Fever patterns and significance US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fever patterns and significance. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fever patterns and significance US Medical PG Question 1: A 15-year-old girl comes to the physician because of a sore throat and subjective fevers for the past 2 weeks. She has been feeling lethargic and is unable to attend school. She has a history of multiple episodes of streptococcal pharyngitis treated with amoxicillin. She immigrated with her family to the United States from China 10 years ago. She appears thin. Her temperature is 37.8°C (100°F), pulse is 97/min, and blood pressure is 90/60 mm Hg. Examination shows pharyngeal erythema and enlarged tonsils with exudates and palatal petechiae. There is cervical lymphadenopathy. The spleen is palpated 2 cm below the left costal margin. Her hemoglobin concentration is 12 g/dL, leukocyte count is 14,100/mm3 with 54% lymphocytes (12% atypical lymphocytes), and platelet count is 280,000/mm3. A heterophile agglutination test is positive. The underlying cause of this patient's symptoms is most likely to increase the risk of which of the following conditions?
- A. Kaposi sarcoma
- B. Glomerulonephritis
- C. Pneumonia
- D. Nasopharyngeal carcinoma (Correct Answer)
- E. Necrotizing retinitis
Fever patterns and significance Explanation: ***Nasopharyngeal carcinoma***
- The patient's symptoms (sore throat, fatigue, pharyngeal erythema, enlarged tonsils with exudates, palatal petechiae, cervical lymphadenopathy, splenomegaly, atypical lymphocytosis, and positive heterophile agglutination test) are classic for **infectious mononucleosis**, caused by the **Epstein-Barr virus (EBV)**.
- EBV infection is a significant risk factor for developing **nasopharyngeal carcinoma**, especially in individuals of Chinese descent, making this the most likely long-term complication.
*Kaposi sarcoma*
- **Kaposi sarcoma** is associated with **human herpesvirus 8 (HHV-8)**, not EBV.
- It is typically seen in immunocompromised individuals, such as those with HIV/AIDS, or in specific endemic regions.
*Glomerulonephritis*
- **Glomerulonephritis** can be a complication of **Streptococcus pyogenes infections** (post-streptococcal glomerulonephritis) or other autoimmune diseases, but it is not directly linked to EBV infection.
- The patient's history of streptococcal pharyngitis is relevant for this, but her current presentation points to EBV.
*Pneumonia*
- While pneumonia can occur as a secondary complication in severely ill patients with infectious mononucleosis, it is not a direct long-term increased risk associated with the underlying EBV infection itself.
- EBV primarily affects lymphoid tissues.
*Necrotizing retinitis*
- **Necrotizing retinitis** is most commonly associated with **cytomegalovirus (CMV)** infection, particularly in immunocompromised patients (e.g., HIV/AIDS).
- It is not a typical complication or long-term risk of EBV infection.
Fever patterns and significance US Medical PG Question 2: A 23-year-old woman presents with progressively worsening headache, photophobia, and intermittent fever that have lasted for 6 days. She says her headache is mostly frontal and radiates down her neck. She denies any recent history of blood transfusions, recent travel, or contact with animals. Her past medical history is unremarkable. She is sexually active with a single partner for the past 3 years. Her temperature is 38.5°C (101.3°F). On physical examination, she appears pale and diaphoretic. A fine erythematous rash is noted on the neck and forearms. A lumbar puncture is performed and CSF analysis reveals:
Opening pressure: 300 mm H2O
Erythrocytes: None
Leukocytes: 72/mm3
Neutrophils: 10%
Lymphocytes: 75%
Mononuclear: 15%
Protein: 100 mg/dL
Glucose: 70 mg/dL
Which of the following is the most likely diagnosis in this patient?
- A. Lymphocytic choriomeningitis virus
- B. Ehrlichiosis
- C. Enterovirus meningitis (Correct Answer)
- D. Brucellosis
- E. Mumps meningitis
Fever patterns and significance Explanation: ***Enterovirus meningitis***
- The patient's symptoms of **headache**, **photophobia**, **fever**, and a **fine erythematous rash**, combined with CSF findings of **lymphocytic pleocytosis (75%)**, **elevated protein**, and **normal glucose**, are classic for **viral (aseptic) meningitis**.
- Enteroviruses (including coxsackievirus and echovirus) are the **most common cause** of viral meningitis in immunocompetent adults, particularly in summer and fall.
- The **normal glucose level** (70 mg/dL) effectively rules out bacterial meningitis, while the **lymphocytic predominance** with mildly elevated protein is pathognomonic for viral etiology.
- The fine erythematous rash is consistent with enteroviral exanthem.
*Lymphocytic choriomeningitis virus*
- While LCMV can cause aseptic meningitis with similar CSF findings (lymphocytic pleocytosis, normal glucose), it is typically acquired through contact with **rodent urine or feces**, particularly from pet hamsters or mice.
- The patient **denies animal contact**, making this diagnosis less likely than the more prevalent enterovirus infection.
*Ehrlichiosis*
- Ehrlichiosis is a **tick-borne illness** (from *Ehrlichia* species) that can cause fever, headache, and rash, but typically presents with **leukopenia**, **thrombocytopenia**, and elevated liver enzymes.
- The rash in ehrlichiosis is often petechial or absent entirely. CNS involvement is uncommon and would more likely present as meningoencephalitis rather than isolated meningitis.
- The CSF profile with prominent lymphocytic pleocytosis and normal glucose fits viral meningitis better than ehrlichiosis.
*Brucellosis*
- Brucellosis is a **zoonotic infection** acquired through contact with **unpasteurized dairy products** or infected livestock (cattle, goats, pigs), which the patient denies.
- While *Brucella* can cause chronic meningitis with lymphocytic pleocytosis, it classically presents with **undulating fever**, hepatosplenomegaly, and a more protracted course (weeks to months).
- The acute 6-day presentation without exposure history makes this unlikely.
*Mumps meningitis*
- Mumps virus can cause aseptic meningitis with a similar CSF profile (lymphocytic pleocytosis, normal glucose).
- However, mumps meningitis typically occurs in association with or following **parotitis (parotid gland swelling)**, which is not mentioned in this case.
- With widespread MMR vaccination, mumps is now rare in immunized populations, making enterovirus a more likely diagnosis.
Fever patterns and significance US Medical PG Question 3: A 25-year-old man presents to the emergency department after a motor vehicle accident. He was the unrestrained front seat driver in a head on collision. The patient is unresponsive and his medical history is unknown. His temperature is 99.5°F (37.5°C), blood pressure is 67/38 mmHg, pulse is 190/min, respirations are 33/min, and oxygen saturation is 98% on room air. The patient is started on IV fluids, blood products, and norepinephrine. A FAST exam is performed and a pelvic binder is placed. One hour later, his temperature is 98.3°F (36.8°C), blood pressure is 119/66 mmHg, pulse is 110/min, respirations are 15/min, and oxygen saturation is 97% on room air. The patient is currently responsive. Management of the patient's pelvic fracture is scheduled by the orthopedic service. While the patient is waiting in the emergency department he suddenly complains of feeling hot, aches, and a headache. The patient's temperature is currently 101°F (38.3°C). He has not been given any pain medications and his past medical history is still unknown. Which of the following is the most likely diagnosis?
- A. Acute hemolytic transfusion reaction
- B. Febrile non-hemolytic transfusion reaction (Correct Answer)
- C. Sympathetic response to pain
- D. Minor blood group incompatibility
- E. Leukoagglutination reaction
Fever patterns and significance Explanation: ***Febrile non-hemolytic transfusion reaction***
- This reaction is characterized by a **fever** and other constitutional symptoms (chills, headache, malaise) developing **within 4 hours of transfusion**, without evidence of hemolysis. The patient's symptoms and temperature rise after blood product administration fit this description.
- It is typically caused by antibodies in the recipient's plasma reacting with **leukocyte antigens** present on donor white blood cells or by **cytokines** released from donor leukocytes during storage.
*Acute hemolytic transfusion reaction*
- This reaction typically presents with more severe symptoms such as **hypotension**, **hemoglobinuria**, flank pain, and diffuse bleeding, indicating widespread intravascular hemolysis due to **ABO incompatibility**.
- Although the patient received blood products, his symptoms (feeling hot, aches, headache, mild fever) are not indicative of the severe, life-threatening nature of an acute hemolytic reaction.
*Sympathetic response to pain*
- While pain can cause a sympathetic response (tachycardia, hypertension), it typically does **not cause a fever** as seen in this patient.
- The patient's initial presentation included signs of shock, and after resuscitation, his vital signs normalized before the new symptoms appeared, suggesting a new process rather than ongoing pain alone.
*Minor blood group incompatibility*
- Reactions to minor blood group incompatibilities are usually **milder and delayed** compared to ABO incompatibilities.
- They often involve **extravascular hemolysis**, which might not present with the acute febrile reaction seen here, and are less common a cause of immediate febrile reactions.
*Leukoagglutination reaction*
- This is an older term for what is now often considered a type of **febrile non-hemolytic transfusion reaction (FNHTR)** caused by recipient antibodies to donor leukocyte antigens leading to leukocyte clumping.
- While related to FNHTR, the term "febrile non-hemolytic transfusion reaction" is the more encompassing and appropriate diagnosis given the typical symptom complex of fever, chills, and headache.
Fever patterns and significance US Medical PG Question 4: A 37-year-old man presents to the emergency department for a persistent fever. The patient states he has felt unwell for the past week and has felt subjectively febrile. The patient has a past medical history of a suicide attempt and alcohol abuse. He is not currently taking any medications. The patient admits to using heroin and cocaine and drinking 5-8 alcoholic drinks per day. His temperature is 103°F (39.4°C), blood pressure is 92/59 mmHg, pulse is 110/min, respirations are 20/min, and oxygen saturation is 96% on room air. Cardiopulmonary exam is notable for a systolic murmur heard best along the left sternal border. Dermatologic exam reveals scarring in the antecubital fossa. Which of the following is the next best step in management?
- A. CT scan
- B. Ultrasound
- C. Chest radiograph
- D. Blood cultures (Correct Answer)
- E. Vancomycin and gentamicin
Fever patterns and significance Explanation: ***Blood cultures***
- The patient's history of **intravenous drug use (IVDU)**, persistent fever, and a **new systolic murmur** strongly suggest **infective endocarditis**.
- **Blood cultures** are crucial for identifying the causative organism and guiding appropriate antibiotic therapy, serving as the cornerstone of diagnosis in suspected endocarditis.
*CT scan*
- While CT scans can be useful for identifying complications of endocarditis (e.g., septic emboli in the brain or lungs), they are **not the initial diagnostic step** for identifying the source of infection.
- CT scans expose the patient to **radiation** and are more expensive, making them less suitable as a first step compared to blood cultures.
*Ultrasound*
- An **echocardiogram** (a type of ultrasound) is essential for visualizing vegetations on heart valves, but it is typically performed *after* blood cultures reveal bacteremia to confirm the diagnosis and assess severity.
- A general ultrasound of other body areas would be non-specific and **unlikely to pinpoint the cause** of persistent fever in this clinical context.
*Chest radiograph*
- A chest radiograph can identify **pulmonary infiltrates** or **septic emboli in the lungs**, which are potential complications of right-sided endocarditis (common in IVDU).
- However, a chest radiograph **does not identify the causative organism** or confirm the primary diagnosis of endocarditis, making it a secondary investigation.
*Vancomycin and gentamicin*
- This combination represents a broad-spectrum antibiotic regimen often used for **empiric treatment of infective endocarditis**, particularly in IVDU patients due to concerns for MRSA or resistant streptococcal species.
- While ultimately necessary, administering antibiotics *before* obtaining **blood cultures** can significantly reduce the yield of cultures and hinder definitive diagnosis and tailored treatment.
Fever patterns and significance US Medical PG Question 5: A 61-year-old woman comes to the physician because of a 6-month history of left knee pain and stiffness. Examination of the left knee shows tenderness to palpation along the joint line; there is crepitus with full flexion and extension. An x-ray of the knee shows osteophytes with joint-space narrowing. Arthrocentesis of the knee joint yields clear fluid with a leukocyte count of 120/mm3. Treatment with ibuprofen during the next week significantly improves her condition. The beneficial effect of this drug is most likely due to inhibition of which of the following?
- A. Conversion of hypoxanthine to urate
- B. Conversion of phospholipids to arachidonic acid
- C. Conversion of prostaglandin H2 to thromboxane A2
- D. Conversion of arachidonic acid to prostaglandin G2 (Correct Answer)
- E. Conversion of dihydroorotate to orotate
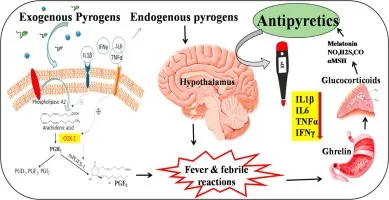
Fever patterns and significance Explanation: ***Conversion of arachidonic acid to prostaglandin G2***
- This patient presents with symptoms and signs consistent with **osteoarthritis**, characterized by joint pain, stiffness, crepitus, and radiographic findings like **osteophytes** and **joint-space narrowing**.
- **Ibuprofen is a non-selective NSAID** that inhibits **cyclooxygenase (COX-1 and COX-2) enzymes**, which catalyze the conversion of **arachidonic acid to prostaglandin G2 (PGG2)**, the first committed step in prostaglandin synthesis.
- By blocking prostaglandin production, ibuprofen reduces inflammation and pain associated with osteoarthritis.
*Conversion of hypoxanthine to urate*
- This process is catalyzed by **xanthine oxidase** and is inhibited by medications like **allopurinol**, used in the treatment of **gout** to reduce uric acid levels.
- Gout typically presents with acute, severe joint pain with signs of inflammation and monosodium urate crystals on joint aspiration, which are not characteristic of this patient's presentation.
*Conversion of phospholipids to arachidonic acid*
- This step is catalyzed by **phospholipase A2**, which is inhibited by **glucocorticoids** (via lipocortin induction).
- While glucocorticoids have potent anti-inflammatory effects by working upstream of the arachidonic acid cascade, ibuprofen has a different mechanism targeting the COX enzymes downstream.
*Conversion of prostaglandin H2 to thromboxane A2*
- This reaction is catalyzed by **thromboxane synthase**, primarily important in platelet aggregation and vasoconstriction.
- NSAIDs like ibuprofen do not specifically inhibit thromboxane synthase; rather, they inhibit COX enzymes upstream, which reduces production of both prostaglandins and thromboxanes.
- Low-dose aspirin preferentially inhibits COX-1 in platelets, reducing thromboxane A2 for cardioprotection, but this is not ibuprofen's primary therapeutic mechanism in osteoarthritis.
*Conversion of dihydroorotate to orotate*
- This is a step in **pyrimidine synthesis**, inhibited by **leflunomide**, a disease-modifying antirheumatic drug (DMARD) used in rheumatoid arthritis.
- This mechanism is unrelated to the action of NSAIDs or the treatment of osteoarthritis.
Fever patterns and significance US Medical PG Question 6: A 20-year-old woman reports to student health complaining of 5 days of viral symptoms including sneezing and a runny nose. She started coughing 2 days ago and is seeking cough medication. She additionally mentions that she developed a fever 2 days ago, but this has resolved. On exam, her temperature is 99.0°F (37.2°C), blood pressure is 118/76 mmHg, pulse is 86/min, and respirations are 12/min. Changes in the activity of warm-sensitive neurons in which part of her hypothalamus likely contributed to the development and resolution of her fever?
- A. Anterior hypothalamus (Correct Answer)
- B. Paraventricular nucleus
- C. Suprachiasmatic nucleus
- D. Lateral area
- E. Posterior hypothalamus
Fever patterns and significance Explanation: ***Anterior hypothalamus***
- The **anterior hypothalamus** contains warm-sensitive neurons that detect increases in body temperature and activate mechanisms for heat dissipation, such as sweating and vasodilation.
- In fever, **prostaglandins** increase the set point in the anterior hypothalamus, causing the body to retain heat and increase heat production until the new set point is reached; resolution of fever involves resetting this set point back to normal.
*Paraventricular nucleus*
- The **paraventricular nucleus** is primarily involved in neuroendocrine functions, stress response, and the regulation of appetite and autonomic nervous system.
- It plays a significant role in releasing hormones like **corticotropin-releasing hormone (CRH)** and **oxytocin**, not direct temperature regulation.
*Suprachiasmatic nucleus*
- The **suprachiasmatic nucleus (SCN)** is the body's main biological clock, regulating **circadian rhythms** including the sleep-wake cycle and daily fluctuations in body temperature.
- While it influences the normal diurnal variation in body temperature, it is not directly responsible for the acute regulation of fever.
*Lateral area*
- The **lateral hypothalamus** primarily functions as the "hunger center," stimulating foraging and feeding behavior.
- Damage to this area can lead to **anorexia** and reduced food intake, not impairments in fever response.
*Posterior hypothalamus*
- The **posterior hypothalamus** is primarily involved in heat conservation and production mechanisms, such as shivering and vasoconstriction, in response to cold.
- It contains cold-sensitive neurons and functions to raise body temperature if it falls below the set point, but it is not where the set point itself is regulated in response to pyrogens.
Fever patterns and significance US Medical PG Question 7: A 42-year-old man comes to his physician with a history of fever, non-bloody diarrhea, and headache for 10 days. He also complains of anorexia and abdominal pain. He returned from a trip to India 3 weeks ago. His temperature is 40.0°C (104.0°F), pulse is 65/min, respirations are 15/min, and blood pressure is 135/80 mm Hg. He has developed a blanchable rash on his chest and trunk. A photograph of the rash is shown. Examination of the heart, lungs, and abdomen show no abnormalities. Laboratory studies show:
Hemoglobin 15 g/dL
Mean corpuscular volume 95 μm3
White blood cell count 3400/mm3
Percent segmented neutrophils 40%
Which of the following is the most likely diagnosis?
- A. Leptospirosis
- B. Enteric fever (Correct Answer)
- C. Dengue fever
- D. Malaria
- E. Nontyphoidal salmonellosis
Fever patterns and significance Explanation: ***Enteric fever***
- The constellation of **fever**, **non-bloody diarrhea**, **bradycardia** (pulse 65/min with 40°C fever), **leukopenia** (WBC 3400/mm³), **rose spots** (blanchable rash on chest/trunk), and recent travel to **India** (endemic area) is highly characteristic of enteric fever caused by *Salmonella Typhi* or *Paratyphi*.
- Abdominal pain, anorexia, and headache are also common symptoms, and the relatively low **neutrophil percentage** (40%) further supports the diagnosis of a bacterial infection with atypical white blood cell response.
*Leptospirosis*
- While leptospirosis can cause **fever** and **headache** and is found in tropical regions, it typically presents with **conjunctival suffusion**, **muscle pain**, and sometimes **jaundice** or **renal involvement**, none of which are detailed here.
- Exposure usually involves contact with contaminated water or soil, and **diarrhea** is less common than in enteric fever.
*Dengue fever*
- Dengue fever is characterized by **high fever**, severe **myalgia** and **arthralgia** ("breakbone fever"), and often a **maculopapular rash**, but **bradycardia** and **leukopenia** with low neutrophils are not typical features.
- **Hemorrhagic manifestations** are also a concern in severe dengue, which are not described.
*Malaria*
- Malaria presents with cyclical **fever** (often paroxysmal), **chills**, **sweats**, and frequently causes **anemia** and **thrombocytopenia**.
- While **leukopenia** can occur, the presence of **rose spots** and sustained fever with relative **bradycardia** point away from malaria as the primary diagnosis.
*Nontyphoidal salmonellosis*
- This typically causes **gastroenteritis** with **diarrhea**, **vomiting**, and **fever**, which is usually self-limiting.
- It would not typically present with **rose spots**, pronounced **bradycardia**, or a prolonged course with systemic symptoms suggestive of enteric fever.
Fever patterns and significance US Medical PG Question 8: A 42-year-old man undergoes therapeutic hypothermia (target temperature 33°C/91.4°F) following cardiac arrest with return of spontaneous circulation. During the cooling phase, he develops shivering, which increases oxygen consumption and interferes with target temperature achievement. He is already on sedation and neuromuscular blockade is being considered. Evaluate the most appropriate management strategy considering both efficacy and safety.
- A. Administer meperidine alone to reduce shivering threshold
- B. Increase sedation and add surface counter-warming of extremities before neuromuscular blockade (Correct Answer)
- C. Abandon therapeutic hypothermia due to complications
- D. Use only mechanical restraints to prevent movement
- E. Immediate neuromuscular blockade without additional measures
Fever patterns and significance Explanation: ***Increase sedation and add surface counter-warming of extremities before neuromuscular blockade***
- A **stepwise approach** to shivering is preferred; increasing **sedation** and using **surface counter-warming** reduces the shivering threshold by tricking the hypothalamus into sensing a warmer periphery.
- This strategy minimizes the need for **neuromuscular blockade**, which can mask seizures and prevent accurate **neurological assessment**.
*Administer meperidine alone to reduce shivering threshold*
- While **meperidine** is an effective anti-shivering agent that lowers the shivering threshold, using it **alone** is often insufficient to control vigorous shivering during induction.
- Reliance on a single pharmacologic agent ignores the **multimodal therapy** benefits of physical measures like skin warming and optimized sedation.
*Abandon therapeutic hypothermia due to complications*
- Shivering is a predictable physiological response, not a reason to abandon **Targeted Temperature Management (TTM)**, which provides significant **neuroprotection** post-cardiac arrest.
- Stopping the therapy would deprive the patient of the benefit of reduced **cerebral metabolic rate** and improved survival outcomes.
*Use only mechanical restraints to prevent movement*
- Mechanical restraints are ineffective against the **metabolic consequences** of shivering, such as increased **oxygen consumption** and CO2 production.
- Shivering is a thermoregulatory reflex, and physical restraint does not stop the underlying **thermogenesis** or metabolic demand.
*Immediate neuromuscular blockade without additional measures*
- **Neuromuscular blockade** should be a last resort as it carries risks of **prolonged muscle weakness** and obscures the patient's clinical neurological status.
- It treats the muscular manifestation but lacks the **sedative or analgesic** properties needed to comfort the patient during the cooling process.
Fever patterns and significance US Medical PG Question 9: A 72-year-old woman with end-stage renal disease on hemodialysis develops fever (103°F/39.4°C) with rigors during dialysis. Blood cultures from both the dialysis catheter and peripheral site grow gram-positive cocci. Despite appropriate antibiotics and catheter removal, she has persistent fevers of 101-102°F (38.3-38.9°C) for 7 days. She feels better and inflammatory markers are decreasing. Evaluate the most likely explanation for persistent fever.
- A. Appropriate lag in temperature resolution despite adequate treatment (Correct Answer)
- B. Undrained abscess requiring surgical intervention
- C. Drug fever from antibiotic therapy
- D. Inadequate dialysis causing uremic fever
- E. Antibiotic-resistant organism requiring regimen change
Fever patterns and significance Explanation: ***Appropriate lag in temperature resolution despite adequate treatment***
- In bacteremia, fever can persist for several days even with effective therapy because **inflammatory cytokines** (like IL-1 and TNF-α) and bacterial products take time to clear from the system.
- The clinical improvement and **decreasing inflammatory markers** (like CRP or ESR) are the most reliable indicators of a positive response to treatment, despite the slow normalization of the **hypothalamic set point**.
*Undrained abscess requiring surgical intervention*
- While a persistent fever can indicate an **occult abscess**, this is less likely when the patient reports feeling clinically better and lab trends are improving.
- Persistent bacteremia or clinical worsening, rather than just isolated fever, would typically necessitate intensive imaging for deep-seated **foci of infection**.
*Drug fever from antibiotic therapy*
- Drug fever is a diagnosis of exclusion that usually occurs after **7 to 10 days** of therapy and is often associated with a newly developed rash or eosinophilia.
- In this case, the patient's fever started with a known **bacterial source** (dialysis catheter), making an infectious resolution lag much more probable than a drug reaction.
*Inadequate dialysis causing uremic fever*
- **Uremia** is more commonly associated with **hypothermia** or a blunted febrile response rather than a high persistent fever.
- Modern dialysis efficiently prevents the build-up of metabolic toxins to levels that would trigger a high-grade **febrile state**.
*Antibiotic-resistant organism requiring regimen change*
- Resistance is unlikely here because the patient is showing **clinical improvement** and a downward trend in inflammatory markers, indicating the current regimen is effective.
- If a **resistant organism** were present, you would expect temperatures to remain very high or increase, and blood cultures to remain positive after 48-72 hours of therapy.
Fever patterns and significance US Medical PG Question 10: A 19-year-old man at a rave party is brought to the ED with agitation, temperature of 107°F (41.7°C), severe hypertension (180/110 mm Hg), tachycardia, dilated pupils, and diaphoresis. His friends report he took 'Molly.' Despite aggressive cooling, his temperature remains dangerously elevated and he develops rhabdomyolysis. Evaluate the most appropriate additional pharmacologic intervention.
- A. Bromocriptine as a dopamine agonist
- B. Benzodiazepines to reduce CNS and muscular hyperactivity (Correct Answer)
- C. Beta-blockers to control hypertension and tachycardia
- D. Antipyretics to reduce hypothalamic set point
- E. Dantrolene sodium to reduce muscle hypermetabolism
Fever patterns and significance Explanation: ***Benzodiazepines to reduce CNS and muscular hyperactivity***
- **MDMA (Ecstasy/Molly)** intoxication causes severe hyperthermia through increased **serotonergic activity**, muscle rigidity, and agitation; **benzodiazepines** are first-line to control agitation and reduce excessive muscle-generated heat.
- Administering **benzodiazepines** also helps manage secondary symptoms like **tachycardia** and **hypertension** by lowering sympathetic outflow.
*Bromocriptine as a dopamine agonist*
- **Bromocriptine** is specifically indicated for **Neuroleptic Malignant Syndrome (NMS)**, which involves dopamine depletion in the hypothalamus and basal ganglia.
- Using it in stimulant or serotonin-mediated toxicity is inappropriate and does not address the primary mechanism of **MDMA**-induced hyperthermia.
*Beta-blockers to control hypertension and tachycardia*
- **Beta-blockers** are generally avoided in stimulant toxicity due to the risk of **unopposed alpha-adrenergic stimulation**, which can worsen **hypertension** and coronary vasoconstriction.
- They do not address the lethal **hyperthermia** or muscle hyperactivity driven by the central nervous system.
*Antipyretics to reduce hypothalamic set point*
- **Antipyretics** like aspirin or acetaminophen are ineffective because the high temperature in **MDMA** toxicity is caused by excess **thermogenesis** (muscle activity), not an altered **hypothalamic set point**.
- Relying on them delays more effective interventions like **evaporative cooling** and sedation.
*Dantrolene sodium to reduce muscle hypermetabolism*
- **Dantrolene** is the specific treatment for **Malignant Hyperthermia** (genetic ryanodine receptor defect) but has limited and controversial evidence in **serotonin syndrome** or MDMA toxicity.
- While it acts on muscle metabolism, **benzodiazepines** should be prioritized to treat the underlying **CNS-mediated agitation** and excessive movement.
More Fever patterns and significance US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.