Hypothermia pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypothermia pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypothermia pathophysiology US Medical PG Question 1: An 84-year-old man presents to the emergency department for a loss of consciousness. The patient states that he was using the bathroom when he lost consciousness and fell, hitting his head on the counter. The patient has a past medical history of diabetes, hypertension, obesity, factor V leiden, constipation, myocardial infarction, and vascular claudication. His current medications include lisinopril, atorvastatin, valproic acid, propranolol, insulin, metformin, and sodium docusate. The patient denies use of illicit substances. His temperature is 99.5°F (37.5°C), blood pressure is 167/98 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam reveals an elderly man sitting comfortably in his stretcher. Cardiac exam reveals a systolic murmur heard at the right upper sternal border that radiates to the carotids. Pulmonary exam reveals mild bibasilar crackles. Neurological exam reveals 5/5 strength in his upper and lower extremities with normal sensation. The patient's gait is mildly unstable. The patient is unable to give a urine sample in the emergency department and states that he almost fainted again when he tried to. Which of the following is the most likely diagnosis?
- A. Seizure
- B. Cardiac arrhythmia
- C. Postural hypotension
- D. Situational syncope (Correct Answer)
- E. Transient ischemic attack
Hypothermia pathophysiology Explanation: ***Situational syncope***
- The patient's loss of consciousness while **straining during defecation** (using the bathroom) is highly suggestive of **situational syncope**, which is a type of **reflex syncope** triggered by specific actions.
- His complaint of almost fainting again when trying to provide a urine sample reinforces the diagnosis, as **micturition (urination) syncope** is another common form of situational syncope.
*Seizure*
- While a loss of consciousness occurred, the patient's presentation lacks typical features of a seizure such as a **postictal state**, tongue biting, or tonic-clonic movements.
- The trigger (straining) and the near-syncopal episode with micturition are inconsistent with a primary seizure disorder.
*Cardiac arrhythmia*
- Although the patient has a history of myocardial infarction and is on **propranolol** (a beta-blocker), there are no specific findings on physical exam or in the history to strongly suggest an arrhythmia as the cause of syncope.
- An arrhythmia-induced syncope typically doesn't have such a clear situational trigger like defecation or urination.
*Postural hypotension*
- Postural hypotension is characterized by a significant drop in blood pressure upon standing, leading to symptoms like dizziness or syncope.
- While the patient is on several medications that could contribute to hypotension (e.g., lisinopril, propranolol), the syncope was specifically associated with straining, not just standing up.
*Transient ischemic attack*
- A TIA involves **transient neurological deficits** such as weakness, sensory changes, or speech disturbances, which typically last minutes to hours.
- A transient loss of consciousness without focal neurological symptoms is not characteristic of a TIA.
Hypothermia pathophysiology US Medical PG Question 2: A 15-year-old boy is brought to the emergency department by his father 10 minutes after falling into a frozen lake during ice fishing. He was in the water for less than 1 minute before his father managed to pull him out. On arrival, his clothes are still wet and he appears scared. His body temperature is 36.2°C (97.1°F), pulse is 102/min, blood pressure is 133/88 mm Hg. Which of the following mechanisms contributes most to maintaining this patient's core body temperature?
- A. Inhibition of the thyroid axis
- B. Involuntary muscular contractions (Correct Answer)
- C. Activation of thermogenin
- D. Increase in hypothalamic set point
- E. Contraction of arrector pili muscles
Hypothermia pathophysiology Explanation: ***Involuntary muscular contractions***
- **Shivering** is the body's primary mechanism for increasing heat production in response to cold stress, involving rapid, involuntary muscle contractions to generate heat.
- This process significantly increases the **metabolic rate** and heat output, crucial for maintaining core body temperature when exposed to cold environments.
*Inhibition of the thyroid axis*
- The **thyroid axis** is generally activated in response to chronic cold exposure to increase basal metabolic rate, not inhibited.
- Inhibition of thyroid hormones would lead to a decrease in metabolism and heat production, worsening hypothermia.
*Activation of thermogenin*
- **Thermogenin** (uncoupling protein 1) is found primarily in **brown adipose tissue** and its activation leads to non-shivering thermogenesis.
- While present in infants and some adults, shivering is a much more significant and rapid response to acute cold in a 15-year-old.
*Increase in hypothalamic set point*
- An increase in the **hypothalamic set point** is characteristic of **fever**, where the body aims to achieve a higher temperature.
- In this scenario, the body is trying to maintain its normal set point despite cold exposure, not raise it.
*Contraction of arrector pili muscles*
- **Contraction of arrector pili muscles** causes **piloerection** (goosebumps), which traps a layer of air close to the skin.
- While contributing to insulation, this mechanism is relatively minor in humans compared to the heat generated by shivering.
Hypothermia pathophysiology US Medical PG Question 3: A 37-year-old man is brought to the emergency department by a friend after he was found lying unconscious outside his front door. The friend reports that they were “pretty drunk” the previous night, and she had dropped her friend off at his home and driven off. When she came back in the morning, she found him passed out on the ground next to the doorstep. On arrival, he is conscious and cooperative. He reports feeling cold, with severe pain in his hands and face. He remembers having lost his gloves last night. His rectal temperature is 35.2°C (95.3°F), pulse is 86/min, respirations are 17/min, and blood pressure is 124/58 mm Hg. Examination shows decreased sensations over the distal fingers, which are cold to touch. The skin over the distal phalanges is cyanotic, hard, waxy, and tender, with surrounding edema. Laboratory studies are within the reference range. An x-ray of the chest and ECG show no abnormalities. Which of the following is the most appropriate next step in management?
- A. Intravenous administration of warmed crystalloid
- B. Debridement of the affected tissue
- C. Immersion of affected extremities in warm water (Correct Answer)
- D. Intra-arterial administration of tissue plasminogen activator
- E. Intravenous administration of antibiotics
Hypothermia pathophysiology Explanation: ***Immersion of affected extremities in warm water***
- The patient presents with **frostbite** (cyanotic, hard, waxy skin with decreased sensation after cold exposure), and **rapid rewarming** with warm water (37-39°C or 98.6-102.2°F) is the most effective initial treatment.
- This method provides continuous, even heat transfer to optimize tissue perfusion and minimize damage.
*Intravenous administration of warmed crystalloid*
- While this patient has mild **hypothermia** (35.2°C), his vital signs are stable, and the primary concern is localized frostbite.
- **Core rewarming** with warmed crystalloids is typically reserved for more severe hypothermia or hemodynamic instability.
*Debridement of the affected tissue*
- **Debridement** of frostbitten tissue is **contraindicated** in the initial stages as it can cause further damage and make the assessment of viable tissue more difficult.
- Surgical intervention is usually delayed until the full extent of tissue damage is clear, which can take several days to weeks.
*Intra-arterial administration of tissue plasminogen activator*
- **Thrombolytics** like tPA might be considered in severe frostbite with evidence of **vascular compromise** if administered within 24 hours of thawing.
- However, it is an **advanced and invasive treatment**, and the immediate priority is always rewarming.
*Intravenous administration of antibiotics*
- **Prophylactic antibiotics** are generally **not recommended** for frostbite as they do not prevent infection and can promote antibiotic resistance.
- Antibiotics should only be used if there is clear evidence of **secondary infection**.
Hypothermia pathophysiology US Medical PG Question 4: An 11-year-old boy presents with a 2-day history of uncontrollable shivering. During admission, the patient’s vital signs are within normal limits, except for a fluctuating body temperature registering as low as 35.0°C (95.0°F) and as high as 40.0°C (104.0°F), requiring alternating use of cooling and warming blankets. A complete blood count (CBC) is normal, and a chest radiograph is negative for consolidations and infiltrates. An MRI of the brain reveals a space-occupying lesion infiltrating the posterior hypothalamus and extending laterally. Which of the following additional findings are most likely, based on this patient’s physical examination?
- A. Polyuria
- B. Hyperphagia
- C. Galactorrhea
- D. Sleep disturbances
- E. Anorexia (Correct Answer)
Hypothermia pathophysiology Explanation: **Anorexia**
- **Hypothalamic lesions**, particularly those affecting the **lateral hypothalamus**, often lead to **anorexia** and **weight loss** due to the role of this region in stimulating appetite.
- The patient's presentation with **uncontrollable shivering** and **deregulated body temperature** further points to hypothalamic dysfunction, which can also disrupt feeding centers.
*Polyuria*
- **Polyuria** is typically associated with damage to the **posterior pituitary gland** or its connections to the hypothalamus, leading to **diabetes insipidus** (lack of ADH).
- While a hypothalamic lesion can affect ADH production, the primary symptom constellation in this case more strongly suggests disruption of other hypothalamic functions.
*Hyperphagia*
- **Hyperphagia** (increased appetite) and **obesity** are most commonly linked to damage to the **ventromedial hypothalamus**, which is considered the satiety center.
- The presented lesion is described as infiltrating the posterior hypothalamus and extending laterally, making hyperphagia less likely than anorexia.
*Galactorrhea*
- **Galactorrhea** is often caused by **hyperprolactinemia**, which can result from lesions compressing the **pituitary stalk** or interfering with **dopamine's inhibitory effect** on prolactin release in the anterior pituitary.
- While a large hypothalamic lesion could theoretically impact pituitary function secondarily, galactorrhea is not a direct or most likely consequence of a posterior and lateral hypothalamic lesion.
*Sleep disturbances*
- While the **hypothalamus** plays a critical role in **sleep-wake cycles** (e.g., the **suprachiasmatic nucleus**), **uncontrollable shivering** and **poikilothermia** point more directly to acute disruption of temperature regulation rather than sleep disturbances as the most prominent likely additional finding.
- Many types of brain lesions can cause sleep disturbances, but the specific presentation here suggests a more particular set of hypothalamic dysfunctions.
Hypothermia pathophysiology US Medical PG Question 5: A cardiologist is studying how a new virus that infects the heart affects the electrical conduction system of the cardiac myocytes. He decides to obtain electrocardiograms on patients with this disease in order to see how the wave patterns and durations change over time. While studying these records, he asks a medical student who is working with him to interpret the traces. Specifically, he asks her to identify the part that represents initial ventricular depolarization. Which of the following characteristics is most consistent with this feature of the electrocardiogram?
- A. Elevated in patients with full thickness ischemic injury of the heart
- B. Becomes peaked in states of hyperkalemia
- C. Becomes prominent in states of hypokalemia
- D. Normal duration defined as less than 120 milliseconds (Correct Answer)
- E. Normal duration defined as less than 200 milliseconds
Hypothermia pathophysiology Explanation: ***Normal duration defined as less than 120 milliseconds***
- The question asks for the representation of **initial ventricular depolarization**, which corresponds to the **QRS complex** on an ECG.
- The normal duration of the **QRS complex** is typically less than **0.12 seconds (120 milliseconds)**, reflecting efficient ventricular depolarization.
*Elevated in patients with full thickness ischemic injury of the heart*
- This description refers to the **ST segment elevation** seen in **ST-segment elevation myocardial infarction (STEMI)**, which represents myocardial injury, not initial ventricular depolarization.
- While related to cardiac electrical activity, **ST segment elevation** is a consequence of injury and refers to repolarization abnormalities, not the QRS complex itself.
*Becomes peaked in states of hyperkalemia*
- **Peaked T waves** are characteristic of **hyperkalemia**, indicating altered ventricular repolarization, not ventricular depolarization.
- The T wave represents ventricular repolarization, and its morphology changes significantly with potassium imbalances.
*Becomes prominent in states of hypokalemia*
- A **prominent U wave** is sometimes observed in **hypokalemia**, which follows the T wave and is thought to represent repolarization of Purkinje fibers.
- The U wave is distinct from the QRS complex and does not represent initial ventricular depolarization.
*Normal duration defined as less than 200 milliseconds*
- A duration of less than 200 milliseconds (0.20 seconds) typically refers to the normal duration of the **PR interval**, which represents atrial depolarization and conduction through the AV node.
- The **QRS complex** (initial ventricular depolarization) has a shorter normal duration, typically less than 120 milliseconds.
Hypothermia pathophysiology US Medical PG Question 6: A 41-year-old woman presents to the emergency room with chest pain. She has had progressive substernal chest pain accompanied by weakness and mild shortness of breath for the past 2 hours. Her past medical history is notable for poorly controlled systemic lupus erythematosus (SLE), Sjogren syndrome, and interstitial lung disease. She was hospitalized last year with pericarditis presumed to be from SLE. Her temperature is 98.6°F (37°C), blood pressure is 106/56 mmHg, pulse is 132/min, and respirations are 26/min. On exam, the skin overlying the internal jugular vein fills at 9 cm above the sternal angle and distant heart sounds are appreciated. There is no friction rub. She is given 1000cc of intravenous fluids with no appreciable change in her blood pressure. An electrocardiogram in this patient would most likely reveal which of the following findings?
- A. Polymorphic P waves
- B. ST elevations in leads II, III, and aVF
- C. Peaked T waves
- D. Wide QRS complexes with no P waves
- E. Electrical alternans (Correct Answer)
Hypothermia pathophysiology Explanation: ***Electrical alternans***
- The patient's symptoms (chest pain, shortness of breath, **hypotension**, **tachycardia**, **elevated JVP**, and **distant heart sounds**) in the context of a history of **pericarditis** and **SLE** are highly suggestive of **cardiac tamponade.**
- **Electrical alternans**, characterized by alternating QRS complex heights due to the swinging motion of the heart in a large pericardial effusion, is a classic EKG finding for cardiac tamponade.
- This finding reflects the mechanical swinging of the heart within the pericardial fluid, causing beat-to-beat variation in QRS amplitude.
*Polymorphic P waves*
- **Polymorphic P waves** (multifocal atrial tachycardia) occur when there are at least three different P wave morphologies on the EKG, indicating multiple ectopic atrial foci.
- This is typically seen in patients with severe lung disease or other conditions causing increased atrial stretch, but it is not a direct consequence or typical finding of cardiac tamponade.
*ST elevations in leads II, III, and aVF*
- **ST elevations in leads II, III, and aVF** indicate an **inferior myocardial infarction**, which is caused by coronary artery occlusion.
- While chest pain is present, the patient's other signs (elevated JVP, distant heart sounds, hypotension not responding to fluids, history of pericarditis/SLE) point away from an acute MI and strongly towards cardiac tamponade.
*Peaked T waves*
- **Peaked T waves** are characteristic of **hyperkalemia**, a condition of excessively high potassium levels in the blood.
- While hyperkalemia can cause cardiac symptoms, it does not typically present with the specific hemodynamic compromise and physical exam findings (elevated JVP, distant heart sounds) described, which are classic for cardiac tamponade.
*Wide QRS complexes with no P waves*
- **Wide QRS complexes with no P waves** are characteristic of a **ventricular arrhythmia**, such as ventricular tachycardia or idioventricular rhythm.
- While the patient is hypotensive and tachycardic, the presenting symptoms and physical exam findings are not directly indicative of a primary ventricular arrhythmia, but rather suggest an extracardiac compression of the heart due to tamponade.
Hypothermia pathophysiology US Medical PG Question 7: A 33-year-old man is evaluated by paramedics after being found unconscious outside of his home. He has no palpable pulses. Physical examination shows erythematous marks in a fern-leaf pattern on his lower extremities. An ECG shows ventricular fibrillation. Which of the following is the most likely cause of this patient's findings?
- A. Infective endocarditis
- B. Lightning strike (Correct Answer)
- C. Opioid overdose
- D. Hypothermia
- E. Cholesterol emboli
Hypothermia pathophysiology Explanation: ***Lightning strike***
- The **fern-leaf pattern** on the skin, known as **Lichtenberg figures**, is pathognomonic for a lightning strike.
- **Ventricular fibrillation** is a common and often fatal cardiac arrhythmia caused by the massive electrical discharge from lightning.
*Infective endocarditis*
- While it can cause cardiac arrhythmias or collapse due to **embolism**, it does not produce **Lichtenberg figures**.
- Typical signs include **fever**, **murmurs**, and **Osler's nodes** or **Janeway lesions**, which are not mentioned here.
*Opioid overdose*
- Leads to **respiratory depression**, **miosis (pinpoint pupils)**, and potentially **bradycardia**, but not ventricular fibrillation or fern-leaf skin patterns.
- The patient would typically present with a **depressed level of consciousness** but usually has palpable pulses initially.
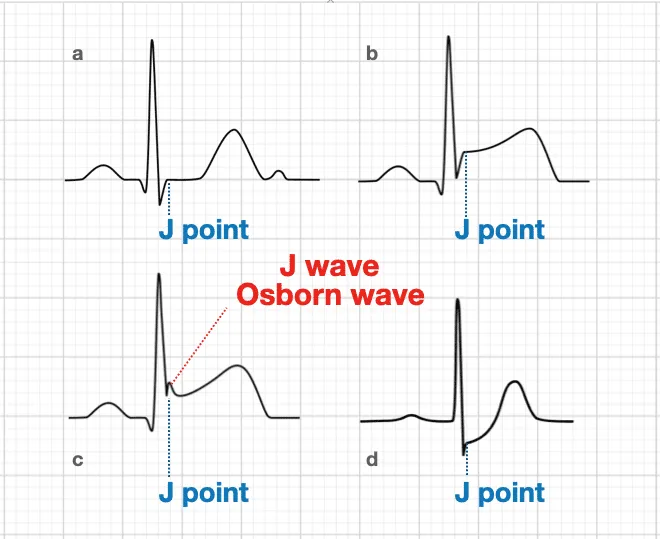
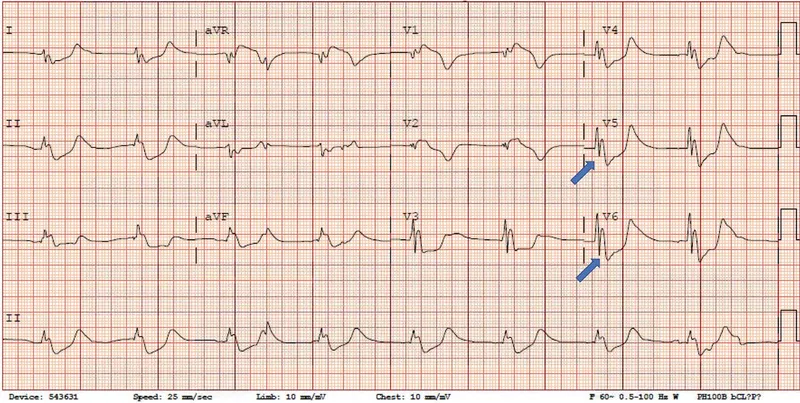
*Hypothermia*
- Can cause cardiac arrhythmias, including **ventricular fibrillation** in severe cases, but would not produce **Lichtenberg figures**.
- The patient's skin would typically be **cold to the touch**, and there might be **J-waves** on the ECG.
*Cholesterol emboli*
- Typically results in widespread **ischemic symptoms** in various organs and can cause skin manifestations like **livedo reticularis** or **"trash foot"**.
- It does not cause **ventricular fibrillation** or the characteristic **fern-leaf pattern** seen in lightning strike victims.
Hypothermia pathophysiology US Medical PG Question 8: An investigator is conducting a study on hematological factors that affect the affinity of hemoglobin for oxygen. An illustration of two graphs (A and B) that represent the affinity of hemoglobin for oxygen is shown. Which of the following best explains a shift from A to B?
- A. Decreased serum pCO2
- B. Increased serum pH
- C. Decreased serum 2,3-bisphosphoglycerate concentration
- D. Increased body temperature (Correct Answer)
- E. Increased hemoglobin γ-chain synthesis
Hypothermia pathophysiology Explanation: ***Increased body temperature***
- A shift from A to B represents a **rightward shift** of the oxygen-hemoglobin dissociation curve, indicating **decreased hemoglobin affinity for oxygen**.
- **Increased body temperature** (e.g., during exercise, fever) reduces hemoglobin's affinity for oxygen, facilitating **oxygen release to tissues**.
*Decreased serum pCO2*
- A **decrease in serum pCO2** leads to an **increase in pH** (alkalosis) and a **leftward shift** of the curve, meaning an increased affinity of hemoglobin for oxygen.
- This is part of the **Bohr effect**, where lower CO2 levels signal decreased tissue metabolic activity, thus reducing oxygen unloading.
*Increased serum pH*
- An **increase in serum pH** (alkalosis) causes a **leftward shift** of the oxygen-hemoglobin dissociation curve, signifying **increased hemoglobin affinity for oxygen**.
- This response is beneficial in the lungs, where higher pH promotes oxygen binding to hemoglobin.
*Decreased serum 2,3-bisphosphoglycerate concentration*
- A **decrease in 2,3-BPG** concentration leads to a **leftward shift** of the curve, representing **increased hemoglobin affinity for oxygen**.
- 2,3-BPG typically binds to deoxyhemoglobin, stabilizing its T-state and promoting oxygen release; thus, less 2,3-BPG means less release.
*Increased hemoglobin γ-chain synthesis*
- Increased **hemoglobin γ-chain synthesis** is characteristic of **fetal hemoglobin (HbF)**, which has a **higher affinity for oxygen** than adult hemoglobin (HbA).
- This would result in a **leftward shift** of the oxygen-hemoglobin dissociation curve, enhancing oxygen uptake by the fetus.
Hypothermia pathophysiology US Medical PG Question 9: Cardiac muscle serves many necessary functions, leading to a specific structure that serves these functions. The structure highlighted is an important histology component of cardiac muscle. What would be the outcome if this structure diffusely failed to function?
- A. Failure of potassium channels to appropriately open to repolarize the cell
- B. Failure of propagation of the action potential from the conduction system (Correct Answer)
- C. Ineffective excitation-contraction coupling due to insufficient calcium ions
- D. Inappropriate formation of cardiac valve leaflets
- E. Outflow tract obstruction
Hypothermia pathophysiology Explanation: ***Failure of propagation of the action potential from the conduction system***
- The highlighted structure, the **intercalated disc**, contains **gap junctions** which are crucial for the rapid, synchronized spread of **action potentials** between cardiac muscle cells.
- A diffuse failure of these structures would prevent the coordinated electrical activation of the myocardium, leading to a failure of impulse propagation and **compromised cardiac contraction**.
*Failure of potassium channels to appropriately open to repolarize the cell*
- This scenario describes a problem with **ion channel function** within individual cardiomyocytes, affecting their repolarization phase.
- While critical for a single cell's electrical activity, it does not directly relate to the primary function of **intercalated discs** in *propagating* action potentials across multiple cells.
*Ineffective excitation-contraction coupling due to insufficient calcium ions*
- This outcome would result from issues with **calcium handling** mechanisms, such as problems with the **sarcoplasmic reticulum** or **calcium channels**, which are internal to the cardiomyocyte.
- It is distinct from the role of **intercalated discs** in facilitating intercellular communication and electrical spread.
*Inappropriate formation of cardiac valve leaflets*
- The formation of cardiac valve leaflets is an intricate process during **embryological development** involving specific signaling pathways and cell migration.
- This structural defect is not directly related to the function of **intercalated discs** in mature cardiac muscle, which are involved in electrical and mechanical coupling.
*Outflow tract obstruction*
- **Outflow tract obstruction** is a congenital or acquired structural defect affecting the major arteries leaving the heart (e.g., aortic or pulmonary stenosis).
- This is a macroscopic structural anomaly that is not caused by a primary failure of **intercalated disc** function.
Hypothermia pathophysiology US Medical PG Question 10: A 42-year-old man undergoes therapeutic hypothermia (target temperature 33°C/91.4°F) following cardiac arrest with return of spontaneous circulation. During the cooling phase, he develops shivering, which increases oxygen consumption and interferes with target temperature achievement. He is already on sedation and neuromuscular blockade is being considered. Evaluate the most appropriate management strategy considering both efficacy and safety.
- A. Administer meperidine alone to reduce shivering threshold
- B. Increase sedation and add surface counter-warming of extremities before neuromuscular blockade (Correct Answer)
- C. Abandon therapeutic hypothermia due to complications
- D. Use only mechanical restraints to prevent movement
- E. Immediate neuromuscular blockade without additional measures
Hypothermia pathophysiology Explanation: ***Increase sedation and add surface counter-warming of extremities before neuromuscular blockade***
- A **stepwise approach** to shivering is preferred; increasing **sedation** and using **surface counter-warming** reduces the shivering threshold by tricking the hypothalamus into sensing a warmer periphery.
- This strategy minimizes the need for **neuromuscular blockade**, which can mask seizures and prevent accurate **neurological assessment**.
*Administer meperidine alone to reduce shivering threshold*
- While **meperidine** is an effective anti-shivering agent that lowers the shivering threshold, using it **alone** is often insufficient to control vigorous shivering during induction.
- Reliance on a single pharmacologic agent ignores the **multimodal therapy** benefits of physical measures like skin warming and optimized sedation.
*Abandon therapeutic hypothermia due to complications*
- Shivering is a predictable physiological response, not a reason to abandon **Targeted Temperature Management (TTM)**, which provides significant **neuroprotection** post-cardiac arrest.
- Stopping the therapy would deprive the patient of the benefit of reduced **cerebral metabolic rate** and improved survival outcomes.
*Use only mechanical restraints to prevent movement*
- Mechanical restraints are ineffective against the **metabolic consequences** of shivering, such as increased **oxygen consumption** and CO2 production.
- Shivering is a thermoregulatory reflex, and physical restraint does not stop the underlying **thermogenesis** or metabolic demand.
*Immediate neuromuscular blockade without additional measures*
- **Neuromuscular blockade** should be a last resort as it carries risks of **prolonged muscle weakness** and obscures the patient's clinical neurological status.
- It treats the muscular manifestation but lacks the **sedative or analgesic** properties needed to comfort the patient during the cooling process.
More Hypothermia pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.