconium aspiration syndrome
- B. Tracheomalacia
- C. Tracheoesophageal fistula
- D. Neonatal pneumonia
- E. Respiratory distress syndrome (Correct Answer)
Temperature regulation in neonates Explanation: ***Respiratory distress syndrome***
- This premature newborn (30 weeks' gestation, 1780-g) with immediate **respiratory distress**, grunting, retractions, and poor oxygenation despite supplemental oxygen is highly indicative of **respiratory distress syndrome (RDS)** due to surfactant deficiency.
- The **decreased breath sounds bilaterally** are consistent with widespread atelectasis characteristic of RDS.
*Meconium aspiration syndrome*
- This typically occurs in **term or post-term infants** and is unlikely in a 30-week premature infant.
- It usually presents with a history of **meconium-stained amniotic fluid** and chest X-ray findings of patchy infiltrates and hyperinflation.
*Tracheomalacia*
- This condition involves **weakness of the tracheal walls** leading to airway collapse, often presenting with a **barking cough** or **stridor**.
- It does not typically cause the severe, rapidly worsening respiratory distress and diffuse lung findings seen in this case.
*Tracheoesophageal fistula*
- This typically presents with **choking, coughing, and cyanosis during feeding**, due to aspiration of milk into the trachea.
- Respiratory distress in this condition is usually associated with feeding, and there is no mention of feeding issues in this scenario.
*Neonatal pneumonia*
- While possible in a premature infant, pneumonia symptoms often include **fever** and specific chest X-ray findings (e.g., infiltrates), which are not emphasized here.
- The rapid onset immediately after birth and progressive nature in a preterm infant strongly point towards a primary respiratory developmental issue like RDS.
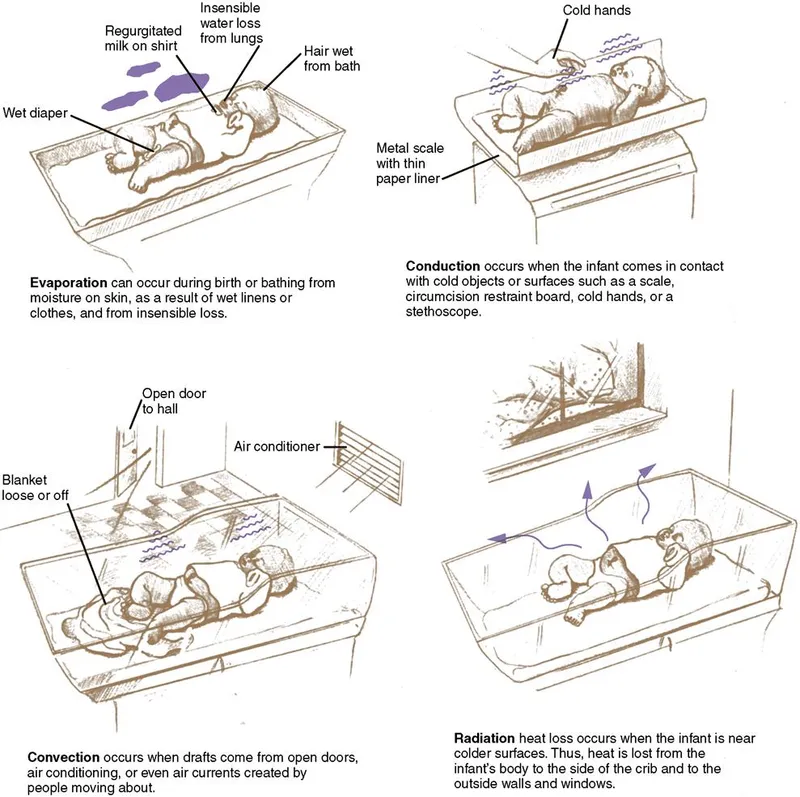
Temperature regulation in neonates US Medical PG Question 8: A group of investigators is studying thermoregulatory adaptations of the human body. A subject is seated in a thermally insulated isolation chamber with an internal temperature of 48°C (118°F), a pressure of 1 atmosphere, and a relative humidity of 10%. Which of the following is the primary mechanism of heat loss in this subject?
- A. Convection
- B. Evaporation (Correct Answer)
- C. Conduction
- D. Piloerection
- E. Radiation
Temperature regulation in neonates Explanation: ***Evaporation***
- In an environment where the ambient temperature (48°C) is **higher than body temperature**, heat gain by convection, conduction, and radiation occurs. Therefore, **evaporation** of sweat is the only significant mechanism for heat loss.
- The relatively low humidity (10%) at this high temperature facilitates efficient sweat **evaporation**, which cools the body as it converts liquid sweat into water vapor.
*Convection*
- **Convection** involves heat transfer through the movement of air or fluid over the body surface.
- Since the ambient temperature (48°C) is significantly **above body temperature**, the body would gain heat via convection, not lose it.
*Conduction*
- **Conduction** is direct heat transfer between objects in contact.
- As the ambient temperature (48°C) is much **higher than the skin temperature**, the body would actually **gain heat** through conduction from any surfaces it touched if they were at ambient temperature.
*Piloerection*
- **Piloerection** (goosebumps) is a mechanism for minimizing heat loss by trapping a layer of warm air close to the skin.
- This response is activated in **cold environments** to conserve heat, not in hot environments to dissipate it.
*Radiation*
- **Radiation** is heat transfer via electromagnetic waves without direct contact.
- Since the ambient temperature (48°C) is **higher than body surface temperature**, the body would **gain heat** by radiation, not lose it efficiently, from the surrounding environment.
Temperature regulation in neonates US Medical PG Question 9: A 42-year-old man undergoes therapeutic hypothermia (target temperature 33°C/91.4°F) following cardiac arrest with return of spontaneous circulation. During the cooling phase, he develops shivering, which increases oxygen consumption and interferes with target temperature achievement. He is already on sedation and neuromuscular blockade is being considered. Evaluate the most appropriate management strategy considering both efficacy and safety.
- A. Administer meperidine alone to reduce shivering threshold
- B. Increase sedation and add surface counter-warming of extremities before neuromuscular blockade (Correct Answer)
- C. Abandon therapeutic hypothermia due to complications
- D. Use only mechanical restraints to prevent movement
- E. Immediate neuromuscular blockade without additional measures
Temperature regulation in neonates Explanation: ***Increase sedation and add surface counter-warming of extremities before neuromuscular blockade***
- A **stepwise approach** to shivering is preferred; increasing **sedation** and using **surface counter-warming** reduces the shivering threshold by tricking the hypothalamus into sensing a warmer periphery.
- This strategy minimizes the need for **neuromuscular blockade**, which can mask seizures and prevent accurate **neurological assessment**.
*Administer meperidine alone to reduce shivering threshold*
- While **meperidine** is an effective anti-shivering agent that lowers the shivering threshold, using it **alone** is often insufficient to control vigorous shivering during induction.
- Reliance on a single pharmacologic agent ignores the **multimodal therapy** benefits of physical measures like skin warming and optimized sedation.
*Abandon therapeutic hypothermia due to complications*
- Shivering is a predictable physiological response, not a reason to abandon **Targeted Temperature Management (TTM)**, which provides significant **neuroprotection** post-cardiac arrest.
- Stopping the therapy would deprive the patient of the benefit of reduced **cerebral metabolic rate** and improved survival outcomes.
*Use only mechanical restraints to prevent movement*
- Mechanical restraints are ineffective against the **metabolic consequences** of shivering, such as increased **oxygen consumption** and CO2 production.
- Shivering is a thermoregulatory reflex, and physical restraint does not stop the underlying **thermogenesis** or metabolic demand.
*Immediate neuromuscular blockade without additional measures*
- **Neuromuscular blockade** should be a last resort as it carries risks of **prolonged muscle weakness** and obscures the patient's clinical neurological status.
- It treats the muscular manifestation but lacks the **sedative or analgesic** properties needed to comfort the patient during the cooling process.
Temperature regulation in neonates US Medical PG Question 10: A 72-year-old woman with end-stage renal disease on hemodialysis develops fever (103°F/39.4°C) with rigors during dialysis. Blood cultures from both the dialysis catheter and peripheral site grow gram-positive cocci. Despite appropriate antibiotics and catheter removal, she has persistent fevers of 101-102°F (38.3-38.9°C) for 7 days. She feels better and inflammatory markers are decreasing. Evaluate the most likely explanation for persistent fever.
- A. Appropriate lag in temperature resolution despite adequate treatment (Correct Answer)
- B. Undrained abscess requiring surgical intervention
- C. Drug fever from antibiotic therapy
- D. Inadequate dialysis causing uremic fever
- E. Antibiotic-resistant organism requiring regimen change
Temperature regulation in neonates Explanation: ***Appropriate lag in temperature resolution despite adequate treatment***
- In bacteremia, fever can persist for several days even with effective therapy because **inflammatory cytokines** (like IL-1 and TNF-α) and bacterial products take time to clear from the system.
- The clinical improvement and **decreasing inflammatory markers** (like CRP or ESR) are the most reliable indicators of a positive response to treatment, despite the slow normalization of the **hypothalamic set point**.
*Undrained abscess requiring surgical intervention*
- While a persistent fever can indicate an **occult abscess**, this is less likely when the patient reports feeling clinically better and lab trends are improving.
- Persistent bacteremia or clinical worsening, rather than just isolated fever, would typically necessitate intensive imaging for deep-seated **foci of infection**.
*Drug fever from antibiotic therapy*
- Drug fever is a diagnosis of exclusion that usually occurs after **7 to 10 days** of therapy and is often associated with a newly developed rash or eosinophilia.
- In this case, the patient's fever started with a known **bacterial source** (dialysis catheter), making an infectious resolution lag much more probable than a drug reaction.
*Inadequate dialysis causing uremic fever*
- **Uremia** is more commonly associated with **hypothermia** or a blunted febrile response rather than a high persistent fever.
- Modern dialysis efficiently prevents the build-up of metabolic toxins to levels that would trigger a high-grade **febrile state**.
*Antibiotic-resistant organism requiring regimen change*
- Resistance is unlikely here because the patient is showing **clinical improvement** and a downward trend in inflammatory markers, indicating the current regimen is effective.
- If a **resistant organism** were present, you would expect temperatures to remain very high or increase, and blood cultures to remain positive after 48-72 hours of therapy.
More Temperature regulation in neonates US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.