Fever pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fever pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fever pathophysiology US Medical PG Question 1: A 6-year-old boy is presented to a pediatric clinic by his mother with complaints of fever, malaise, and cough for the past 2 days. He frequently complains of a sore throat and has difficulty eating solid foods. The mother mentions that, initially, the boy’s fever was low-grade and intermittent but later became high grade and continuous. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The past medical history is noncontributory. The boy takes a multivitamin every day. The mother reports that he does well in school and is helpful around the house. The boy’s vital signs include blood pressure 110/65 mm Hg, heart rate 110/min, respiratory rate 32/min, and temperature 38.3°C (101.0°F). On physical examination, the boy appears uncomfortable and has difficulty breathing. His heart is mildly tachycardic with a regular rhythm and his lungs are clear to auscultation bilaterally. Oropharyngeal examination shows that his palatine tonsils are covered with pus and that there is erythema of the surrounding mucosa. Which of the following mediators is responsible for this patient’s elevated temperature?
- A. Leukotriene D4
- B. Prostaglandin F2
- C. Prostaglandin E2 (Correct Answer)
- D. Thromboxane A2
- E. Prostaglandin I2
Fever pathophysiology Explanation: ***Prostaglandin E2***
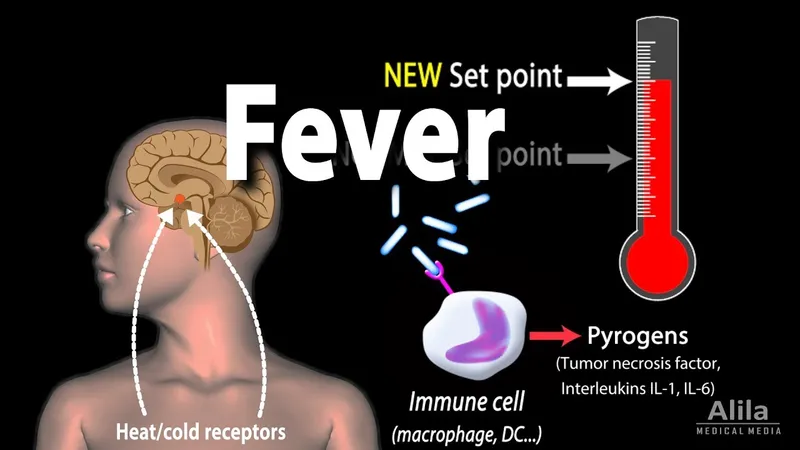
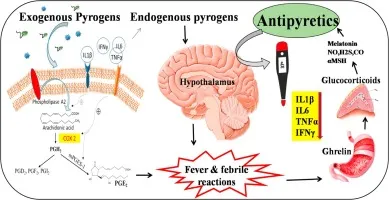
- **Prostaglandin E2 (PGE2)** is a key mediator of fever, acting directly on the **hypothalamus** to reset the body's thermoregulatory set point.
- In response to infection and inflammation, immune cells release **pyrogens** (like IL-1, TNF-alpha), which stimulate PGE2 synthesis in the brain, leading to increased body temperature.
*Leukotriene D4*
- **Leukotriene D4 (LTD4)** is a potent mediator of **bronchoconstriction** and increased **vascular permeability**, particularly in allergic reactions and asthma.
- While it plays a role in inflammation, it does not directly cause fever by altering the hypothalamic set point.
*Prostaglandin F2*
- **Prostaglandin F2 (PGF2)** has various physiological roles, including **uterine contraction** and **bronchoconstriction**, and is important for reproductive functions.
- It is not primarily involved in mediating the febrile response to infection.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is predominantly involved in **platelet aggregation** and **vasoconstriction**, playing a crucial role in hemostasis and thrombosis.
- While it is a product of the arachidonic acid pathway, it does not directly contribute to fever.
*Prostaglandin I2*
- **Prostaglandin I2 (PGI2)**, also known as **prostacyclin**, is a potent **vasodilator** and inhibitor of **platelet aggregation**, protecting the vascular endothelium.
- It typically counteracts the effects of TXA2 and is not a mediator of fever.
Fever pathophysiology US Medical PG Question 2: A 55-year-old woman with diabetes presents to the emergency department due to swelling of her left leg, fever, and chills for the past 2 days. The woman’s maximum recorded temperature at home was 38.3°C (101.0°F). Her left leg is red and swollen from her ankle to the calf, with an ill-defined edge. Her vital signs include: blood pressure 120/78 mm Hg, pulse rate 94/min, temperature 38.3°C (101.0°F), and respiratory rate 16/min. On physical examination, her left leg shows marked tenderness and warmth compared with her right leg. The left inguinal lymph node is enlarged to 3 x 3 cm. Which of the following chemical mediators is the most likely cause of the woman’s fever?
- A. Bradykinin
- B. Histamine
- C. PGE2 (Correct Answer)
- D. Arachidonic acid
- E. LTB4
Fever pathophysiology Explanation: ***PGE2***
- **Prostaglandin E2 (PGE2)** is a potent **pyrogen** that acts on the **hypothalamus** to reset the body's thermoregulatory set point, leading to fever.
- In infections like **cellulitis**, inflammatory mediators stimulate the production of PGE2, causing the systemic symptom of fever.
*Bradykinin*
- **Bradykinin** primarily mediates **pain** and **vasodilation** at the site of inflammation.
- While it contributes to local signs of inflammation, it is not a direct mediator of systemic fever.
*Histamine*
- **Histamine** is a key mediator in immediate **hypersensitivity reactions** and local inflammation, causing **vasodilation** and increased **vascular permeability**.
- It does not directly induce fever by acting on the thermoregulatory center.
*Arachidonic acid*
- **Arachidonic acid** is a **precursor** molecule derived from membrane phospholipids, which is metabolized to various inflammatory mediators like prostaglandins and leukotrienes.
- It is not a direct chemical mediator of fever itself; rather, its downstream products such as PGE2 are.
*LTB4*
- **Leukotriene B4 (LTB4)** is a potent **chemotactic agent** for neutrophils, playing a role in immune cell recruitment to the site of inflammation.
- While involved in inflammation, LTB4 does not directly cause fever.
Fever pathophysiology US Medical PG Question 3: A 3-day-old female newborn is brought to the emergency department because of fever, poor feeding, and irritability for 6 hours. She was delivered at home at 39 weeks' gestation and delivery was uncomplicated. The mother had no prenatal care. Her temperature is 39.8°C (103.6°F), pulse is 172/min, respirations are 58/min, and blood pressure is 74/45 mm Hg. She appears lethargic. Physical examination shows expiratory grunting and nasal flaring. Serum studies show elevated levels of interleukin-6. Which of the following is the most likely effect of this laboratory finding?
- A. Decreased synthesis of hepcidin
- B. Decreased expression of MHC class II
- C. Increased release of fibrinogen (Correct Answer)
- D. Increased classical activation of macrophages
- E. Increased production of IgE
Fever pathophysiology Explanation: ***Increased release of fibrinogen***
- **Interleukin-6 (IL-6)** is a major **pro-inflammatory cytokine** that stimulates the liver to produce **acute phase reactants**, including **fibrinogen**.
- This increase in fibrinogen is part of the body's non-specific immune response to infection and inflammation, leading to elevated inflammatory markers like **ESR**.
*Decreased synthesis of hepcidin*
- **Hepcidin** synthesis is *increased* by IL-6, not decreased, as part of the body's response to inflammation to limit iron availability to pathogens.
- High levels of hepcidin lead to **anemia of chronic disease** by inhibiting iron absorption and release from macrophages.
*Decreased expression of MHC class II*
- IL-6 generally *enhances* immune responses, and while it doesn't directly increase MHC class II expression on antigen-presenting cells, reduced expression is not a typical effect.
- **MHC class II** expression is primarily regulated by cytokines like **interferon-gamma** and helps present antigens to T-helper cells.
*Increased classical activation of macrophages*
- **Classical activation of macrophages** (M1 polarization) is primarily driven by **interferon-gamma (IFN-γ)** and **TNF-α**, often in response to pathogen signals.
- While IL-6 can contribute to the overall inflammatory environment, it is not the primary cytokine for classical macrophage activation; rather, it often promotes alternative (M2) phenotypes or has pleiotropic effects.
*Increased production of IgE*
- **IgE production** is primarily associated with **allergic reactions** and **parasitic infections**, driven by cytokines like **IL-4** and **IL-13**.
- IL-6 is not directly involved in stimulating IgE synthesis; its main roles are in inflammation, hematopoiesis, and the acute phase response.
Fever pathophysiology US Medical PG Question 4: A group of investigators is studying thermoregulatory adaptations of the human body. A subject is seated in a thermally insulated isolation chamber with an internal temperature of 48°C (118°F), a pressure of 1 atmosphere, and a relative humidity of 10%. Which of the following is the primary mechanism of heat loss in this subject?
- A. Convection
- B. Evaporation (Correct Answer)
- C. Conduction
- D. Piloerection
- E. Radiation
Fever pathophysiology Explanation: ***Evaporation***
- In an environment where the ambient temperature (48°C) is **higher than body temperature**, heat gain by convection, conduction, and radiation occurs. Therefore, **evaporation** of sweat is the only significant mechanism for heat loss.
- The relatively low humidity (10%) at this high temperature facilitates efficient sweat **evaporation**, which cools the body as it converts liquid sweat into water vapor.
*Convection*
- **Convection** involves heat transfer through the movement of air or fluid over the body surface.
- Since the ambient temperature (48°C) is significantly **above body temperature**, the body would gain heat via convection, not lose it.
*Conduction*
- **Conduction** is direct heat transfer between objects in contact.
- As the ambient temperature (48°C) is much **higher than the skin temperature**, the body would actually **gain heat** through conduction from any surfaces it touched if they were at ambient temperature.
*Piloerection*
- **Piloerection** (goosebumps) is a mechanism for minimizing heat loss by trapping a layer of warm air close to the skin.
- This response is activated in **cold environments** to conserve heat, not in hot environments to dissipate it.
*Radiation*
- **Radiation** is heat transfer via electromagnetic waves without direct contact.
- Since the ambient temperature (48°C) is **higher than body surface temperature**, the body would **gain heat** by radiation, not lose it efficiently, from the surrounding environment.
Fever pathophysiology US Medical PG Question 5: A researcher is studying how arachidonic acid metabolites mediate the inflammatory response in rats. She has developed multiple enzyme inhibitors that specifically target individual proteins in the arachidonic acid pathway. She injects these inhibitors in rats who have been exposed to common bacterial pathogens and analyzes their downstream effects. In one of her experiments, she injects a leukotriene B4 inhibitor into a rat and observes an abnormal cell response. Which of the following interleukins would most closely restore the function of one of the missing products?
- A. Interleukin 2
- B. Interleukin 4
- C. Interleukin 1
- D. Interleukin 5
- E. Interleukin 8 (Correct Answer)
Fever pathophysiology Explanation: ***Interleukin 8***
- **Leukotriene B4 (LTB4)** is a potent **chemoattractant** and activator of neutrophils.
- **Interleukin 8 (IL-8)**, also known as **CXCL8**, is a primary **chemoattractant** for neutrophils, functionally mimicking the role of LTB4 in recruiting these inflammatory cells to the site of infection.
*Interleukin 2*
- **IL-2** is primarily involved in the **growth, proliferation, and differentiation of T cells**, as well as the activation of B cells and natural killer cells.
- It does not have a significant role in **neutrophil chemotaxis**, which is the main function of LTB4.
*Interleukin 4*
- **IL-4** is crucial for **B cell activation** and class switching to IgE, and it's a key cytokine in the **Th2 immune response**.
- Its functions are related to **allergic reactions** and **parasitic infections**, not neutrophil recruitment.
*Interleukin 1*
- **IL-1** is a pro-inflammatory cytokine that mediates a wide range of immune responses, including **fever** and the activation of other immune cells.
- While it contributes to inflammation, it does not directly act as a **chemoattractant for neutrophils** in the same manner as LTB4 or IL-8.
*Interleukin 5*
- **IL-5** is primarily involved in the **growth and differentiation of eosinophils** and B cell IgA production.
- It plays a significant role in **allergic reactions** and defense against parasites, not neutrophil chemotaxis.
Fever pathophysiology US Medical PG Question 6: While playing in the woods with friends, a 14-year-old African-American male is bitten by an insect. Minutes later he notices swelling and redness at the site of the insect bite. Which substance has directly led to the wheal formation?
- A. IFN-gamma
- B. IL-4
- C. IL-22
- D. Histamine (Correct Answer)
- E. Arachidonic acid
Fever pathophysiology Explanation: ***Histamine***
- **Histamine** is a key mediator released by **mast cells** and basophils during immediate hypersensitivity reactions, such as an insect bite.
- It causes vasodilation, increased vascular permeability, and itching, leading to the characteristic **wheal and flare** response.
*IFN-gamma*
- **IFN-gamma** is primarily involved in **Type IV hypersensitivity** (delayed-type) reactions and viral/intracellular bacterial defense.
- It would not directly cause immediate wheal formation from an insect bite.
*IL-4*
- **IL-4** is crucial for **Th2 differentiation** and IgE production, which is involved in allergic reactions.
- While essential for the underlying allergic response, it does not directly cause the acute wheal formation.
*IL-22*
- **IL-22** is involved in host defense, particularly against extracellular bacteria, and plays a role in tissue repair and inflammation, especially in epithelial tissues.
- It is not a primary mediator of immediate hypersensitivity reactions or wheal formation.
*Arachidonic acid*
- **Arachidonic acid** is a precursor to eicosanoids (prostaglandins, leukotrienes), which mediate later phases of inflammation and pain.
- While contributing to the overall inflammatory response, it does not directly cause the initial, rapid wheal formation.
Fever pathophysiology US Medical PG Question 7: A 38-year-old man comes to the physician because of severe muscle pain and swelling of his eyelids for 3 days. He has also had fever and chills during this period. For the last 2 days, he has had severe pain in his mouth while chewing. He had an episode of diarrhea a month ago for which he did not seek medical care. He has no history of serious illness. His sister has dermatomyositis. He returned from a hunting trip to eastern Europe 45 days ago. His temperature is 38.1°C (100.6°F), pulse is 80/min, and blood pressure is 130/70 mm Hg. Examination shows periorbital edema and severe generalized muscle tenderness. There are splinter hemorrhages on both hands. Laboratory studies show:
Hemoglobin 14.2 g/dL
Leukocyte count 12,500/mm3
Segmented neutrophils 60%
Eosinophils 18%
Lymphocytes 20%
Monocytes 2%
Serum
Glucose 117 mg/dL
Creatinine 1.1 mg/dL
Alkaline phosphatase 72 U/L
Creatine kinase 765 U/L
Urinalysis is within normal limits. Which of the following is most likely to have prevented this patient's condition?
- A. Consume pasteurized dairy products
- B. Clean drinking water
- C. Cooking meat to 71°C (160°F) (Correct Answer)
- D. Metronidazole at the onset of diarrhea
- E. Influenza vaccine
Fever pathophysiology Explanation: ***Cooking meat to 71°C (160°F)***
- This patient's symptoms (fever, **periorbital edema**, **severe myalgia**, **eosinophilia**, elevated CK) after a hunting trip to eastern Europe are highly suggestive of **Trichinellosis**, caused by consuming undercooked meat infected with *Trichinella* larvae.
- **Thoroughly cooking meat** (especially wild game or pork) to an internal temperature of 71°C (160°F) is a primary preventative measure against *Trichinella* infection, as it kills the larvae.
*Consume pasteurized dairy products*
- Consuming pasteurized dairy products prevents infections such as **brucellosis** or **listeriosis**.
- These infections typically present with different clinical features, and their transmission is not associated with hunting wild game in Eastern Europe in the context of the patient's symptoms.
*Clean drinking water*
- Access to clean drinking water is crucial for preventing waterborne diseases like **giardiasis**, **cholera**, or **typhoid fever**.
- While the patient had diarrhea, the subsequent systemic symptoms with muscle involvement and eosinophilia point away from typical waterborne illnesses as the primary cause of his current condition.
*Metronidazole at the onset of diarrhea*
- **Metronidazole** is an antibiotic used to treat parasitic infections like **Giardia** or bacterial infections such as those caused by *Clostridium difficile*.
- Treating diarrhea with metronidazole, even if effective for the initial gastrointestinal issue, would not prevent a subsequent *Trichinella* infection which is acquired through undercooked meat.
*Influenza vaccine*
- The **influenza vaccine** protects against the **influenza virus**, which causes respiratory symptoms, fever, and generalized myalgia.
- However, the absence of prominent respiratory symptoms, the presence of marked eosinophilia, periorbital edema, and the history of recent exposure to wild game make influenza an unlikely diagnosis.
Fever pathophysiology US Medical PG Question 8: A parent presents to her pediatrician requesting information about immunizations for her newborn. The pediatrician explains about basic principles of immunization, types of vaccines, possible adverse effects, and the immunization schedule. Regarding how immunizations work, the pediatrician explains that there are mainly 2 types of vaccines. The first type of vaccine provides stronger and more lasting immunity as it induces both cellular and humoral immune responses. The second type of vaccine produces mainly a humoral response only, and its overall efficacy is less as compared to the first type. Which of the following vaccines belongs to the first type of vaccine that the pediatrician is talking about?
- A. Hepatitis A vaccine
- B. Polio vaccine (Salk)
- C. Yellow fever vaccine (Correct Answer)
- D. Rabies vaccine
- E. Hepatitis B vaccine
Fever pathophysiology Explanation: ***Yellow fever vaccine***
- The Yellow fever vaccine is a **live-attenuated vaccine**, which mimics natural infection and effectively stimulates both **cellular and humoral immune responses**, leading to strong and long-lasting immunity.
- Live-attenuated vaccines contain a weakened form of the pathogen, allowing for replication within the host and robust immune system activation.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is an **inactivated vaccine**, which primarily induces a **humoral (antibody-mediated) immune response**.
- Inactivated vaccines generally do not stimulate a strong cellular immune response and often require booster doses to maintain protective immunity.
*Polio vaccine (Salk)*
- The Salk polio vaccine is an **inactivated polio vaccine (IPV)**, meaning it contains killed viral particles.
- As an inactivated vaccine, it mainly elicits a **humoral immune response** producing circulating antibodies but less mucosal or cellular immunity.
*Rabies vaccine*
- The Rabies vaccine is an **inactivated vaccine** given after exposure or for pre-exposure prophylaxis.
- It primarily induces a **humoral antibody response** rather than a strong cellular immune response.
*Hepatitis B vaccine*
- The Hepatitis B vaccine is a **recombinant vaccine**, containing only a portion of the viral antigen (HBsAg).
- This type of vaccine primarily stimulates a **humoral immune response** leading to antibody production, which is effective but does not typically induce a strong cellular response like live vaccines.
Fever pathophysiology US Medical PG Question 9: An investigator is studying the clearance of respiratory particles in healthy non-smokers. An aerosol containing radio-labeled particles that are small enough to reach the alveoli is administered to the subjects via a non-rebreather mask. A gamma scanner is then used to evaluate the rate of particle clearance from the lungs. The primary mechanism of particle clearance most likely involves which of the following cell types?
- A. Goblet cells
- B. Macrophages (Correct Answer)
- C. Club cells
- D. Type I pneumocytes
- E. Neutrophils
Fever pathophysiology Explanation: ***Macrophages***
- **Alveolar macrophages** are the primary phagocytic cells in the alveoli responsible for clearing inhaled particles that reach this deepest part of the lung.
- They engulf and digest foreign substances, including pathogens and inert particles, protecting the delicate alveolar structures.
*Goblet cells*
- **Goblet cells** are found in the larger airways (trachea, bronchi), where they produce mucus to trap inhaled particles.
- They are not present in the alveoli, so they cannot clear particles that have reached this region.
*Club cells*
- **Club cells** (formerly Clara cells) are located in the bronchioles and secrete components of the surfactant-like material, but they do not primarily function in particle clearance.
- While they have some protective roles, they are not the main phagocytic cells for alveolar particles.
*Type I pneumocytes*
- **Type I pneumocytes** are flattened, thin cells that form the majority of the alveolar surface and are primarily involved in gas exchange.
- They are not phagocytic and do not play a direct role in clearing inhaled particles.
*Neutrophils*
- **Neutrophils** are acute inflammatory cells primarily involved in combating bacterial infections.
- While they can migrate to the lungs during inflammation, they are not the primary, routine phagocytic cells for clearing inhaled particles in healthy individuals.
Fever pathophysiology US Medical PG Question 10: A 42-year-old man undergoes therapeutic hypothermia (target temperature 33°C/91.4°F) following cardiac arrest with return of spontaneous circulation. During the cooling phase, he develops shivering, which increases oxygen consumption and interferes with target temperature achievement. He is already on sedation and neuromuscular blockade is being considered. Evaluate the most appropriate management strategy considering both efficacy and safety.
- A. Administer meperidine alone to reduce shivering threshold
- B. Increase sedation and add surface counter-warming of extremities before neuromuscular blockade (Correct Answer)
- C. Abandon therapeutic hypothermia due to complications
- D. Use only mechanical restraints to prevent movement
- E. Immediate neuromuscular blockade without additional measures
Fever pathophysiology Explanation: ***Increase sedation and add surface counter-warming of extremities before neuromuscular blockade***
- A **stepwise approach** to shivering is preferred; increasing **sedation** and using **surface counter-warming** reduces the shivering threshold by tricking the hypothalamus into sensing a warmer periphery.
- This strategy minimizes the need for **neuromuscular blockade**, which can mask seizures and prevent accurate **neurological assessment**.
*Administer meperidine alone to reduce shivering threshold*
- While **meperidine** is an effective anti-shivering agent that lowers the shivering threshold, using it **alone** is often insufficient to control vigorous shivering during induction.
- Reliance on a single pharmacologic agent ignores the **multimodal therapy** benefits of physical measures like skin warming and optimized sedation.
*Abandon therapeutic hypothermia due to complications*
- Shivering is a predictable physiological response, not a reason to abandon **Targeted Temperature Management (TTM)**, which provides significant **neuroprotection** post-cardiac arrest.
- Stopping the therapy would deprive the patient of the benefit of reduced **cerebral metabolic rate** and improved survival outcomes.
*Use only mechanical restraints to prevent movement*
- Mechanical restraints are ineffective against the **metabolic consequences** of shivering, such as increased **oxygen consumption** and CO2 production.
- Shivering is a thermoregulatory reflex, and physical restraint does not stop the underlying **thermogenesis** or metabolic demand.
*Immediate neuromuscular blockade without additional measures*
- **Neuromuscular blockade** should be a last resort as it carries risks of **prolonged muscle weakness** and obscures the patient's clinical neurological status.
- It treats the muscular manifestation but lacks the **sedative or analgesic** properties needed to comfort the patient during the cooling process.
More Fever pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.