Environmental stress responses US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Environmental stress responses. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Environmental stress responses US Medical PG Question 1: A 6-year-old boy is presented to a pediatric clinic by his mother with complaints of fever, malaise, and cough for the past 2 days. He frequently complains of a sore throat and has difficulty eating solid foods. The mother mentions that, initially, the boy’s fever was low-grade and intermittent but later became high grade and continuous. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The past medical history is noncontributory. The boy takes a multivitamin every day. The mother reports that he does well in school and is helpful around the house. The boy’s vital signs include blood pressure 110/65 mm Hg, heart rate 110/min, respiratory rate 32/min, and temperature 38.3°C (101.0°F). On physical examination, the boy appears uncomfortable and has difficulty breathing. His heart is mildly tachycardic with a regular rhythm and his lungs are clear to auscultation bilaterally. Oropharyngeal examination shows that his palatine tonsils are covered with pus and that there is erythema of the surrounding mucosa. Which of the following mediators is responsible for this patient’s elevated temperature?
- A. Leukotriene D4
- B. Prostaglandin F2
- C. Prostaglandin E2 (Correct Answer)
- D. Thromboxane A2
- E. Prostaglandin I2
Environmental stress responses Explanation: ***Prostaglandin E2***
- **Prostaglandin E2 (PGE2)** is a key mediator of fever, acting directly on the **hypothalamus** to reset the body's thermoregulatory set point.
- In response to infection and inflammation, immune cells release **pyrogens** (like IL-1, TNF-alpha), which stimulate PGE2 synthesis in the brain, leading to increased body temperature.
*Leukotriene D4*
- **Leukotriene D4 (LTD4)** is a potent mediator of **bronchoconstriction** and increased **vascular permeability**, particularly in allergic reactions and asthma.
- While it plays a role in inflammation, it does not directly cause fever by altering the hypothalamic set point.
*Prostaglandin F2*
- **Prostaglandin F2 (PGF2)** has various physiological roles, including **uterine contraction** and **bronchoconstriction**, and is important for reproductive functions.
- It is not primarily involved in mediating the febrile response to infection.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is predominantly involved in **platelet aggregation** and **vasoconstriction**, playing a crucial role in hemostasis and thrombosis.
- While it is a product of the arachidonic acid pathway, it does not directly contribute to fever.
*Prostaglandin I2*
- **Prostaglandin I2 (PGI2)**, also known as **prostacyclin**, is a potent **vasodilator** and inhibitor of **platelet aggregation**, protecting the vascular endothelium.
- It typically counteracts the effects of TXA2 and is not a mediator of fever.
Environmental stress responses US Medical PG Question 2: Two-hours into recovery from general anesthesia for an orthopedic fracture, a 34-year-old woman develops fever and masseter muscle rigidity with lockjaw. She has no history of a similar episode. She has no history of serious illness and takes no medications. She appears confused. In the recovery room, her blood pressure is 78/50 mm Hg, the pulse is 128/min, the respirations are 42/min, and the temperature is 40.3°C (104.5°F). Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Serum
Na+ 145 mEq/L
K+ 6.5 mEq/L
Arterial blood gas on room air
pH 7.01
PCO2 78 mm Hg
HCO3− 14 mEq/L
PO2 55 mm Hg
The patient is reintubated. Which of the following is the most appropriate next step in pharmacotherapy?
- A. Lorazepam
- B. Diphenhydramine
- C. Dantrolene (Correct Answer)
- D. Labetalol
- E. Cyproheptadine
Environmental stress responses Explanation: ***Dantrolene***
- The patient exhibits classic signs of **malignant hyperthermia**, including
**masseter muscle rigidity**, **fever (40.3°C)**, **tachycardia (128/min)**,
**tachypnea (42/min)**, and **hypotension (78/50 mm Hg)**. The **elevated potassium (6.5
mEq/L)**, **acidosis (pH 7.01)**, and **hypercapnia (PCO2 78 mm Hg)**
further support this diagnosis.
- **Dantrolene** is the only specific antidote for malignant hyperthermia as
it acts as a **ryanodine receptor antagonist**, inhibiting calcium release
from the sarcoplasmic reticulum and thereby reducing muscle contracture and
heat production.
*Lorazepam*
- **Lorazepam** is a benzodiazepine used for treating seizures, anxiety, and
agitation, but it does **not address the underlying pathophysiology of
malignant hyperthermia**.
- While the patient appears confused, this is likely secondary to the
metabolic derangements and hyperthermia, not a primary indication for
lorazepam.
*Diphenhydramine*
- **Diphenhydramine** is an antihistamine used to treat allergic reactions or
sedation; it has no role in the management of malignant hyperthermia.
- It would not alleviate the muscle rigidity, hyperthermia, or metabolic
abnormalities seen in this patient.
*Labetalol*
- **Labetalol** is a beta-blocker used to manage hypertension and tachycardia,
but these are symptoms of malignant hyperthermia rather than the root
cause.
- While it could temporarily lower heart rate and blood pressure, it **does
not address the excessive calcium release** in skeletal muscle, which is
the hallmark of malignant hyperthermia.
*Cyproheptadine*
- **Cyproheptadine** is a serotonin antagonist used in the treatment of
serotonin syndrome.
- Malignant hyperthermia and serotonin syndrome share some clinical features
like hyperthermia, but the **trigger (anesthetic agents)** and underlying
mechanisms are different, making cyproheptadine ineffective here.
Environmental stress responses US Medical PG Question 3: An infant boy of unknown age and medical history is dropped off in the emergency department. The infant appears lethargic and has a large protruding tongue. Although the infant exhibits signs of neglect, he is in no apparent distress. The heart rate is 70/min, the respiratory rate is 30/min, and the temperature is 35.7°C (96.2°F). Which of the following is the most likely cause of the patient’s physical exam findings?
- A. Autosomal dominant mutation in the SERPING1 gene
- B. Genetic imprinting disorder affecting chromosome 11p15.5
- C. Type I hypersensitivity reaction
- D. Excess growth hormone secondary to pituitary gland tumor
- E. Congenital agenesis of an endocrine gland in the anterior neck (Correct Answer)
Environmental stress responses Explanation: ***Congenital agenesis of an endocrine gland in the anterior neck***
- This description is highly suggestive of **congenital hypothyroidism**, caused by **thyroid dysgenesis** (agenesis or hypoplasia of the thyroid gland).
- Symptoms include **lethargy**, **macroglossia** (large protruding tongue), **hypotonia**, **feeding difficulties**, **umbilical hernia**, and **hypothermia**, all consistent with the clinical picture.
*Autosomal dominant mutation in the SERPING1 gene*
- A mutation in the **SERPING1 gene** causes **hereditary angioedema**, characterized by recurrent episodes of unpredictable swelling in various body parts.
- While swelling can affect the tongue, it is typically episodic, painful, and often triggered, which is not suggested by the chronic lethargy and physical signs described.
*Genetic imprinting disorder affecting chromosome 11p15.5*
- This describes **Beckwith-Wiedemann syndrome**, an overgrowth disorder caused by imprinting defects involving genes like **IGF2**, **H19**, and **CDKN1C** on chromosome 11p15.5.
- Features include **macroglossia**, **macrosomia**, **umbilical hernia**, **hemihyperplasia**, and increased risk of embryonal tumors like **Wilms tumor**.
- However, Beckwith-Wiedemann syndrome does not typically present with profound **lethargy** and **hypothermia** as seen in congenital hypothyroidism.
*Type I hypersensitivity reaction*
- A **Type I hypersensitivity reaction** (e.g., anaphylaxis) could cause acute **angioedema** of the tongue, but this would be an acute, rapidly progressing, and life-threatening event.
- The infant's description of being "in no apparent distress" and exhibiting chronic signs like lethargy and hypothermia makes an acute allergic reaction unlikely.
*Excess growth hormone secondary to pituitary gland tumor*
- **Excess growth hormone** (gigantism in children, acromegaly in adults) can cause **macroglossia** and coarse facial features in the long term.
- However, it does not explain the associated **lethargia**, **hypothermia**, and profound developmental delay seen in congenital hypothyroidism in an infant.
Environmental stress responses US Medical PG Question 4: An 11-year-old boy presents with a 2-day history of uncontrollable shivering. During admission, the patient’s vital signs are within normal limits, except for a fluctuating body temperature registering as low as 35.0°C (95.0°F) and as high as 40.0°C (104.0°F), requiring alternating use of cooling and warming blankets. A complete blood count (CBC) is normal, and a chest radiograph is negative for consolidations and infiltrates. An MRI of the brain reveals a space-occupying lesion infiltrating the posterior hypothalamus and extending laterally. Which of the following additional findings are most likely, based on this patient’s physical examination?
- A. Polyuria
- B. Hyperphagia
- C. Galactorrhea
- D. Sleep disturbances
- E. Anorexia (Correct Answer)
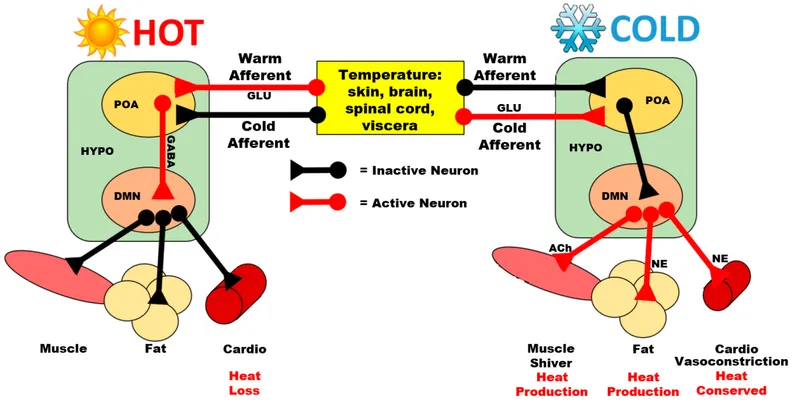
Environmental stress responses Explanation: **Anorexia**
- **Hypothalamic lesions**, particularly those affecting the **lateral hypothalamus**, often lead to **anorexia** and **weight loss** due to the role of this region in stimulating appetite.
- The patient's presentation with **uncontrollable shivering** and **deregulated body temperature** further points to hypothalamic dysfunction, which can also disrupt feeding centers.
*Polyuria*
- **Polyuria** is typically associated with damage to the **posterior pituitary gland** or its connections to the hypothalamus, leading to **diabetes insipidus** (lack of ADH).
- While a hypothalamic lesion can affect ADH production, the primary symptom constellation in this case more strongly suggests disruption of other hypothalamic functions.
*Hyperphagia*
- **Hyperphagia** (increased appetite) and **obesity** are most commonly linked to damage to the **ventromedial hypothalamus**, which is considered the satiety center.
- The presented lesion is described as infiltrating the posterior hypothalamus and extending laterally, making hyperphagia less likely than anorexia.
*Galactorrhea*
- **Galactorrhea** is often caused by **hyperprolactinemia**, which can result from lesions compressing the **pituitary stalk** or interfering with **dopamine's inhibitory effect** on prolactin release in the anterior pituitary.
- While a large hypothalamic lesion could theoretically impact pituitary function secondarily, galactorrhea is not a direct or most likely consequence of a posterior and lateral hypothalamic lesion.
*Sleep disturbances*
- While the **hypothalamus** plays a critical role in **sleep-wake cycles** (e.g., the **suprachiasmatic nucleus**), **uncontrollable shivering** and **poikilothermia** point more directly to acute disruption of temperature regulation rather than sleep disturbances as the most prominent likely additional finding.
- Many types of brain lesions can cause sleep disturbances, but the specific presentation here suggests a more particular set of hypothalamic dysfunctions.
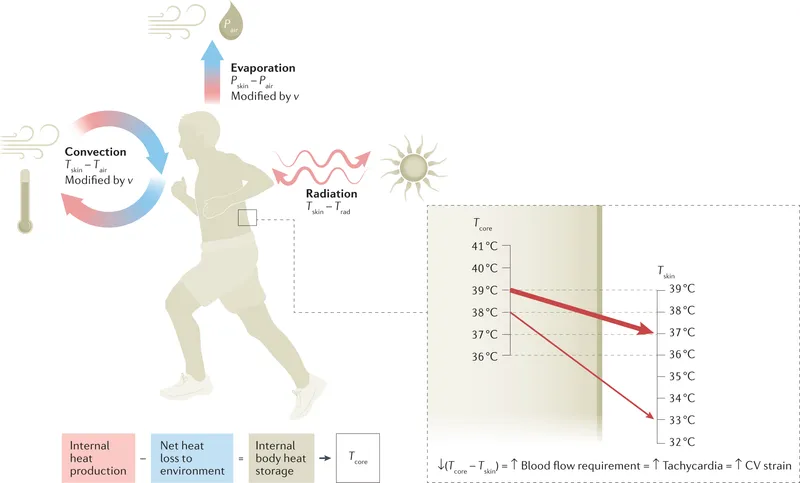
Environmental stress responses US Medical PG Question 5: A group of investigators is studying thermoregulatory adaptations of the human body. A subject is seated in a thermally insulated isolation chamber with an internal temperature of 48°C (118°F), a pressure of 1 atmosphere, and a relative humidity of 10%. Which of the following is the primary mechanism of heat loss in this subject?
- A. Convection
- B. Evaporation (Correct Answer)
- C. Conduction
- D. Piloerection
- E. Radiation
Environmental stress responses Explanation: ***Evaporation***
- In an environment where the ambient temperature (48°C) is **higher than body temperature**, heat gain by convection, conduction, and radiation occurs. Therefore, **evaporation** of sweat is the only significant mechanism for heat loss.
- The relatively low humidity (10%) at this high temperature facilitates efficient sweat **evaporation**, which cools the body as it converts liquid sweat into water vapor.
*Convection*
- **Convection** involves heat transfer through the movement of air or fluid over the body surface.
- Since the ambient temperature (48°C) is significantly **above body temperature**, the body would gain heat via convection, not lose it.
*Conduction*
- **Conduction** is direct heat transfer between objects in contact.
- As the ambient temperature (48°C) is much **higher than the skin temperature**, the body would actually **gain heat** through conduction from any surfaces it touched if they were at ambient temperature.
*Piloerection*
- **Piloerection** (goosebumps) is a mechanism for minimizing heat loss by trapping a layer of warm air close to the skin.
- This response is activated in **cold environments** to conserve heat, not in hot environments to dissipate it.
*Radiation*
- **Radiation** is heat transfer via electromagnetic waves without direct contact.
- Since the ambient temperature (48°C) is **higher than body surface temperature**, the body would **gain heat** by radiation, not lose it efficiently, from the surrounding environment.
Environmental stress responses US Medical PG Question 6: A 16-year-old girl is brought to the emergency department unresponsive. A witness reports that she became anxious, lightheaded, and began sweating and trembling a few minutes before she lost consciousness. Her vitals are as follows: blood pressure 95/60 mm Hg, heart rate 110/min, respiratory rate 21/min, and temperature 35.5°C (95.5°F). She becomes responsive but is still somnolent. She complains of dizziness and weakness. A more detailed history reveals that she has drastically restricted her diet to lose weight for the past 18 hours, and has not eaten today. Her skin is pale, wet, and cold. The rest of the physical examination is unremarkable. Blood testing shows a plasma glucose level of 2.8 mmol/L (50.5 mg/dL). Which of the following statements is true?
- A. Hypoglycemia in this patient is being compensated with an increased glycogenolysis rate. (Correct Answer)
- B. Epinephrine-induced gluconeogenesis is the main process that allows for the compensation of a decreased glucose level.
- C. There is an increase in the glycogen synthesis rate in this patient’s hepatocytes.
- D. The patient’s symptoms are most likely the consequence of increased insulin secretion from the pancreatic islets.
- E. The patient’s hypoglycemia inhibits glucagon release from pancreatic alpha cells.
Environmental stress responses Explanation: ***Hypoglycemia in this patient is being compensated with an increased glycogenolysis rate.***
- The patient's symptoms (anxiety, sweating, trembling, dizziness, weakness) and **low blood glucose (2.8 mmol/L)** confirm hypoglycemia. The immediate physiological response to hypoglycemia is the release of counter-regulatory hormones (glucagon, epinephrine, cortisol, growth hormone) which stimulate **glycogenolysis** (breakdown of glycogen to glucose) in the liver to maintain blood glucose, especially in the initial hours of fasting.
- Given that she has only fasted for 18 hours, her **hepatic glycogen stores** would still be recruited to provide glucose, making increased glycogenolysis a primary compensatory mechanism before gluconeogenesis becomes dominant.
*Epinephrine-induced gluconeogenesis is the main process that allows for the compensation of a decreased glucose level.*
- While epinephrine promotes **gluconeogenesis**, it is not the *main* compensatory process in the *initial* stages of fasting (0-24 hours). **Glycogenolysis** is the primary response in the first few hours.
- Gluconeogenesis becomes the predominant source of glucose after glycogen stores are significantly depleted, typically after 24 hours of fasting or longer.
*There is an increase in the glycogen synthesis rate in this patient’s hepatocytes.*
- **Glycogen synthesis (glycogenesis)** occurs when blood glucose levels are high, typically after a meal, to store excess glucose as glycogen.
- In a state of hypoglycemia, the liver's priority is to *release* glucose, meaning **glycogenolysis** is increased, and glycogen synthesis is inhibited.
*The patient’s symptoms are most likely the consequence of increased insulin secretion from the pancreatic islets.*
- **Increased insulin secretion** would *cause* hypoglycemia, not be a consequence. In response to hypoglycemia, insulin secretion is *reduced* to prevent further lowering of blood glucose.
- The symptoms described (anxiety, sweating, trembling) are characteristic of the **adrenergic response** to hypoglycemia, mediated by epinephrine and norepinephrine, which are counter-regulatory hormones.
*The patient’s hypoglycemia inhibits glucagon release from pancreatic alpha cells.*
- **Hypoglycemia** is a strong stimulant for **glucagon release** from pancreatic alpha cells. Glucagon's primary role is to raise blood glucose levels by promoting hepatic glycogenolysis and gluconeogenesis.
- Therefore, glucagon release would be *stimulated*, not inhibited, in this patient's condition.
Environmental stress responses US Medical PG Question 7: A previously healthy 44-year-old man is brought by his coworkers to the emergency department 45 minutes after he became light-headed and collapsed while working in the boiler room of a factory. He did not lose consciousness. His coworkers report that 30 minutes prior to collapsing, he told them he was nauseous and had a headache. The patient appears sweaty and lethargic. He is not oriented to time, place, or person. The patient’s vital signs are as follows: temperature 41°C (105.8°F); heart rate 133/min; respiratory rate 22/min; and blood pressure 90/52 mm Hg. Examination shows equal and reactive pupils. Deep tendon reflexes are 2+ bilaterally. His neck is supple. A 0.9% saline infusion is administered. A urinary catheter is inserted and dark brown urine is collected. The patient’s laboratory test results are as follows:
Laboratory test
Blood
Hemoglobin 15 g/dL
Leukocyte count 18,000/mm3
Platelet count 51,000/mm3
Serum
Na+ 149 mEq/L
K+ 5.0 mEq/L
Cl- 98 mEq/L
Urea nitrogen 42 mg/dL
Glucose 88 mg/dL
Creatinine 1.8 mg/dL
Aspartate aminotransferase (AST, GOT) 210
Alanine aminotransferase (ALT, GPT) 250
Creatine kinase 86,000 U/mL
Which of the following is the most appropriate next step in patient management?
- A. Dantrolene
- B. Acetaminophen therapy
- C. Hemodialysis
- D. Ice water immersion (Correct Answer)
- E. Evaporative cooling
Environmental stress responses Explanation: ***Ice water immersion***
- This patient presents with signs and symptoms consistent with **heat stroke**, including high body temperature (41°C), altered mental status, and a history of working in a hot environment (boiler room). **Rapid aggressive cooling** is the most critical immediate intervention to prevent organ damage.
- **Ice water immersion** is the fastest and most effective cooling method for heat stroke, aiming to reduce core body temperature to less than 39°C (102.2°F) within 30 minutes.
*Dantrolene*
- **Dantrolene** is primarily used to treat **malignant hyperthermia** and **neuroleptic malignant syndrome**, conditions caused by abnormal calcium release in muscle cells, not environmental heat exposure.
- While both conditions involve hyperthermia, the underlying pathophysiology and triggers are different from heat stroke.
*Acetaminophen therapy*
- **Acetaminophen** is an antipyretic that works by inhibiting prostaglandin synthesis in the central nervous system, affecting the hypothalamic thermoregulatory center.
- It is **ineffective** for the hyperthermia seen in heat stroke, which is due to a failure of thermoregulation rather than an altered hypothalamic set point, and could potentially worsen liver injury.
*Hemodialysis*
- **Hemodialysis** is indicated for severe **renal failure**, drug overdose, or certain electrolyte imbalances. Although this patient has acute kidney injury (elevated BUN and creatinine, dark urine suggestive of rhabdomyolysis), aggressive cooling is the immediate life-saving intervention for heat stroke.
- While renal support might be necessary later if kidney injury progresses, it is not the most appropriate *initial* next step for hyperthermia and altered mental status.
*Evaporative cooling*
- **Evaporative cooling** (e.g., spraying with lukewarm water and using fans) is a cooling method that can be effective, particularly in environments with low humidity.
- However, for severe heat stroke with a temperature as high as 41°C, **ice water immersion** provides a more rapid and aggressive temperature reduction, which is crucial for improving outcomes.
Environmental stress responses US Medical PG Question 8: You have been asked to deliver a lecture to medical students about the effects of various body hormones and neurotransmitters on the metabolism of glucose. Which of the following statements best describes the effects of sympathetic stimulation on glucose metabolism?
- A. Norepinephrine causes increased glucose absorption within the intestines.
- B. Without epinephrine, insulin cannot act on the liver.
- C. Peripheral tissues require epinephrine to take up glucose.
- D. Epinephrine increases liver glycogenolysis. (Correct Answer)
- E. Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.
Environmental stress responses Explanation: ***Epinephrine increases liver glycogenolysis.***
- **Epinephrine**, released during sympathetic stimulation, primarily acts to increase **glucose availability** for immediate energy.
- It achieves this by stimulating **glycogenolysis** (breakdown of glycogen into glucose) in the liver via **beta-adrenergic receptors**.
*Norepinephrine causes increased glucose absorption within the intestines.*
- **Norepinephrine** primarily causes **vasoconstriction** and can *decrease* **intestinal motility** and nutrient absorption due to shunting blood away from the digestive tract during stress.
- Glucose absorption is mainly regulated by digestive enzymes and transport proteins, not directly increased by norepinephrine.
*Without epinephrine, insulin cannot act on the liver.*
- **Insulin** acts on the liver independent of epinephrine to promote **glucose uptake**, **glycogenesis**, and **lipid synthesis**.
- Epinephrine and insulin have **antagonistic effects** on liver glucose metabolism; epinephrine increases glucose output, while insulin decreases it.
*Peripheral tissues require epinephrine to take up glucose.*
- **Insulin** is the primary hormone required for **glucose uptake** by most peripheral tissues, especially **muscle** and **adipose tissue**, via **GLUT4 transporters**.
- Epinephrine generally *reduces* glucose uptake by peripheral tissues to preserve glucose for the brain during stress.
*Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.*
- Sympathetic stimulation, primarily acting through **alpha-2 adrenergic receptors** on pancreatic beta cells, actually **inhibits** **insulin secretion**.
- This inhibition helps to increase blood glucose levels by reducing insulin's glucose-lowering effects.
Environmental stress responses US Medical PG Question 9: A 28-year-old patient comes to the physician’s office with complaints of headaches and difficulty seeing out of the corner of her eye. She gave birth to her son 1 year ago. Further visual testing reveals the patient has bitemporal hemianopsia. The patient undergoes brain MRI which shows an anterior pituitary mass, likely adenoma. The patient has her blood tested to see if the adenoma is secreting extra hormone. The patient is found to have a slight excess of a hormone that uptakes a basophilic stain. Which of the following is most likely to be the hormone detected in her blood?
- A. Prolactin
- B. Growth hormone
- C. Thyroid stimulating hormone (Correct Answer)
- D. Antidiuretic hormone
- E. Oxytocin
Environmental stress responses Explanation: ***Thyroid stimulating hormone***
- **Thyroid-stimulating hormone (TSH)** is synthesized by **thyrotroph cells** which are basophilic, making it the most likely hormone to stain basophilically in this context.
- An excess of TSH from a pituitary adenoma could lead to clinical symptoms of **hyperthyroidism**, although the question states it's only a "slight excess."
*Prolactin*
- **Prolactin** is secreted by **lactotrophs**, which are acidophilic and would not take up a basophilic stain.
- While **prolactinomas** are the most common pituitary adenomas, their cells are not basophilic, and this patient does not exhibit common symptoms of hyperprolactinemia (galactorrhea, amenorrhea).
*Growth hormone*
- **Growth hormone (GH)** is produced by **somatotrophs**, which are acidophilic and would not take up a basophilic stain.
- Excess GH typically causes **acromegaly** in adults, characterized by distinctive physical changes not mentioned in the patient's presentation.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)**, also known as vasopressin, is synthesized in the **hypothalamus** and released from the posterior pituitary, not secreted by basophilic cells of the anterior pituitary.
- Overproduction of ADH leads to **SIADH**, characterized by hyponatremia and concentrated urine, none of which are described.
*Oxytocin*
- **Oxytocin** is also produced in the **hypothalamus** and released from the posterior pituitary, not by basophilic cells in the anterior pituitary.
- Its primary functions relate to uterine contractions and milk ejection and are not associated with pituitary adenomas causing bitemporal hemianopsia.
Environmental stress responses US Medical PG Question 10: A 42-year-old man undergoes therapeutic hypothermia (target temperature 33°C/91.4°F) following cardiac arrest with return of spontaneous circulation. During the cooling phase, he develops shivering, which increases oxygen consumption and interferes with target temperature achievement. He is already on sedation and neuromuscular blockade is being considered. Evaluate the most appropriate management strategy considering both efficacy and safety.
- A. Administer meperidine alone to reduce shivering threshold
- B. Increase sedation and add surface counter-warming of extremities before neuromuscular blockade (Correct Answer)
- C. Abandon therapeutic hypothermia due to complications
- D. Use only mechanical restraints to prevent movement
- E. Immediate neuromuscular blockade without additional measures
Environmental stress responses Explanation: ***Increase sedation and add surface counter-warming of extremities before neuromuscular blockade***
- A **stepwise approach** to shivering is preferred; increasing **sedation** and using **surface counter-warming** reduces the shivering threshold by tricking the hypothalamus into sensing a warmer periphery.
- This strategy minimizes the need for **neuromuscular blockade**, which can mask seizures and prevent accurate **neurological assessment**.
*Administer meperidine alone to reduce shivering threshold*
- While **meperidine** is an effective anti-shivering agent that lowers the shivering threshold, using it **alone** is often insufficient to control vigorous shivering during induction.
- Reliance on a single pharmacologic agent ignores the **multimodal therapy** benefits of physical measures like skin warming and optimized sedation.
*Abandon therapeutic hypothermia due to complications*
- Shivering is a predictable physiological response, not a reason to abandon **Targeted Temperature Management (TTM)**, which provides significant **neuroprotection** post-cardiac arrest.
- Stopping the therapy would deprive the patient of the benefit of reduced **cerebral metabolic rate** and improved survival outcomes.
*Use only mechanical restraints to prevent movement*
- Mechanical restraints are ineffective against the **metabolic consequences** of shivering, such as increased **oxygen consumption** and CO2 production.
- Shivering is a thermoregulatory reflex, and physical restraint does not stop the underlying **thermogenesis** or metabolic demand.
*Immediate neuromuscular blockade without additional measures*
- **Neuromuscular blockade** should be a last resort as it carries risks of **prolonged muscle weakness** and obscures the patient's clinical neurological status.
- It treats the muscular manifestation but lacks the **sedative or analgesic** properties needed to comfort the patient during the cooling process.
More Environmental stress responses US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.