Heat production mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Heat production mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Heat production mechanisms US Medical PG Question 1: An investigator is studying a hereditary defect in the mitochondrial enzyme succinyl-CoA synthetase. In addition to succinate, the reaction catalyzed by this enzyme produces a molecule that is utilized as an energy source for protein translation. This molecule is also required for which of the following conversion reactions?
- A. Oxaloacetate to phosphoenolpyruvate (Correct Answer)
- B. Pyruvate to acetyl-CoA
- C. Acetaldehyde to acetate
- D. Glucose-6-phosphate to 6-phosphogluconolactone
- E. Fructose-6-phosphate to fructose-1,6-bisphosphate
Heat production mechanisms Explanation: ***Oxaloacetate to phosphoenolpyruvate***
- The reaction catalyzed by **succinyl-CoA synthetase** (also known as succinate thiokinase) produces **GTP** (guanosine triphosphate) from GDP and Pi, in addition to succinate.
- **GTP** is required for the conversion of **oxaloacetate** to **phosphoenolpyruvate** in gluconeogenesis, catalyzed by **PEP carboxykinase**.
*Pyruvate to acetyl-CoA*
- This reaction is catalyzed by the **pyruvate dehydrogenase complex** and produces NADH, not GTP.
- It is an irreversible step linking glycolysis to the citric acid cycle.
*Acetaldehyde to acetate*
- This reaction is catalyzed by **aldehyde dehydrogenase** and uses **NAD+** as a cofactor, producing NADH.
- It is involved in alcohol metabolism.
*Glucose-6-phosphate to 6-phosphogluconolactone*
- This is the first committed step of the **pentose phosphate pathway**, catalyzed by **glucose-6-phosphate dehydrogenase**.
- It uses **NADP+** as a cofactor, producing NADPH.
*Fructose-6-phosphate to fructose-1,6-bisphosphate*
- This reaction is a key regulatory step in **glycolysis**, catalyzed by **phosphofructokinase-1 (PFK-1)**.
- It consumes **ATP**, rather than producing GTP or utilizing it as a cofactor in the context of this question.
Heat production mechanisms US Medical PG Question 2: A 20-year-old woman reports to student health complaining of 5 days of viral symptoms including sneezing and a runny nose. She started coughing 2 days ago and is seeking cough medication. She additionally mentions that she developed a fever 2 days ago, but this has resolved. On exam, her temperature is 99.0°F (37.2°C), blood pressure is 118/76 mmHg, pulse is 86/min, and respirations are 12/min. Changes in the activity of warm-sensitive neurons in which part of her hypothalamus likely contributed to the development and resolution of her fever?
- A. Anterior hypothalamus (Correct Answer)
- B. Paraventricular nucleus
- C. Suprachiasmatic nucleus
- D. Lateral area
- E. Posterior hypothalamus
Heat production mechanisms Explanation: ***Anterior hypothalamus***
- The **anterior hypothalamus** contains warm-sensitive neurons that detect increases in body temperature and activate mechanisms for heat dissipation, such as sweating and vasodilation.
- In fever, **prostaglandins** increase the set point in the anterior hypothalamus, causing the body to retain heat and increase heat production until the new set point is reached; resolution of fever involves resetting this set point back to normal.
*Paraventricular nucleus*
- The **paraventricular nucleus** is primarily involved in neuroendocrine functions, stress response, and the regulation of appetite and autonomic nervous system.
- It plays a significant role in releasing hormones like **corticotropin-releasing hormone (CRH)** and **oxytocin**, not direct temperature regulation.
*Suprachiasmatic nucleus*
- The **suprachiasmatic nucleus (SCN)** is the body's main biological clock, regulating **circadian rhythms** including the sleep-wake cycle and daily fluctuations in body temperature.
- While it influences the normal diurnal variation in body temperature, it is not directly responsible for the acute regulation of fever.
*Lateral area*
- The **lateral hypothalamus** primarily functions as the "hunger center," stimulating foraging and feeding behavior.
- Damage to this area can lead to **anorexia** and reduced food intake, not impairments in fever response.
*Posterior hypothalamus*
- The **posterior hypothalamus** is primarily involved in heat conservation and production mechanisms, such as shivering and vasoconstriction, in response to cold.
- It contains cold-sensitive neurons and functions to raise body temperature if it falls below the set point, but it is not where the set point itself is regulated in response to pyrogens.
Heat production mechanisms US Medical PG Question 3: A 26-year-old medical student who is preparing for Step 1 exams is woken up by her friend for breakfast. She realizes that she must have fallen asleep at her desk while attempting to study through the night. While walking with her friend to breakfast, she realizes that she has not eaten since breakfast the previous day. Using this as motivation to review some biochemistry, she pauses to consider what organs are responsible for allowing her to continue thinking clearly in this physiologic state. Which of the following sets of organs are associated with the major source of energy currently facilitating her cognition?
- A. Muscle only
- B. Liver and kidney (Correct Answer)
- C. Liver and muscle
- D. Liver, muscle, and kidney
- E. Liver only
Heat production mechanisms Explanation: ***Liver and kidney***
- After an overnight fast (~16-24 hours without food), the **liver** is the **primary organ** responsible for maintaining blood glucose levels through **glycogenolysis** (initially) and **gluconeogenesis** (predominantly at this stage).
- The **kidney** also contributes to **gluconeogenesis** even during an overnight fast, providing approximately **10-15% of total glucose production**. While this contribution is relatively minor compared to the liver, it becomes increasingly important during more prolonged fasting states (>48-72 hours), where it can account for up to 40% of glucose production.
- Since the brain relies almost exclusively on glucose at this stage of fasting (ketone bodies are not yet a major fuel source), both organs that produce glucose for systemic use are correctly identified here.
*Muscle only*
- Muscle glycogen can only be used by the **muscle cells themselves** due to the absence of **glucose-6-phosphatase**, so muscle cannot release free glucose into the bloodstream for use by the brain.
- While muscle does provide amino acids (particularly alanine and glutamine) for gluconeogenesis in the liver and kidney, it does not directly supply glucose to support brain function.
*Liver and muscle*
- As explained above, muscle cannot directly supply glucose to the bloodstream to support brain function due to the lack of **glucose-6-phosphatase**.
- The liver is a major contributor, but muscle is not a direct source of blood glucose.
*Liver, muscle, and kidney*
- This option incorrectly includes muscle as a direct source of glucose for the brain. While liver and kidney both perform gluconeogenesis and release glucose into the bloodstream, muscle lacks this capability.
*Liver only*
- While the liver is indeed the **dominant source** of glucose during an overnight fast (contributing ~85-90% of gluconeogenesis), the **kidney also actively participates** in glucose production, contributing ~10-15% at this stage.
- Since the question asks which organs are "responsible" for maintaining cognition, and both organs contribute to systemic glucose production (even if disproportionately), "liver only" is incomplete.
- The kidney's contribution, though relatively minor during overnight fasting, becomes more substantial during prolonged fasting states.
Heat production mechanisms US Medical PG Question 4: A 2-month-old boy is presented to the clinic for a well-child visit by his parents. They are concerned with his weak cry and difficulty with feeding. Birth history reveals that the boy was born at the 37th week of gestation by cesarean section due to poor fetal movement and fetal distress. His Apgar scores were 3 and 5 at 1st and 5th minute respectively and his birth weight was 2.5 kg (6 lb). His vital signs include heart rate 120/min, respiratory rate 40/min, blood pressure 90/50 mm Hg, and temperature 37.0°C (98.6°F). Physical examination reveals a malnourished boy with a small narrow forehead and a small jaw. His mouth is small and he has comparatively small genitals. He has a poor muscle tone. After repeated follow-up, he gains weight rapidly but his height fails to increase. Developmental milestones are delayed at the age of 3 years. Genetic testing reveals Prader-Willi syndrome. Which of the following is the most common mechanism for the development of this patient’s condition?
- A. Anticipation
- B. Heteroplasmy
- C. Incomplete penetrance
- D. Maternal uniparental disomy
- E. Paternal deletion of 15q11-q13 (Correct Answer)
Heat production mechanisms Explanation: ***Paternal deletion of 15q11-q13***
- This is the **most common genetic mechanism** (occurring in about 70-75% of cases) for Prader-Willi syndrome, involving the loss of genetic material from the paternally inherited chromosome 15 in the specified region
- The deletion affects genes that are **normally expressed only from the paternal chromosome** due to genomic imprinting, leading to the characteristic features of hypotonia, feeding difficulties in infancy, subsequent hyperphagia with obesity, hypogonadism, and developmental delays
*Incorrect: Anticipation*
- Anticipation describes a genetic phenomenon where a disorder appears earlier or symptoms become more severe with each successive generation
- This is typically seen in disorders caused by expanding **trinucleotide repeats** (e.g., Huntington's disease, myotonic dystrophy), not applicable to Prader-Willi syndrome
*Incorrect: Heteroplasmy*
- Heteroplasmy refers to the presence of more than one type of mitochondrial DNA within a cell or individual
- This concept is relevant to **mitochondrial genetic disorders** which are maternally inherited, not to Prader-Willi syndrome which is a nuclear chromosomal imprinting disorder
*Incorrect: Incomplete penetrance*
- Incomplete penetrance occurs when individuals carrying a pathogenic mutation do not express the associated clinical phenotype
- Prader-Willi syndrome typically presents with a **consistent set of features** when the genetic defect is present; incomplete penetrance is not the mechanism of disease development
*Incorrect: Maternal uniparental disomy*
- Maternal uniparental disomy (UPD) of chromosome 15 is the **second most common mechanism** for Prader-Willi syndrome (occurring in about 20-25% of cases)
- This involves inheriting **both copies of chromosome 15 from the mother** and none from the father, leading to absence of paternal gene expression in the critical 15q11-q13 region
- While less common than paternal deletion, this is still a significant cause of the syndrome
Heat production mechanisms US Medical PG Question 5: You have been asked to deliver a lecture to medical students about the effects of various body hormones and neurotransmitters on the metabolism of glucose. Which of the following statements best describes the effects of sympathetic stimulation on glucose metabolism?
- A. Norepinephrine causes increased glucose absorption within the intestines.
- B. Without epinephrine, insulin cannot act on the liver.
- C. Peripheral tissues require epinephrine to take up glucose.
- D. Epinephrine increases liver glycogenolysis. (Correct Answer)
- E. Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.
Heat production mechanisms Explanation: ***Epinephrine increases liver glycogenolysis.***
- **Epinephrine**, released during sympathetic stimulation, primarily acts to increase **glucose availability** for immediate energy.
- It achieves this by stimulating **glycogenolysis** (breakdown of glycogen into glucose) in the liver via **beta-adrenergic receptors**.
*Norepinephrine causes increased glucose absorption within the intestines.*
- **Norepinephrine** primarily causes **vasoconstriction** and can *decrease* **intestinal motility** and nutrient absorption due to shunting blood away from the digestive tract during stress.
- Glucose absorption is mainly regulated by digestive enzymes and transport proteins, not directly increased by norepinephrine.
*Without epinephrine, insulin cannot act on the liver.*
- **Insulin** acts on the liver independent of epinephrine to promote **glucose uptake**, **glycogenesis**, and **lipid synthesis**.
- Epinephrine and insulin have **antagonistic effects** on liver glucose metabolism; epinephrine increases glucose output, while insulin decreases it.
*Peripheral tissues require epinephrine to take up glucose.*
- **Insulin** is the primary hormone required for **glucose uptake** by most peripheral tissues, especially **muscle** and **adipose tissue**, via **GLUT4 transporters**.
- Epinephrine generally *reduces* glucose uptake by peripheral tissues to preserve glucose for the brain during stress.
*Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.*
- Sympathetic stimulation, primarily acting through **alpha-2 adrenergic receptors** on pancreatic beta cells, actually **inhibits** **insulin secretion**.
- This inhibition helps to increase blood glucose levels by reducing insulin's glucose-lowering effects.
Heat production mechanisms US Medical PG Question 6: An investigator is studying muscle contraction in tissue obtained from the thigh muscle of an experimental animal. After injection of radiolabeled ATP, the tissue is stimulated with electrical impulses. Radioassay of these muscle cells is most likely to show greatest activity in which of the following structures?
- A. H zone
- B. M line
- C. A band (Correct Answer)
- D. Z line
- E. I band
Heat production mechanisms Explanation: ***A band***
- The **A band** contains the entire length of the **thick myosin filaments** along with the **overlap zone** where myosin and actin interact. Myosin has **ATPase activity**, meaning it binds and hydrolyzes **ATP** to power muscle contraction through cross-bridge cycling.
- Therefore, the greatest accumulation of **radiolabeled ATP** and its breakdown products would be found where **myosin heads** are located throughout the A band.
- The A band represents the most complete answer as it encompasses all regions containing myosin ATPase activity.
*H zone*
- The **H zone** is the central part of the **A band** where only **thick myosin filaments** are present, with no overlap with thin actin filaments.
- While myosin heads with ATPase activity are present here and would show radiolabeled ATP, the **H zone** is only a **subset** of the A band. The **A band** is the more comprehensive answer as it includes both the H zone and the overlap regions where most cross-bridge cycling occurs.
*M line*
- The **M line** is the very center of the **H zone** and anchors the **thick filaments**.
- It consists of structural proteins like **myomesin** and **creatine kinase**. While creatine kinase can phosphorylate ADP to regenerate ATP, it does not directly hydrolyze ATP for muscle contraction the way myosin ATPase does.
*Z line*
- The **Z line** (or Z disc) marks the boundaries of a **sarcomere** and anchors the **thin actin filaments**.
- It contains proteins like **alpha-actinin** and **desmin** but does not directly consume ATP for muscle contraction.
*I band*
- The **I band** contains only **thin actin filaments** and extends from the edge of the A band to the Z line.
- While actin is crucial for contraction, it does not possess **ATPase activity**; ATP hydrolysis primarily occurs at the **myosin heads** located in the A band.
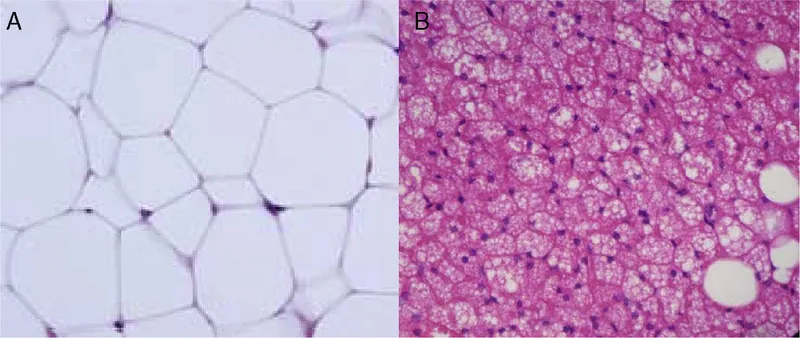
Heat production mechanisms US Medical PG Question 7: An investigator is conducting a study on hematological factors that affect the affinity of hemoglobin for oxygen. An illustration of two graphs (A and B) that represent the affinity of hemoglobin for oxygen is shown. Which of the following best explains a shift from A to B?
- A. Decreased serum pCO2
- B. Increased serum pH
- C. Decreased serum 2,3-bisphosphoglycerate concentration
- D. Increased body temperature (Correct Answer)
- E. Increased hemoglobin γ-chain synthesis
Heat production mechanisms Explanation: ***Increased body temperature***
- A shift from A to B represents a **rightward shift** of the oxygen-hemoglobin dissociation curve, indicating **decreased hemoglobin affinity for oxygen**.
- **Increased body temperature** (e.g., during exercise, fever) reduces hemoglobin's affinity for oxygen, facilitating **oxygen release to tissues**.
*Decreased serum pCO2*
- A **decrease in serum pCO2** leads to an **increase in pH** (alkalosis) and a **leftward shift** of the curve, meaning an increased affinity of hemoglobin for oxygen.
- This is part of the **Bohr effect**, where lower CO2 levels signal decreased tissue metabolic activity, thus reducing oxygen unloading.
*Increased serum pH*
- An **increase in serum pH** (alkalosis) causes a **leftward shift** of the oxygen-hemoglobin dissociation curve, signifying **increased hemoglobin affinity for oxygen**.
- This response is beneficial in the lungs, where higher pH promotes oxygen binding to hemoglobin.
*Decreased serum 2,3-bisphosphoglycerate concentration*
- A **decrease in 2,3-BPG** concentration leads to a **leftward shift** of the curve, representing **increased hemoglobin affinity for oxygen**.
- 2,3-BPG typically binds to deoxyhemoglobin, stabilizing its T-state and promoting oxygen release; thus, less 2,3-BPG means less release.
*Increased hemoglobin γ-chain synthesis*
- Increased **hemoglobin γ-chain synthesis** is characteristic of **fetal hemoglobin (HbF)**, which has a **higher affinity for oxygen** than adult hemoglobin (HbA).
- This would result in a **leftward shift** of the oxygen-hemoglobin dissociation curve, enhancing oxygen uptake by the fetus.
Heat production mechanisms US Medical PG Question 8: A 42-year-old man undergoes therapeutic hypothermia (target temperature 33°C/91.4°F) following cardiac arrest with return of spontaneous circulation. During the cooling phase, he develops shivering, which increases oxygen consumption and interferes with target temperature achievement. He is already on sedation and neuromuscular blockade is being considered. Evaluate the most appropriate management strategy considering both efficacy and safety.
- A. Administer meperidine alone to reduce shivering threshold
- B. Increase sedation and add surface counter-warming of extremities before neuromuscular blockade (Correct Answer)
- C. Abandon therapeutic hypothermia due to complications
- D. Use only mechanical restraints to prevent movement
- E. Immediate neuromuscular blockade without additional measures
Heat production mechanisms Explanation: ***Increase sedation and add surface counter-warming of extremities before neuromuscular blockade***
- A **stepwise approach** to shivering is preferred; increasing **sedation** and using **surface counter-warming** reduces the shivering threshold by tricking the hypothalamus into sensing a warmer periphery.
- This strategy minimizes the need for **neuromuscular blockade**, which can mask seizures and prevent accurate **neurological assessment**.
*Administer meperidine alone to reduce shivering threshold*
- While **meperidine** is an effective anti-shivering agent that lowers the shivering threshold, using it **alone** is often insufficient to control vigorous shivering during induction.
- Reliance on a single pharmacologic agent ignores the **multimodal therapy** benefits of physical measures like skin warming and optimized sedation.
*Abandon therapeutic hypothermia due to complications*
- Shivering is a predictable physiological response, not a reason to abandon **Targeted Temperature Management (TTM)**, which provides significant **neuroprotection** post-cardiac arrest.
- Stopping the therapy would deprive the patient of the benefit of reduced **cerebral metabolic rate** and improved survival outcomes.
*Use only mechanical restraints to prevent movement*
- Mechanical restraints are ineffective against the **metabolic consequences** of shivering, such as increased **oxygen consumption** and CO2 production.
- Shivering is a thermoregulatory reflex, and physical restraint does not stop the underlying **thermogenesis** or metabolic demand.
*Immediate neuromuscular blockade without additional measures*
- **Neuromuscular blockade** should be a last resort as it carries risks of **prolonged muscle weakness** and obscures the patient's clinical neurological status.
- It treats the muscular manifestation but lacks the **sedative or analgesic** properties needed to comfort the patient during the cooling process.
Heat production mechanisms US Medical PG Question 9: A 72-year-old woman with end-stage renal disease on hemodialysis develops fever (103°F/39.4°C) with rigors during dialysis. Blood cultures from both the dialysis catheter and peripheral site grow gram-positive cocci. Despite appropriate antibiotics and catheter removal, she has persistent fevers of 101-102°F (38.3-38.9°C) for 7 days. She feels better and inflammatory markers are decreasing. Evaluate the most likely explanation for persistent fever.
- A. Appropriate lag in temperature resolution despite adequate treatment (Correct Answer)
- B. Undrained abscess requiring surgical intervention
- C. Drug fever from antibiotic therapy
- D. Inadequate dialysis causing uremic fever
- E. Antibiotic-resistant organism requiring regimen change
Heat production mechanisms Explanation: ***Appropriate lag in temperature resolution despite adequate treatment***
- In bacteremia, fever can persist for several days even with effective therapy because **inflammatory cytokines** (like IL-1 and TNF-α) and bacterial products take time to clear from the system.
- The clinical improvement and **decreasing inflammatory markers** (like CRP or ESR) are the most reliable indicators of a positive response to treatment, despite the slow normalization of the **hypothalamic set point**.
*Undrained abscess requiring surgical intervention*
- While a persistent fever can indicate an **occult abscess**, this is less likely when the patient reports feeling clinically better and lab trends are improving.
- Persistent bacteremia or clinical worsening, rather than just isolated fever, would typically necessitate intensive imaging for deep-seated **foci of infection**.
*Drug fever from antibiotic therapy*
- Drug fever is a diagnosis of exclusion that usually occurs after **7 to 10 days** of therapy and is often associated with a newly developed rash or eosinophilia.
- In this case, the patient's fever started with a known **bacterial source** (dialysis catheter), making an infectious resolution lag much more probable than a drug reaction.
*Inadequate dialysis causing uremic fever*
- **Uremia** is more commonly associated with **hypothermia** or a blunted febrile response rather than a high persistent fever.
- Modern dialysis efficiently prevents the build-up of metabolic toxins to levels that would trigger a high-grade **febrile state**.
*Antibiotic-resistant organism requiring regimen change*
- Resistance is unlikely here because the patient is showing **clinical improvement** and a downward trend in inflammatory markers, indicating the current regimen is effective.
- If a **resistant organism** were present, you would expect temperatures to remain very high or increase, and blood cultures to remain positive after 48-72 hours of therapy.
Heat production mechanisms US Medical PG Question 10: A 19-year-old man at a rave party is brought to the ED with agitation, temperature of 107°F (41.7°C), severe hypertension (180/110 mm Hg), tachycardia, dilated pupils, and diaphoresis. His friends report he took 'Molly.' Despite aggressive cooling, his temperature remains dangerously elevated and he develops rhabdomyolysis. Evaluate the most appropriate additional pharmacologic intervention.
- A. Bromocriptine as a dopamine agonist
- B. Benzodiazepines to reduce CNS and muscular hyperactivity (Correct Answer)
- C. Beta-blockers to control hypertension and tachycardia
- D. Antipyretics to reduce hypothalamic set point
- E. Dantrolene sodium to reduce muscle hypermetabolism
Heat production mechanisms Explanation: ***Benzodiazepines to reduce CNS and muscular hyperactivity***
- **MDMA (Ecstasy/Molly)** intoxication causes severe hyperthermia through increased **serotonergic activity**, muscle rigidity, and agitation; **benzodiazepines** are first-line to control agitation and reduce excessive muscle-generated heat.
- Administering **benzodiazepines** also helps manage secondary symptoms like **tachycardia** and **hypertension** by lowering sympathetic outflow.
*Bromocriptine as a dopamine agonist*
- **Bromocriptine** is specifically indicated for **Neuroleptic Malignant Syndrome (NMS)**, which involves dopamine depletion in the hypothalamus and basal ganglia.
- Using it in stimulant or serotonin-mediated toxicity is inappropriate and does not address the primary mechanism of **MDMA**-induced hyperthermia.
*Beta-blockers to control hypertension and tachycardia*
- **Beta-blockers** are generally avoided in stimulant toxicity due to the risk of **unopposed alpha-adrenergic stimulation**, which can worsen **hypertension** and coronary vasoconstriction.
- They do not address the lethal **hyperthermia** or muscle hyperactivity driven by the central nervous system.
*Antipyretics to reduce hypothalamic set point*
- **Antipyretics** like aspirin or acetaminophen are ineffective because the high temperature in **MDMA** toxicity is caused by excess **thermogenesis** (muscle activity), not an altered **hypothalamic set point**.
- Relying on them delays more effective interventions like **evaporative cooling** and sedation.
*Dantrolene sodium to reduce muscle hypermetabolism*
- **Dantrolene** is the specific treatment for **Malignant Hyperthermia** (genetic ryanodine receptor defect) but has limited and controversial evidence in **serotonin syndrome** or MDMA toxicity.
- While it acts on muscle metabolism, **benzodiazepines** should be prioritized to treat the underlying **CNS-mediated agitation** and excessive movement.
More Heat production mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.