Core body temperature maintenance US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Core body temperature maintenance. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Core body temperature maintenance US Medical PG Question 1: A 25-year-old man presents to the emergency department after a motor vehicle accident. He was the unrestrained front seat driver in a head on collision. The patient is unresponsive and his medical history is unknown. His temperature is 99.5°F (37.5°C), blood pressure is 67/38 mmHg, pulse is 190/min, respirations are 33/min, and oxygen saturation is 98% on room air. The patient is started on IV fluids, blood products, and norepinephrine. A FAST exam is performed and a pelvic binder is placed. One hour later, his temperature is 98.3°F (36.8°C), blood pressure is 119/66 mmHg, pulse is 110/min, respirations are 15/min, and oxygen saturation is 97% on room air. The patient is currently responsive. Management of the patient's pelvic fracture is scheduled by the orthopedic service. While the patient is waiting in the emergency department he suddenly complains of feeling hot, aches, and a headache. The patient's temperature is currently 101°F (38.3°C). He has not been given any pain medications and his past medical history is still unknown. Which of the following is the most likely diagnosis?
- A. Acute hemolytic transfusion reaction
- B. Febrile non-hemolytic transfusion reaction (Correct Answer)
- C. Sympathetic response to pain
- D. Minor blood group incompatibility
- E. Leukoagglutination reaction
Core body temperature maintenance Explanation: ***Febrile non-hemolytic transfusion reaction***
- This reaction is characterized by a **fever** and other constitutional symptoms (chills, headache, malaise) developing **within 4 hours of transfusion**, without evidence of hemolysis. The patient's symptoms and temperature rise after blood product administration fit this description.
- It is typically caused by antibodies in the recipient's plasma reacting with **leukocyte antigens** present on donor white blood cells or by **cytokines** released from donor leukocytes during storage.
*Acute hemolytic transfusion reaction*
- This reaction typically presents with more severe symptoms such as **hypotension**, **hemoglobinuria**, flank pain, and diffuse bleeding, indicating widespread intravascular hemolysis due to **ABO incompatibility**.
- Although the patient received blood products, his symptoms (feeling hot, aches, headache, mild fever) are not indicative of the severe, life-threatening nature of an acute hemolytic reaction.
*Sympathetic response to pain*
- While pain can cause a sympathetic response (tachycardia, hypertension), it typically does **not cause a fever** as seen in this patient.
- The patient's initial presentation included signs of shock, and after resuscitation, his vital signs normalized before the new symptoms appeared, suggesting a new process rather than ongoing pain alone.
*Minor blood group incompatibility*
- Reactions to minor blood group incompatibilities are usually **milder and delayed** compared to ABO incompatibilities.
- They often involve **extravascular hemolysis**, which might not present with the acute febrile reaction seen here, and are less common a cause of immediate febrile reactions.
*Leukoagglutination reaction*
- This is an older term for what is now often considered a type of **febrile non-hemolytic transfusion reaction (FNHTR)** caused by recipient antibodies to donor leukocyte antigens leading to leukocyte clumping.
- While related to FNHTR, the term "febrile non-hemolytic transfusion reaction" is the more encompassing and appropriate diagnosis given the typical symptom complex of fever, chills, and headache.
Core body temperature maintenance US Medical PG Question 2: A scientist is trying to design a drug to modulate cellular metabolism in the treatment of obesity. Specifically, he is interested in understanding how fats are processed in adipocytes in response to different energy states. His target is a protein within these cells that catalyzes catabolism of an energy source. The products of this reaction are subsequently used in gluconeogenesis or β-oxidation. Which of the following is true of the most likely protein that is being studied by this scientist?
- A. It is stimulated by epinephrine (Correct Answer)
- B. It is inhibited by glucagon
- C. It is inhibited by acetylcholine
- D. It is inhibited by cortisol
- E. It is stimulated by insulin
Core body temperature maintenance Explanation: ***It is stimulated by epinephrine***
- The protein described is likely **hormone-sensitive lipase (HSL)**, which catabolizes **triglycerides** in adipocytes to **glycerol** and **fatty acids**.
- **Epinephrine** (and norepinephrine) stimulates HSL activity via a **cAMP-dependent protein kinase A (PKA)** pathway, leading to increased fatty acid release for energy.
*It is inhibited by glucagon*
- **Glucagon primarily acts on the liver** to promote gluconeogenesis and glycogenolysis, but it does **not directly inhibit HSL** in adipocytes.
- While glucagon has a lipolytic effect, it doesn't inhibit the enzyme that releases fatty acids.
*It is inhibited by acetylcholine*
- **Acetylcholine** is a neurotransmitter involved in the **parasympathetic nervous system**, which generally promotes energy storage.
- It does **not directly inhibit HSL**; its effects on lipid metabolism are indirect and typically involve other pathways.
*It is inhibited by cortisol*
- **Cortisol**, a glucocorticoid, generally **promotes lipolysis** (breakdown of fats) in certain contexts, particularly during stress to provide energy substrates.
- Therefore, it would **not inhibit HSL**; rather, it often enhances its activity or provides a permissive effect for other lipolytic hormones.
*It is stimulated by insulin*
- **Insulin** is an **anabolic hormone** that promotes energy storage, including **lipogenesis** (fat synthesis) and inhibits lipolysis.
- Insulin **inhibits HSL activity** by activating phosphodiesterase, which reduces cAMP levels, thus deactivating PKA and preventing HSL phosphorylation.
Core body temperature maintenance US Medical PG Question 3: A 55-year-old woman with diabetes presents to the emergency department due to swelling of her left leg, fever, and chills for the past 2 days. The woman’s maximum recorded temperature at home was 38.3°C (101.0°F). Her left leg is red and swollen from her ankle to the calf, with an ill-defined edge. Her vital signs include: blood pressure 120/78 mm Hg, pulse rate 94/min, temperature 38.3°C (101.0°F), and respiratory rate 16/min. On physical examination, her left leg shows marked tenderness and warmth compared with her right leg. The left inguinal lymph node is enlarged to 3 x 3 cm. Which of the following chemical mediators is the most likely cause of the woman’s fever?
- A. Bradykinin
- B. Histamine
- C. PGE2 (Correct Answer)
- D. Arachidonic acid
- E. LTB4
Core body temperature maintenance Explanation: ***PGE2***
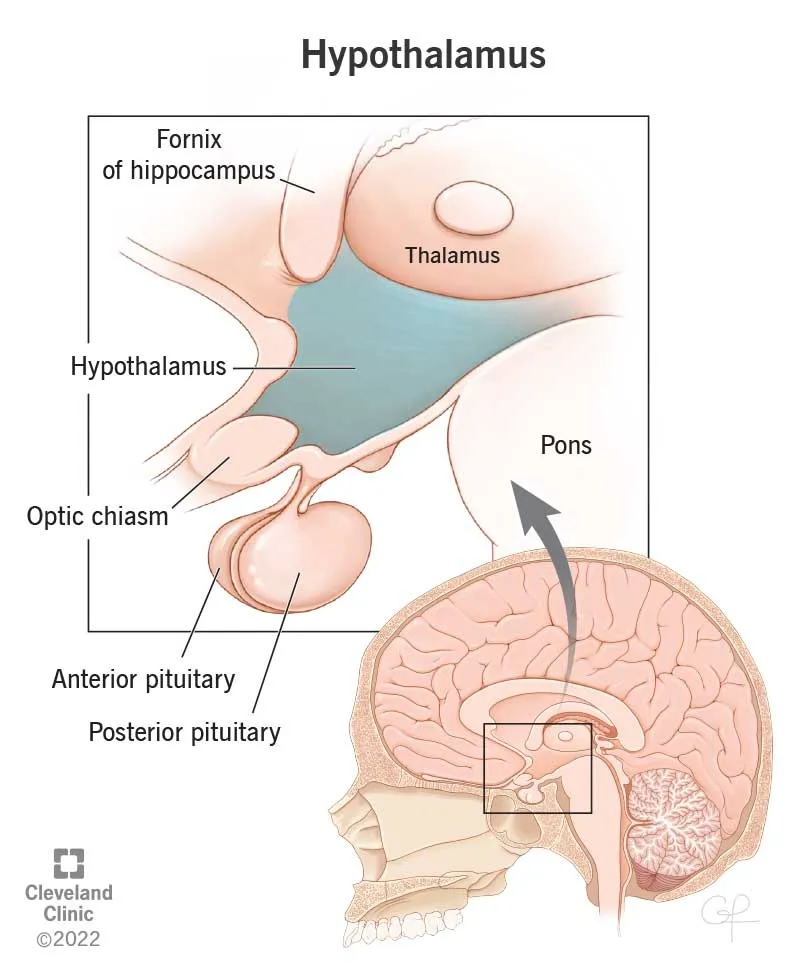
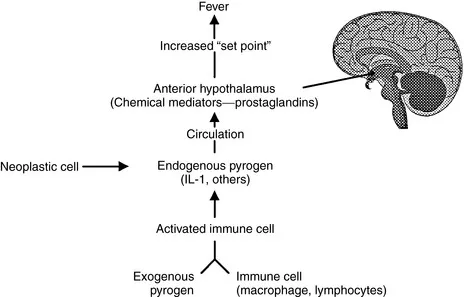
- **Prostaglandin E2 (PGE2)** is a potent **pyrogen** that acts on the **hypothalamus** to reset the body's thermoregulatory set point, leading to fever.
- In infections like **cellulitis**, inflammatory mediators stimulate the production of PGE2, causing the systemic symptom of fever.
*Bradykinin*
- **Bradykinin** primarily mediates **pain** and **vasodilation** at the site of inflammation.
- While it contributes to local signs of inflammation, it is not a direct mediator of systemic fever.
*Histamine*
- **Histamine** is a key mediator in immediate **hypersensitivity reactions** and local inflammation, causing **vasodilation** and increased **vascular permeability**.
- It does not directly induce fever by acting on the thermoregulatory center.
*Arachidonic acid*
- **Arachidonic acid** is a **precursor** molecule derived from membrane phospholipids, which is metabolized to various inflammatory mediators like prostaglandins and leukotrienes.
- It is not a direct chemical mediator of fever itself; rather, its downstream products such as PGE2 are.
*LTB4*
- **Leukotriene B4 (LTB4)** is a potent **chemotactic agent** for neutrophils, playing a role in immune cell recruitment to the site of inflammation.
- While involved in inflammation, LTB4 does not directly cause fever.
Core body temperature maintenance US Medical PG Question 4: A 3-day-old female newborn is brought to the emergency department because of fever, poor feeding, and irritability for 6 hours. She was delivered at home at 39 weeks' gestation and delivery was uncomplicated. The mother had no prenatal care. Her temperature is 39.8°C (103.6°F), pulse is 172/min, respirations are 58/min, and blood pressure is 74/45 mm Hg. She appears lethargic. Physical examination shows expiratory grunting and nasal flaring. Serum studies show elevated levels of interleukin-6. Which of the following is the most likely effect of this laboratory finding?
- A. Decreased synthesis of hepcidin
- B. Decreased expression of MHC class II
- C. Increased release of fibrinogen (Correct Answer)
- D. Increased classical activation of macrophages
- E. Increased production of IgE
Core body temperature maintenance Explanation: ***Increased release of fibrinogen***
- **Interleukin-6 (IL-6)** is a major **pro-inflammatory cytokine** that stimulates the liver to produce **acute phase reactants**, including **fibrinogen**.
- This increase in fibrinogen is part of the body's non-specific immune response to infection and inflammation, leading to elevated inflammatory markers like **ESR**.
*Decreased synthesis of hepcidin*
- **Hepcidin** synthesis is *increased* by IL-6, not decreased, as part of the body's response to inflammation to limit iron availability to pathogens.
- High levels of hepcidin lead to **anemia of chronic disease** by inhibiting iron absorption and release from macrophages.
*Decreased expression of MHC class II*
- IL-6 generally *enhances* immune responses, and while it doesn't directly increase MHC class II expression on antigen-presenting cells, reduced expression is not a typical effect.
- **MHC class II** expression is primarily regulated by cytokines like **interferon-gamma** and helps present antigens to T-helper cells.
*Increased classical activation of macrophages*
- **Classical activation of macrophages** (M1 polarization) is primarily driven by **interferon-gamma (IFN-γ)** and **TNF-α**, often in response to pathogen signals.
- While IL-6 can contribute to the overall inflammatory environment, it is not the primary cytokine for classical macrophage activation; rather, it often promotes alternative (M2) phenotypes or has pleiotropic effects.
*Increased production of IgE*
- **IgE production** is primarily associated with **allergic reactions** and **parasitic infections**, driven by cytokines like **IL-4** and **IL-13**.
- IL-6 is not directly involved in stimulating IgE synthesis; its main roles are in inflammation, hematopoiesis, and the acute phase response.
Core body temperature maintenance US Medical PG Question 5: An 11-year-old boy presents with a 2-day history of uncontrollable shivering. During admission, the patient’s vital signs are within normal limits, except for a fluctuating body temperature registering as low as 35.0°C (95.0°F) and as high as 40.0°C (104.0°F), requiring alternating use of cooling and warming blankets. A complete blood count (CBC) is normal, and a chest radiograph is negative for consolidations and infiltrates. An MRI of the brain reveals a space-occupying lesion infiltrating the posterior hypothalamus and extending laterally. Which of the following additional findings are most likely, based on this patient’s physical examination?
- A. Polyuria
- B. Hyperphagia
- C. Galactorrhea
- D. Sleep disturbances
- E. Anorexia (Correct Answer)
Core body temperature maintenance Explanation: **Anorexia**
- **Hypothalamic lesions**, particularly those affecting the **lateral hypothalamus**, often lead to **anorexia** and **weight loss** due to the role of this region in stimulating appetite.
- The patient's presentation with **uncontrollable shivering** and **deregulated body temperature** further points to hypothalamic dysfunction, which can also disrupt feeding centers.
*Polyuria*
- **Polyuria** is typically associated with damage to the **posterior pituitary gland** or its connections to the hypothalamus, leading to **diabetes insipidus** (lack of ADH).
- While a hypothalamic lesion can affect ADH production, the primary symptom constellation in this case more strongly suggests disruption of other hypothalamic functions.
*Hyperphagia*
- **Hyperphagia** (increased appetite) and **obesity** are most commonly linked to damage to the **ventromedial hypothalamus**, which is considered the satiety center.
- The presented lesion is described as infiltrating the posterior hypothalamus and extending laterally, making hyperphagia less likely than anorexia.
*Galactorrhea*
- **Galactorrhea** is often caused by **hyperprolactinemia**, which can result from lesions compressing the **pituitary stalk** or interfering with **dopamine's inhibitory effect** on prolactin release in the anterior pituitary.
- While a large hypothalamic lesion could theoretically impact pituitary function secondarily, galactorrhea is not a direct or most likely consequence of a posterior and lateral hypothalamic lesion.
*Sleep disturbances*
- While the **hypothalamus** plays a critical role in **sleep-wake cycles** (e.g., the **suprachiasmatic nucleus**), **uncontrollable shivering** and **poikilothermia** point more directly to acute disruption of temperature regulation rather than sleep disturbances as the most prominent likely additional finding.
- Many types of brain lesions can cause sleep disturbances, but the specific presentation here suggests a more particular set of hypothalamic dysfunctions.
Core body temperature maintenance US Medical PG Question 6: A 20-year-old woman reports to student health complaining of 5 days of viral symptoms including sneezing and a runny nose. She started coughing 2 days ago and is seeking cough medication. She additionally mentions that she developed a fever 2 days ago, but this has resolved. On exam, her temperature is 99.0°F (37.2°C), blood pressure is 118/76 mmHg, pulse is 86/min, and respirations are 12/min. Changes in the activity of warm-sensitive neurons in which part of her hypothalamus likely contributed to the development and resolution of her fever?
- A. Anterior hypothalamus (Correct Answer)
- B. Paraventricular nucleus
- C. Suprachiasmatic nucleus
- D. Lateral area
- E. Posterior hypothalamus
Core body temperature maintenance Explanation: ***Anterior hypothalamus***
- The **anterior hypothalamus** contains warm-sensitive neurons that detect increases in body temperature and activate mechanisms for heat dissipation, such as sweating and vasodilation.
- In fever, **prostaglandins** increase the set point in the anterior hypothalamus, causing the body to retain heat and increase heat production until the new set point is reached; resolution of fever involves resetting this set point back to normal.
*Paraventricular nucleus*
- The **paraventricular nucleus** is primarily involved in neuroendocrine functions, stress response, and the regulation of appetite and autonomic nervous system.
- It plays a significant role in releasing hormones like **corticotropin-releasing hormone (CRH)** and **oxytocin**, not direct temperature regulation.
*Suprachiasmatic nucleus*
- The **suprachiasmatic nucleus (SCN)** is the body's main biological clock, regulating **circadian rhythms** including the sleep-wake cycle and daily fluctuations in body temperature.
- While it influences the normal diurnal variation in body temperature, it is not directly responsible for the acute regulation of fever.
*Lateral area*
- The **lateral hypothalamus** primarily functions as the "hunger center," stimulating foraging and feeding behavior.
- Damage to this area can lead to **anorexia** and reduced food intake, not impairments in fever response.
*Posterior hypothalamus*
- The **posterior hypothalamus** is primarily involved in heat conservation and production mechanisms, such as shivering and vasoconstriction, in response to cold.
- It contains cold-sensitive neurons and functions to raise body temperature if it falls below the set point, but it is not where the set point itself is regulated in response to pyrogens.
Core body temperature maintenance US Medical PG Question 7: A 33-year-old man presents to the emergency department acutely confused. The patient was found down at a local construction site by his coworkers. The patient has a past medical history of a seizure disorder and schizophrenia and is currently taking haloperidol. He had recent surgery 2 months ago to remove an inflamed appendix. His temperature is 105°F (40.6°C), blood pressure is 120/84 mmHg, pulse is 150/min, respirations are 19/min, and oxygen saturation is 99% on room air. Physical exam is notable for a confused man who cannot answer questions. His clothes are drenched in sweat. He is not making purposeful movements with his extremities although no focal neurological deficits are clearly apparent. Which of the following is the most likely diagnosis?
- A. Heat exhaustion
- B. Nonexertional heat stroke
- C. Neuroleptic malignant syndrome
- D. Malignant hyperthermia
- E. Exertional heat stroke (Correct Answer)
Core body temperature maintenance Explanation: ***Exertional heat stroke***
- This diagnosis is supported by the patient's presentation of **hyperthermia** (105°F), **tachycardia**, **confusion**, and a history of working at a **construction site** (suggesting physical exertion in a hot environment).
- The patient's **drenched clothes from sweat** indicate the body's initial attempt to cool down, but the extremely high core temperature and confusion signify a failure of thermoregulation.
*Heat exhaustion*
- While heat exhaustion also involves **sweating** and can present with elevated body temperature, the core temperature is typically **below 104°F (40°C)**, and **marked altered mental status** (like severe confusion) is less common or less severe.
- The patient's temperature of 105°F (40.6°C) and profound confusion are more indicative of heat stroke.
*Nonexertional heat stroke*
- Nonexertional (or classic) heat stroke usually affects populations with **compromised thermoregulation** (e.g., elderly, very young, chronically ill) who are exposed to high environmental temperatures **without significant physical exertion**.
- The patient's age (33) and history of working at a construction site make exertional heat stroke more likely than nonexertional.
*Neuroleptic malignant syndrome*
- NMS is characterized by **fever, muscle rigidity** (often "lead pipe" rigidity), **altered mental status**, and **autonomic instability** (including tachycardia and diaphoresis), and is associated with **antipsychotic medications** like haloperidol.
- However, NMS typically develops **gradually over days to weeks**, not acutely. The key differentiator here is the **clear environmental and exertional context** (construction site work), **acute onset** after being found down, and the **absence of characteristic muscle rigidity** that would be prominent in NMS.
- Heat stroke is more probable given the immediate occupational exposure and clinical timeline.
*Malignant hyperthermia*
- Malignant hyperthermia is a rare, life-threatening condition associated with exposure to certain **anesthetic agents** (e.g., succinylcholine, volatile anesthetics) or, less commonly, severe exertion in susceptible individuals.
- The patient's recent surgery was two months prior, and there is no mention of current exposure to triggers, making it unlikely to be the immediate cause of his acute presentation.
Core body temperature maintenance US Medical PG Question 8: A previously healthy 44-year-old man is brought by his coworkers to the emergency department 45 minutes after he became light-headed and collapsed while working in the boiler room of a factory. He did not lose consciousness. His coworkers report that 30 minutes prior to collapsing, he told them he was nauseous and had a headache. The patient appears sweaty and lethargic. He is not oriented to time, place, or person. The patient’s vital signs are as follows: temperature 41°C (105.8°F); heart rate 133/min; respiratory rate 22/min; and blood pressure 90/52 mm Hg. Examination shows equal and reactive pupils. Deep tendon reflexes are 2+ bilaterally. His neck is supple. A 0.9% saline infusion is administered. A urinary catheter is inserted and dark brown urine is collected. The patient’s laboratory test results are as follows:
Laboratory test
Blood
Hemoglobin 15 g/dL
Leukocyte count 18,000/mm3
Platelet count 51,000/mm3
Serum
Na+ 149 mEq/L
K+ 5.0 mEq/L
Cl- 98 mEq/L
Urea nitrogen 42 mg/dL
Glucose 88 mg/dL
Creatinine 1.8 mg/dL
Aspartate aminotransferase (AST, GOT) 210
Alanine aminotransferase (ALT, GPT) 250
Creatine kinase 86,000 U/mL
Which of the following is the most appropriate next step in patient management?
- A. Dantrolene
- B. Acetaminophen therapy
- C. Hemodialysis
- D. Ice water immersion (Correct Answer)
- E. Evaporative cooling
Core body temperature maintenance Explanation: ***Ice water immersion***
- This patient presents with signs and symptoms consistent with **heat stroke**, including high body temperature (41°C), altered mental status, and a history of working in a hot environment (boiler room). **Rapid aggressive cooling** is the most critical immediate intervention to prevent organ damage.
- **Ice water immersion** is the fastest and most effective cooling method for heat stroke, aiming to reduce core body temperature to less than 39°C (102.2°F) within 30 minutes.
*Dantrolene*
- **Dantrolene** is primarily used to treat **malignant hyperthermia** and **neuroleptic malignant syndrome**, conditions caused by abnormal calcium release in muscle cells, not environmental heat exposure.
- While both conditions involve hyperthermia, the underlying pathophysiology and triggers are different from heat stroke.
*Acetaminophen therapy*
- **Acetaminophen** is an antipyretic that works by inhibiting prostaglandin synthesis in the central nervous system, affecting the hypothalamic thermoregulatory center.
- It is **ineffective** for the hyperthermia seen in heat stroke, which is due to a failure of thermoregulation rather than an altered hypothalamic set point, and could potentially worsen liver injury.
*Hemodialysis*
- **Hemodialysis** is indicated for severe **renal failure**, drug overdose, or certain electrolyte imbalances. Although this patient has acute kidney injury (elevated BUN and creatinine, dark urine suggestive of rhabdomyolysis), aggressive cooling is the immediate life-saving intervention for heat stroke.
- While renal support might be necessary later if kidney injury progresses, it is not the most appropriate *initial* next step for hyperthermia and altered mental status.
*Evaporative cooling*
- **Evaporative cooling** (e.g., spraying with lukewarm water and using fans) is a cooling method that can be effective, particularly in environments with low humidity.
- However, for severe heat stroke with a temperature as high as 41°C, **ice water immersion** provides a more rapid and aggressive temperature reduction, which is crucial for improving outcomes.
Core body temperature maintenance US Medical PG Question 9: You have been asked to deliver a lecture to medical students about the effects of various body hormones and neurotransmitters on the metabolism of glucose. Which of the following statements best describes the effects of sympathetic stimulation on glucose metabolism?
- A. Norepinephrine causes increased glucose absorption within the intestines.
- B. Without epinephrine, insulin cannot act on the liver.
- C. Peripheral tissues require epinephrine to take up glucose.
- D. Epinephrine increases liver glycogenolysis. (Correct Answer)
- E. Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.
Core body temperature maintenance Explanation: ***Epinephrine increases liver glycogenolysis.***
- **Epinephrine**, released during sympathetic stimulation, primarily acts to increase **glucose availability** for immediate energy.
- It achieves this by stimulating **glycogenolysis** (breakdown of glycogen into glucose) in the liver via **beta-adrenergic receptors**.
*Norepinephrine causes increased glucose absorption within the intestines.*
- **Norepinephrine** primarily causes **vasoconstriction** and can *decrease* **intestinal motility** and nutrient absorption due to shunting blood away from the digestive tract during stress.
- Glucose absorption is mainly regulated by digestive enzymes and transport proteins, not directly increased by norepinephrine.
*Without epinephrine, insulin cannot act on the liver.*
- **Insulin** acts on the liver independent of epinephrine to promote **glucose uptake**, **glycogenesis**, and **lipid synthesis**.
- Epinephrine and insulin have **antagonistic effects** on liver glucose metabolism; epinephrine increases glucose output, while insulin decreases it.
*Peripheral tissues require epinephrine to take up glucose.*
- **Insulin** is the primary hormone required for **glucose uptake** by most peripheral tissues, especially **muscle** and **adipose tissue**, via **GLUT4 transporters**.
- Epinephrine generally *reduces* glucose uptake by peripheral tissues to preserve glucose for the brain during stress.
*Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.*
- Sympathetic stimulation, primarily acting through **alpha-2 adrenergic receptors** on pancreatic beta cells, actually **inhibits** **insulin secretion**.
- This inhibition helps to increase blood glucose levels by reducing insulin's glucose-lowering effects.
Core body temperature maintenance US Medical PG Question 10: An investigator is conducting a study on hematological factors that affect the affinity of hemoglobin for oxygen. An illustration of two graphs (A and B) that represent the affinity of hemoglobin for oxygen is shown. Which of the following best explains a shift from A to B?
- A. Decreased serum pCO2
- B. Increased serum pH
- C. Decreased serum 2,3-bisphosphoglycerate concentration
- D. Increased body temperature (Correct Answer)
- E. Increased hemoglobin γ-chain synthesis
Core body temperature maintenance Explanation: ***Increased body temperature***
- A shift from A to B represents a **rightward shift** of the oxygen-hemoglobin dissociation curve, indicating **decreased hemoglobin affinity for oxygen**.
- **Increased body temperature** (e.g., during exercise, fever) reduces hemoglobin's affinity for oxygen, facilitating **oxygen release to tissues**.
*Decreased serum pCO2*
- A **decrease in serum pCO2** leads to an **increase in pH** (alkalosis) and a **leftward shift** of the curve, meaning an increased affinity of hemoglobin for oxygen.
- This is part of the **Bohr effect**, where lower CO2 levels signal decreased tissue metabolic activity, thus reducing oxygen unloading.
*Increased serum pH*
- An **increase in serum pH** (alkalosis) causes a **leftward shift** of the oxygen-hemoglobin dissociation curve, signifying **increased hemoglobin affinity for oxygen**.
- This response is beneficial in the lungs, where higher pH promotes oxygen binding to hemoglobin.
*Decreased serum 2,3-bisphosphoglycerate concentration*
- A **decrease in 2,3-BPG** concentration leads to a **leftward shift** of the curve, representing **increased hemoglobin affinity for oxygen**.
- 2,3-BPG typically binds to deoxyhemoglobin, stabilizing its T-state and promoting oxygen release; thus, less 2,3-BPG means less release.
*Increased hemoglobin γ-chain synthesis*
- Increased **hemoglobin γ-chain synthesis** is characteristic of **fetal hemoglobin (HbF)**, which has a **higher affinity for oxygen** than adult hemoglobin (HbA).
- This would result in a **leftward shift** of the oxygen-hemoglobin dissociation curve, enhancing oxygen uptake by the fetus.
More Core body temperature maintenance US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.