Hyperthermia vs fever US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hyperthermia vs fever. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hyperthermia vs fever US Medical PG Question 1: A 15-year-old boy is brought to the emergency department by his father 10 minutes after falling into a frozen lake during ice fishing. He was in the water for less than 1 minute before his father managed to pull him out. On arrival, his clothes are still wet and he appears scared. His body temperature is 36.2°C (97.1°F), pulse is 102/min, blood pressure is 133/88 mm Hg. Which of the following mechanisms contributes most to maintaining this patient's core body temperature?
- A. Inhibition of the thyroid axis
- B. Involuntary muscular contractions (Correct Answer)
- C. Activation of thermogenin
- D. Increase in hypothalamic set point
- E. Contraction of arrector pili muscles
Hyperthermia vs fever Explanation: ***Involuntary muscular contractions***
- **Shivering** is the body's primary mechanism for increasing heat production in response to cold stress, involving rapid, involuntary muscle contractions to generate heat.
- This process significantly increases the **metabolic rate** and heat output, crucial for maintaining core body temperature when exposed to cold environments.
*Inhibition of the thyroid axis*
- The **thyroid axis** is generally activated in response to chronic cold exposure to increase basal metabolic rate, not inhibited.
- Inhibition of thyroid hormones would lead to a decrease in metabolism and heat production, worsening hypothermia.
*Activation of thermogenin*
- **Thermogenin** (uncoupling protein 1) is found primarily in **brown adipose tissue** and its activation leads to non-shivering thermogenesis.
- While present in infants and some adults, shivering is a much more significant and rapid response to acute cold in a 15-year-old.
*Increase in hypothalamic set point*
- An increase in the **hypothalamic set point** is characteristic of **fever**, where the body aims to achieve a higher temperature.
- In this scenario, the body is trying to maintain its normal set point despite cold exposure, not raise it.
*Contraction of arrector pili muscles*
- **Contraction of arrector pili muscles** causes **piloerection** (goosebumps), which traps a layer of air close to the skin.
- While contributing to insulation, this mechanism is relatively minor in humans compared to the heat generated by shivering.
Hyperthermia vs fever US Medical PG Question 2: Two-hours into recovery from general anesthesia for an orthopedic fracture, a 34-year-old woman develops fever and masseter muscle rigidity with lockjaw. She has no history of a similar episode. She has no history of serious illness and takes no medications. She appears confused. In the recovery room, her blood pressure is 78/50 mm Hg, the pulse is 128/min, the respirations are 42/min, and the temperature is 40.3°C (104.5°F). Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Serum
Na+ 145 mEq/L
K+ 6.5 mEq/L
Arterial blood gas on room air
pH 7.01
PCO2 78 mm Hg
HCO3− 14 mEq/L
PO2 55 mm Hg
The patient is reintubated. Which of the following is the most appropriate next step in pharmacotherapy?
- A. Lorazepam
- B. Diphenhydramine
- C. Dantrolene (Correct Answer)
- D. Labetalol
- E. Cyproheptadine
Hyperthermia vs fever Explanation: ***Dantrolene***
- The patient exhibits classic signs of **malignant hyperthermia**, including
**masseter muscle rigidity**, **fever (40.3°C)**, **tachycardia (128/min)**,
**tachypnea (42/min)**, and **hypotension (78/50 mm Hg)**. The **elevated potassium (6.5
mEq/L)**, **acidosis (pH 7.01)**, and **hypercapnia (PCO2 78 mm Hg)**
further support this diagnosis.
- **Dantrolene** is the only specific antidote for malignant hyperthermia as
it acts as a **ryanodine receptor antagonist**, inhibiting calcium release
from the sarcoplasmic reticulum and thereby reducing muscle contracture and
heat production.
*Lorazepam*
- **Lorazepam** is a benzodiazepine used for treating seizures, anxiety, and
agitation, but it does **not address the underlying pathophysiology of
malignant hyperthermia**.
- While the patient appears confused, this is likely secondary to the
metabolic derangements and hyperthermia, not a primary indication for
lorazepam.
*Diphenhydramine*
- **Diphenhydramine** is an antihistamine used to treat allergic reactions or
sedation; it has no role in the management of malignant hyperthermia.
- It would not alleviate the muscle rigidity, hyperthermia, or metabolic
abnormalities seen in this patient.
*Labetalol*
- **Labetalol** is a beta-blocker used to manage hypertension and tachycardia,
but these are symptoms of malignant hyperthermia rather than the root
cause.
- While it could temporarily lower heart rate and blood pressure, it **does
not address the excessive calcium release** in skeletal muscle, which is
the hallmark of malignant hyperthermia.
*Cyproheptadine*
- **Cyproheptadine** is a serotonin antagonist used in the treatment of
serotonin syndrome.
- Malignant hyperthermia and serotonin syndrome share some clinical features
like hyperthermia, but the **trigger (anesthetic agents)** and underlying
mechanisms are different, making cyproheptadine ineffective here.
Hyperthermia vs fever US Medical PG Question 3: A group of investigators is studying thermoregulatory adaptations of the human body. A subject is seated in a thermally insulated isolation chamber with an internal temperature of 48°C (118°F), a pressure of 1 atmosphere, and a relative humidity of 10%. Which of the following is the primary mechanism of heat loss in this subject?
- A. Convection
- B. Evaporation (Correct Answer)
- C. Conduction
- D. Piloerection
- E. Radiation
Hyperthermia vs fever Explanation: ***Evaporation***
- In an environment where the ambient temperature (48°C) is **higher than body temperature**, heat gain by convection, conduction, and radiation occurs. Therefore, **evaporation** of sweat is the only significant mechanism for heat loss.
- The relatively low humidity (10%) at this high temperature facilitates efficient sweat **evaporation**, which cools the body as it converts liquid sweat into water vapor.
*Convection*
- **Convection** involves heat transfer through the movement of air or fluid over the body surface.
- Since the ambient temperature (48°C) is significantly **above body temperature**, the body would gain heat via convection, not lose it.
*Conduction*
- **Conduction** is direct heat transfer between objects in contact.
- As the ambient temperature (48°C) is much **higher than the skin temperature**, the body would actually **gain heat** through conduction from any surfaces it touched if they were at ambient temperature.
*Piloerection*
- **Piloerection** (goosebumps) is a mechanism for minimizing heat loss by trapping a layer of warm air close to the skin.
- This response is activated in **cold environments** to conserve heat, not in hot environments to dissipate it.
*Radiation*
- **Radiation** is heat transfer via electromagnetic waves without direct contact.
- Since the ambient temperature (48°C) is **higher than body surface temperature**, the body would **gain heat** by radiation, not lose it efficiently, from the surrounding environment.
Hyperthermia vs fever US Medical PG Question 4: A 23-year-old man presents to the emergency department brought in by police. He was found shouting at strangers in the middle of the street. The patient has no significant past medical history, and his only medications include a short course of prednisone recently prescribed for poison ivy exposure. His temperature is 77°F (25°C), blood pressure is 90/50 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. The patient is only wearing underwear, and he is occasionally mumbling angrily about the government. He appears to be responding to internal stimuli, and it is difficult to obtain a history from him. Which of the following is the next best step in management?
- A. Haloperidol IM
- B. Warmed IV normal saline and warm blankets (Correct Answer)
- C. Lorazepam and discontinue steroids
- D. Warm air recirculator
- E. Risperidone and warm blankets
Hyperthermia vs fever Explanation: ***Warmed IV normal saline and warm blankets***
- The patient's core body temperature of **77°F (25°C)** indicates severe **hypothermia**. The immediate priority is to rewarm the patient to prevent further physiological compromise.
- **Warmed IV normal saline** and **warm blankets** are essential interventions for **passive external rewarming** and **active core rewarming**, helping to gradually increase the patient's body temperature and stabilize hemodynamic status.
*Haloperidol IM*
- While the patient exhibits agitation and psychotic-like symptoms, addressing severe **hypothermia** is the immediate life-saving priority. Administering an antipsychotic without first stabilizing core temperature could be dangerous.
- Furthermore, **haloperidol** can have sedative effects that might mask the neurological signs of worsening hypothermia or other underlying conditions.
*Lorazepam and discontinue steroids*
- The patient's altered mental status and agitation are likely due to **hypothermia**, not necessarily an adverse effect of **prednisone** or an isolated psychiatric emergency requiring benzodiazepines.
- Discontinuing **steroids** abruptly can lead to **adrenal insufficiency**, which could further complicate the patient's critical condition, especially in the context of stress from severe hypothermia.
*Warm air recirculator*
- A **warm air recirculator** (e.g., forced-air warming blanket) is a form of **active external rewarming**. While beneficial, it is often used in conjunction with or after initiating **active core rewarming** with warmed IV fluids in cases of severe hypothermia.
- Relying solely on external rewarming might not be sufficient to rapidly correct **severe hypothermia** (core temperature < 28°C) and address associated **hemodynamic instability**.
*Risperidone and warm blankets*
- Similar to haloperidol, **risperidone** is an antipsychotic used for agitation and psychosis. However, the patient's primary and life-threatening issue is severe **hypothermia**.
- While **warm blankets** are appropriate for rewarming, addressing the underlying cause of the patient's presentation (hypothermia) takes precedence over immediate pharmacological management of psychiatric symptoms.
Hyperthermia vs fever US Medical PG Question 5: A 67-year-old man presents to the emergency department with confusion. The patient is generally healthy, but his wife noticed him becoming progressively more confused as the day went on. The patient is not currently taking any medications and has no recent falls or trauma. His temperature is 102°F (38.9°C), blood pressure is 126/64 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a confused man who cannot participate in a neurological exam secondary to his confusion. No symptoms are elicited with flexion of the neck and jolt accentuation of headache is negative. Initial laboratory values are unremarkable and the patient's chest radiograph and urinalysis are within normal limits. An initial CT scan of the head is unremarkable. Which of the following is the best next step in management?
- A. CT angiogram of the head and neck
- B. Vancomycin, ceftriaxone, ampicillin, and dexamethasone
- C. Acyclovir (Correct Answer)
- D. PCR of the cerebrospinal fluid
- E. MRI of the head
Hyperthermia vs fever Explanation: ***Acyclovir***
- This patient presents with **acute confusion and fever** without an obvious infectious source, negative meningeal signs, and normal initial imaging, highly suggestive of **herpes simplex encephalitis (HSE)**.
- HSE is a **medical emergency** with high mortality (70-80%) if untreated, but mortality drops to 20-30% with early acyclovir therapy.
- **Empiric acyclovir must be started immediately** upon clinical suspicion of HSE, **without waiting for diagnostic confirmation**.
- Standard management includes obtaining CSF for PCR **concurrently** with starting acyclovir, but treatment should never be delayed for diagnostic testing.
- The best next step in **management** is initiating acyclovir; CSF PCR is obtained for confirmation but does not delay treatment.
*PCR of the cerebrospinal fluid*
- **CSF PCR for HSV** is the gold standard **diagnostic test** for HSE with high sensitivity (96%) and specificity (99%).
- While lumbar puncture should be performed to obtain CSF for PCR, this is a **diagnostic step** that should be done **concurrently** with starting acyclovir, not instead of it.
- The question asks for best next step in **management**, not diagnosis—acyclovir therapy takes precedence.
- Delaying acyclovir while awaiting diagnostic confirmation significantly increases morbidity and mortality.
*Vancomycin, ceftriaxone, ampicillin, and dexamethasone*
- This broad-spectrum antibiotic regimen is empiric therapy for **bacterial meningitis** and should be considered in patients with fever and altered mental status.
- However, the **absence of meningeal signs** (negative nuchal rigidity, negative jolt accentuation) makes bacterial meningitis less likely.
- In practice, when HSE is suspected but bacterial meningitis cannot be excluded, both antimicrobial regimens may be initiated empirically, but the primary concern here is HSE given the clinical presentation.
*MRI of the head*
- **MRI with FLAIR sequences** is highly sensitive for HSE and typically shows **temporal lobe involvement** (especially medial temporal lobes).
- However, MRI findings may be **normal early in the disease course** (first 48-72 hours).
- MRI is useful for supporting the diagnosis but should **not delay empiric acyclovir therapy**.
- Obtaining MRI before treatment would be inappropriate given the time-sensitive nature of HSE.
*CT angiogram of the head and neck*
- CT angiography evaluates vascular structures and is indicated for suspected **stroke, aneurysm, or vascular dissection**.
- This patient lacks focal neurological deficits, signs of acute stroke, or vascular risk factors that would prioritize vascular imaging.
- The presentation with fever and diffuse encephalopathy points toward an infectious/inflammatory process rather than a vascular etiology.
Hyperthermia vs fever US Medical PG Question 6: A researcher is studying how arachidonic acid metabolites mediate the inflammatory response in rats. She has developed multiple enzyme inhibitors that specifically target individual proteins in the arachidonic acid pathway. She injects these inhibitors in rats who have been exposed to common bacterial pathogens and analyzes their downstream effects. In one of her experiments, she injects a leukotriene B4 inhibitor into a rat and observes an abnormal cell response. Which of the following interleukins would most closely restore the function of one of the missing products?
- A. Interleukin 2
- B. Interleukin 4
- C. Interleukin 1
- D. Interleukin 5
- E. Interleukin 8 (Correct Answer)
Hyperthermia vs fever Explanation: ***Interleukin 8***
- **Leukotriene B4 (LTB4)** is a potent **chemoattractant** and activator of neutrophils.
- **Interleukin 8 (IL-8)**, also known as **CXCL8**, is a primary **chemoattractant** for neutrophils, functionally mimicking the role of LTB4 in recruiting these inflammatory cells to the site of infection.
*Interleukin 2*
- **IL-2** is primarily involved in the **growth, proliferation, and differentiation of T cells**, as well as the activation of B cells and natural killer cells.
- It does not have a significant role in **neutrophil chemotaxis**, which is the main function of LTB4.
*Interleukin 4*
- **IL-4** is crucial for **B cell activation** and class switching to IgE, and it's a key cytokine in the **Th2 immune response**.
- Its functions are related to **allergic reactions** and **parasitic infections**, not neutrophil recruitment.
*Interleukin 1*
- **IL-1** is a pro-inflammatory cytokine that mediates a wide range of immune responses, including **fever** and the activation of other immune cells.
- While it contributes to inflammation, it does not directly act as a **chemoattractant for neutrophils** in the same manner as LTB4 or IL-8.
*Interleukin 5*
- **IL-5** is primarily involved in the **growth and differentiation of eosinophils** and B cell IgA production.
- It plays a significant role in **allergic reactions** and defense against parasites, not neutrophil chemotaxis.
Hyperthermia vs fever US Medical PG Question 7: A 42-year-old man undergoes therapeutic hypothermia (target temperature 33°C/91.4°F) following cardiac arrest with return of spontaneous circulation. During the cooling phase, he develops shivering, which increases oxygen consumption and interferes with target temperature achievement. He is already on sedation and neuromuscular blockade is being considered. Evaluate the most appropriate management strategy considering both efficacy and safety.
- A. Administer meperidine alone to reduce shivering threshold
- B. Increase sedation and add surface counter-warming of extremities before neuromuscular blockade (Correct Answer)
- C. Abandon therapeutic hypothermia due to complications
- D. Use only mechanical restraints to prevent movement
- E. Immediate neuromuscular blockade without additional measures
Hyperthermia vs fever Explanation: ***Increase sedation and add surface counter-warming of extremities before neuromuscular blockade***
- A **stepwise approach** to shivering is preferred; increasing **sedation** and using **surface counter-warming** reduces the shivering threshold by tricking the hypothalamus into sensing a warmer periphery.
- This strategy minimizes the need for **neuromuscular blockade**, which can mask seizures and prevent accurate **neurological assessment**.
*Administer meperidine alone to reduce shivering threshold*
- While **meperidine** is an effective anti-shivering agent that lowers the shivering threshold, using it **alone** is often insufficient to control vigorous shivering during induction.
- Reliance on a single pharmacologic agent ignores the **multimodal therapy** benefits of physical measures like skin warming and optimized sedation.
*Abandon therapeutic hypothermia due to complications*
- Shivering is a predictable physiological response, not a reason to abandon **Targeted Temperature Management (TTM)**, which provides significant **neuroprotection** post-cardiac arrest.
- Stopping the therapy would deprive the patient of the benefit of reduced **cerebral metabolic rate** and improved survival outcomes.
*Use only mechanical restraints to prevent movement*
- Mechanical restraints are ineffective against the **metabolic consequences** of shivering, such as increased **oxygen consumption** and CO2 production.
- Shivering is a thermoregulatory reflex, and physical restraint does not stop the underlying **thermogenesis** or metabolic demand.
*Immediate neuromuscular blockade without additional measures*
- **Neuromuscular blockade** should be a last resort as it carries risks of **prolonged muscle weakness** and obscures the patient's clinical neurological status.
- It treats the muscular manifestation but lacks the **sedative or analgesic** properties needed to comfort the patient during the cooling process.
Hyperthermia vs fever US Medical PG Question 8: A 72-year-old woman with end-stage renal disease on hemodialysis develops fever (103°F/39.4°C) with rigors during dialysis. Blood cultures from both the dialysis catheter and peripheral site grow gram-positive cocci. Despite appropriate antibiotics and catheter removal, she has persistent fevers of 101-102°F (38.3-38.9°C) for 7 days. She feels better and inflammatory markers are decreasing. Evaluate the most likely explanation for persistent fever.
- A. Appropriate lag in temperature resolution despite adequate treatment (Correct Answer)
- B. Undrained abscess requiring surgical intervention
- C. Drug fever from antibiotic therapy
- D. Inadequate dialysis causing uremic fever
- E. Antibiotic-resistant organism requiring regimen change
Hyperthermia vs fever Explanation: ***Appropriate lag in temperature resolution despite adequate treatment***
- In bacteremia, fever can persist for several days even with effective therapy because **inflammatory cytokines** (like IL-1 and TNF-α) and bacterial products take time to clear from the system.
- The clinical improvement and **decreasing inflammatory markers** (like CRP or ESR) are the most reliable indicators of a positive response to treatment, despite the slow normalization of the **hypothalamic set point**.
*Undrained abscess requiring surgical intervention*
- While a persistent fever can indicate an **occult abscess**, this is less likely when the patient reports feeling clinically better and lab trends are improving.
- Persistent bacteremia or clinical worsening, rather than just isolated fever, would typically necessitate intensive imaging for deep-seated **foci of infection**.
*Drug fever from antibiotic therapy*
- Drug fever is a diagnosis of exclusion that usually occurs after **7 to 10 days** of therapy and is often associated with a newly developed rash or eosinophilia.
- In this case, the patient's fever started with a known **bacterial source** (dialysis catheter), making an infectious resolution lag much more probable than a drug reaction.
*Inadequate dialysis causing uremic fever*
- **Uremia** is more commonly associated with **hypothermia** or a blunted febrile response rather than a high persistent fever.
- Modern dialysis efficiently prevents the build-up of metabolic toxins to levels that would trigger a high-grade **febrile state**.
*Antibiotic-resistant organism requiring regimen change*
- Resistance is unlikely here because the patient is showing **clinical improvement** and a downward trend in inflammatory markers, indicating the current regimen is effective.
- If a **resistant organism** were present, you would expect temperatures to remain very high or increase, and blood cultures to remain positive after 48-72 hours of therapy.
Hyperthermia vs fever US Medical PG Question 9: A 19-year-old man at a rave party is brought to the ED with agitation, temperature of 107°F (41.7°C), severe hypertension (180/110 mm Hg), tachycardia, dilated pupils, and diaphoresis. His friends report he took 'Molly.' Despite aggressive cooling, his temperature remains dangerously elevated and he develops rhabdomyolysis. Evaluate the most appropriate additional pharmacologic intervention.
- A. Bromocriptine as a dopamine agonist
- B. Benzodiazepines to reduce CNS and muscular hyperactivity (Correct Answer)
- C. Beta-blockers to control hypertension and tachycardia
- D. Antipyretics to reduce hypothalamic set point
- E. Dantrolene sodium to reduce muscle hypermetabolism
Hyperthermia vs fever Explanation: ***Benzodiazepines to reduce CNS and muscular hyperactivity***
- **MDMA (Ecstasy/Molly)** intoxication causes severe hyperthermia through increased **serotonergic activity**, muscle rigidity, and agitation; **benzodiazepines** are first-line to control agitation and reduce excessive muscle-generated heat.
- Administering **benzodiazepines** also helps manage secondary symptoms like **tachycardia** and **hypertension** by lowering sympathetic outflow.
*Bromocriptine as a dopamine agonist*
- **Bromocriptine** is specifically indicated for **Neuroleptic Malignant Syndrome (NMS)**, which involves dopamine depletion in the hypothalamus and basal ganglia.
- Using it in stimulant or serotonin-mediated toxicity is inappropriate and does not address the primary mechanism of **MDMA**-induced hyperthermia.
*Beta-blockers to control hypertension and tachycardia*
- **Beta-blockers** are generally avoided in stimulant toxicity due to the risk of **unopposed alpha-adrenergic stimulation**, which can worsen **hypertension** and coronary vasoconstriction.
- They do not address the lethal **hyperthermia** or muscle hyperactivity driven by the central nervous system.
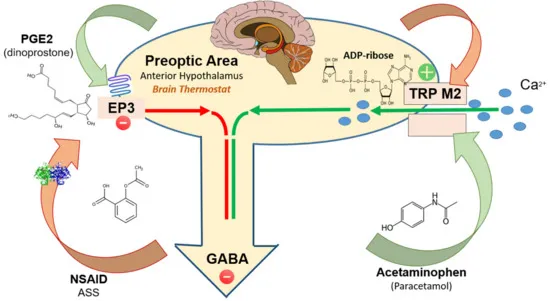
*Antipyretics to reduce hypothalamic set point*
- **Antipyretics** like aspirin or acetaminophen are ineffective because the high temperature in **MDMA** toxicity is caused by excess **thermogenesis** (muscle activity), not an altered **hypothalamic set point**.
- Relying on them delays more effective interventions like **evaporative cooling** and sedation.
*Dantrolene sodium to reduce muscle hypermetabolism*
- **Dantrolene** is the specific treatment for **Malignant Hyperthermia** (genetic ryanodine receptor defect) but has limited and controversial evidence in **serotonin syndrome** or MDMA toxicity.
- While it acts on muscle metabolism, **benzodiazepines** should be prioritized to treat the underlying **CNS-mediated agitation** and excessive movement.
Hyperthermia vs fever US Medical PG Question 10: A 55-year-old alcoholic man is admitted to the ICU with septic shock. Despite appropriate antibiotics and fluid resuscitation, he remains hypotensive. His core temperature is 95°F (35°C). Blood pressure improves only after active rewarming is initiated. Analyze the mechanism by which hypothermia contributed to his refractory hypotension.
- A. Decreased cardiac contractility and dysrhythmias from cold-induced membrane dysfunction (Correct Answer)
- B. Increased blood viscosity reducing cardiac output
- C. Impaired renal perfusion and fluid retention
- D. Peripheral vasodilation causing distributive shock
- E. Decreased catecholamine synthesis by adrenal glands
Hyperthermia vs fever Explanation: ***Decreased cardiac contractility and dysrhythmias from cold-induced membrane dysfunction***
- Hypothermia directly impairs **myocardial contractility** by affecting cell membrane ion channels and enzymatic reactions, leading to significantly reduced **cardiac output**.
- Cold temperatures induce **electrocardiographic changes** such as bradycardia and increased risk of **dysrhythmias**, making hypotension refractory to standard fluids and vasopressors until rewarming occurs.
*Increased blood viscosity reducing cardiac output*
- While hypothermia does increase **blood viscosity** (the "sludging" effect), this primarily leads to **microcirculatory impairment** rather than global refractory hypotension in acute shock.
- The hemodynamic instability in sepsis combined with hypothermia is more significantly driven by **myocardial depression** than by changes in blood rheology.
*Impaired renal perfusion and fluid retention*
- Hypothermia typically causes **cold diuresis** due to inhibited antidiuretic hormone (ADH) and increased tubular pressure, which would lead to fluid loss rather than retention.
- While **renal perfusion** may eventually decrease due to low cardiac output, this mechanism does not explain why blood pressure is refractory to resuscitation during the hypothermic state.
*Peripheral vasodilation causing distributive shock*
- Early hypothermia actually causes **peripheral vasoconstriction** as a compensatory mechanism to preserve core heat, which is the opposite of vasodilation.
- Although **distributive shock** is present due to sepsis, the hypothermia-induced component of hypotension is specifically related to **cardiovascular depression**, not additional vasodilation.
*Decreased catecholamine synthesis by adrenal glands*
- Hypothermia leads to a decreased **responsiveness** to catecholamines (both endogenous and exogenous) rather than a primary failure of their synthesis.
- The enzymatic slowing and **metabolic depression** caused by cold temperatures prevent target organs from reacting appropriately to the **adrenaline and noradrenaline** already present in the system.
More Hyperthermia vs fever US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.