Temperature regulation

On this page
🌡️ The Hypothalamic Command Center: Your Body's Precision Thermostat
Your body maintains its core temperature within a razor-thin 0.6°C range despite facing arctic cold and desert heat-a feat of biological engineering that rivals any climate control system. You'll discover how the hypothalamus orchestrates heat production through shivering and metabolism, deploys cooling mechanisms from vasodilation to sweating, and integrates these responses through precise neural networks. We'll then translate this physiology into clinical reality: recognizing when regulation fails in fever, hypothermia, and heat stroke, and mastering the therapeutic interventions that can save lives when temperature goes dangerously wrong.
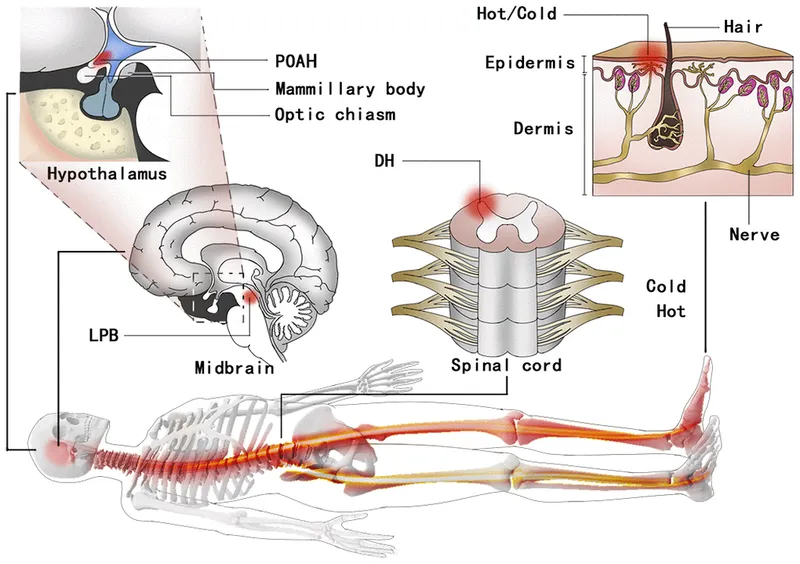
The preoptic anterior hypothalamus (POAH) serves as the primary thermoregulatory center, containing both warm-sensitive and cold-sensitive neurons. Warm-sensitive neurons increase firing rates by 10-fold when temperature rises just 1°C, while cold-sensitive neurons demonstrate the opposite response pattern.
📌 Remember: POAH - Primary Orchestrator of All Heat regulation, containing 80% of temperature-sensitive neurons in the brain
-
Central Thermoreceptors (Hypothalamic)
- Located primarily in POAH (80% of brain's thermosensitive neurons)
- Warm-sensitive neurons: increase firing 10x per 1°C rise
- Cold-sensitive neurons: decrease firing with temperature elevation
- Ratio warm:cold neurons = 3:1 in healthy adults
- Response time: <30 seconds to temperature changes
-
Peripheral Thermoreceptors (Skin and Deep Tissues)
- Skin thermoreceptors: 30,000+ cold vs 3,000 warm receptors
- Deep tissue sensors in spinal cord, abdomen, great vessels
- Provide 25% of thermal input to hypothalamus
- Critical for anticipatory responses to environmental changes
| Thermoreceptor Type | Location | Density | Response Time | Temperature Range | Clinical Significance |
|---|---|---|---|---|---|
| Cold (peripheral) | Skin surface | 30,000+ | 0.1-0.5 sec | 10-40°C | Immediate behavioral responses |
| Warm (peripheral) | Skin surface | 3,000 | 0.2-1.0 sec | 30-45°C | Heat stress detection |
| Central warm | POAH | 80% of CNS | <30 sec | 36-42°C | Core temperature regulation |
| Central cold | POAH | 20% of CNS | <30 sec | 35-39°C | Metabolic heat production |
| Deep tissue | Viscera/spine | Variable | 1-5 sec | 35-40°C | Anticipatory adjustments |
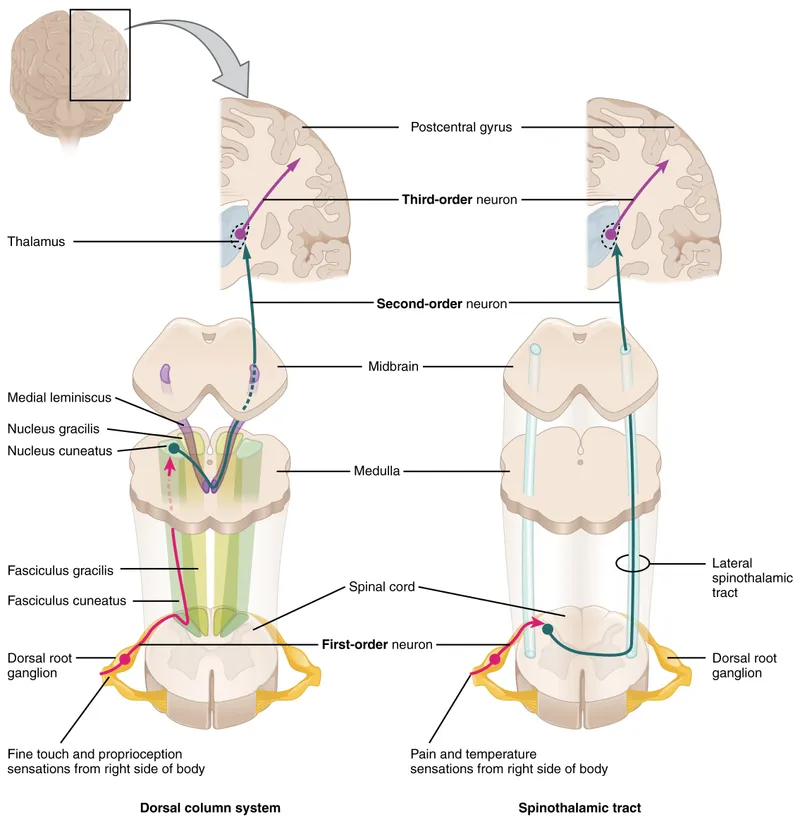
The integration of thermal signals occurs through ascending spinothalamic pathways that relay peripheral information to the hypothalamus within 100-500 milliseconds. This rapid processing enables anticipatory responses before core temperature actually changes.
💡 Master This: The 3:1 ratio of warm-to-cold sensitive neurons in POAH explains why heat detection is more sensitive than cold detection, protecting against hyperthermia which is more immediately life-threatening than mild hypothermia.
Understanding thermoreceptor distribution and hypothalamic integration provides the foundation for recognizing how fever resets the thermostat and why certain medications disrupt temperature regulation.
🌡️ The Hypothalamic Command Center: Your Body's Precision Thermostat
🔥 Heat Production Arsenal: Metabolic Furnaces and Muscle Generators
📌 Remember: SHIVER - Skeletal muscle Heat Increases Very Effectively, Raising metabolism 5x baseline within 60 seconds
-
Shivering Thermogenesis (Rapid Response)
- Onset time: 30-60 seconds after cold exposure
- Peak heat production: 400-500 watts (5x baseline)
- Efficiency: 100% conversion to heat (no mechanical work)
- Involves Type I and IIa muscle fibers primarily
- Frequency: 10-20 Hz muscle contractions
- Duration limit: 2-4 hours before fatigue
-
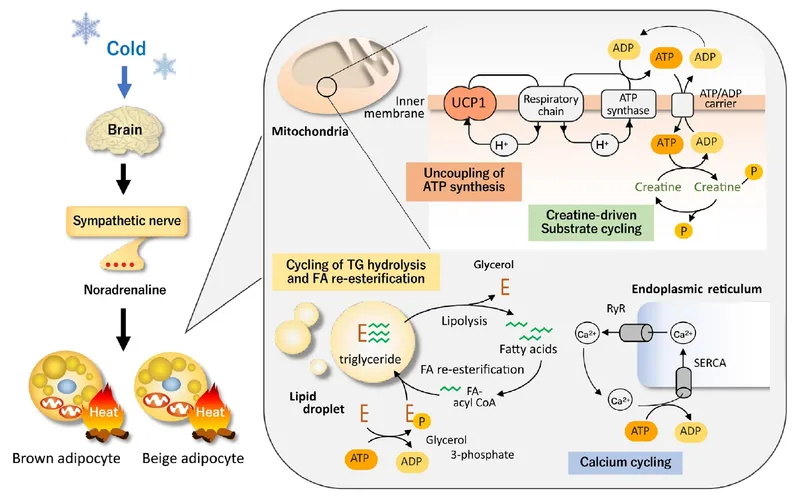
Non-Shivering Thermogenesis (Sustained Response)
- Brown adipose tissue (BAT) activation via sympathetic stimulation
- Heat production: 50-100 watts additional
- UCP1 protein uncouples oxidative phosphorylation
- Peak response: 2-4 hours after cold exposure
- Capacity: 300-500g BAT in healthy adults
| Heat Production Method | Response Time | Peak Output | Duration | Efficiency | Primary Trigger |
|---|---|---|---|---|---|
| Shivering | 30-60 sec | 400-500W | 2-4 hours | 100% | Skin cold receptors |
| Brown fat (BAT) | 2-4 hours | 50-100W | Days-weeks | 85% | Sympathetic activation |
| Voluntary exercise | Immediate | 300-800W | Variable | 25% | Behavioral response |
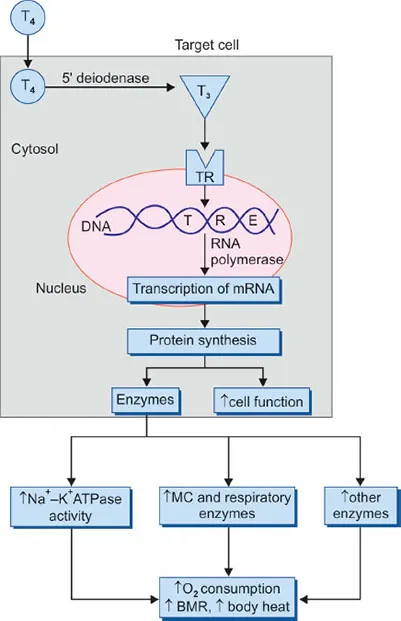
| Thyroid stimulation | 24-48 hours | 20-30W | Weeks | 90% | TSH/T3/T4 elevation |
| Basal metabolism | Continuous | 80-100W | Constant | 95% | Cellular respiration |
Hormonal Heat Production involves thyroid hormone upregulation, increasing Na+/K+-ATPase activity and protein synthesis. This mechanism provides 20-30% increase in basal metabolic rate over 24-48 hours, representing the body's long-term adaptation to cold environments.
💡 Master This: Shivering provides immediate high-intensity heat (5x baseline) but fatigues quickly, while brown fat offers sustained moderate heat production (1.5x baseline) for prolonged cold exposure.
The sympathetic nervous system coordinates both shivering and non-shivering responses through norepinephrine release, which stimulates β3-adrenergic receptors in brown fat and α-motor neurons controlling skeletal muscle. This dual activation explains why beta-blockers can impair cold tolerance.
Heat production mechanisms provide the foundation for understanding fever pathophysiology and therapeutic hypothermia protocols used in critical care settings.
🔥 Heat Production Arsenal: Metabolic Furnaces and Muscle Generators
❄️ Heat Dissipation Networks: The Body's Cooling Infrastructure
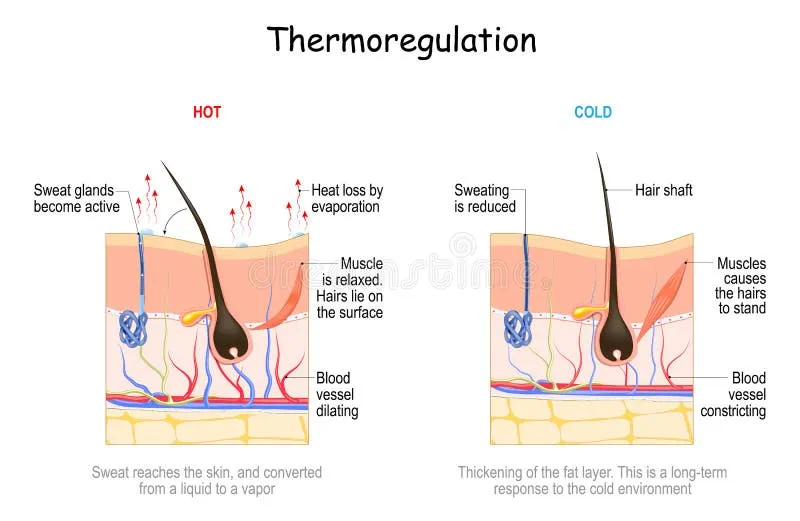
-
Radiation (Electromagnetic Heat Transfer)
- Accounts for 60% of heat loss at rest in 20°C environment
- Effectiveness decreases when ambient temperature >32°C
- Stefan-Boltzmann law: Heat loss ∝ (T₁⁴ - T₂⁴)
- Skin temperature: 33-34°C vs ambient 20-25°C
- Heat transfer rate: 40-60 watts/m² body surface
-
Convection (Air Movement Heat Transfer)
- Contributes 15-20% of heat loss at rest
- Effectiveness increases with air movement: 2x at 1 m/s wind
- Natural convection: 5-10 watts/m²
- Forced convection: 20-40 watts/m² with fan
📌 Remember: RACE - Radiation And Convection Eliminate most heat when cool, Evaporation essential when hot
| Heat Loss Mechanism | % at Rest (20°C) | % During Exercise | Environmental Limit | Max Capacity | Control Method |
|---|---|---|---|---|---|
| Radiation | 60% | 15% | Ambient <32°C | 60 W/m² | Vasodilation |
| Convection | 20% | 10% | Air movement | 40 W/m² | Vasodilation |
| Evaporation | 15% | 70% | Humidity <100% | 600 W/m² | Sweating |
| Conduction | 5% | 5% | Surface contact | 100 W/m² | Behavior |
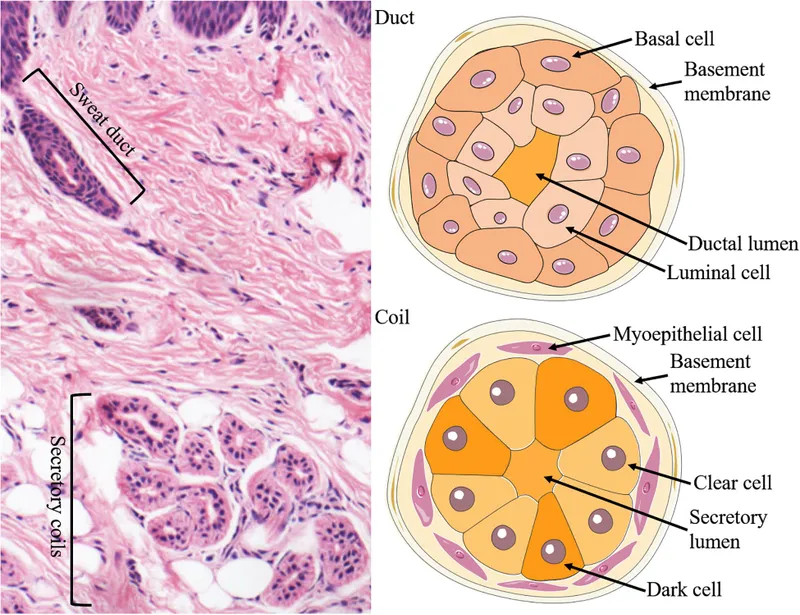
- Sweating Capacity and Regulation
- Maximum sweat rate: 2-3 liters/hour in acclimatized individuals
- Heat removal potential: 1,400-2,100 watts at maximum sweating
- Eccrine glands: 2-4 million distributed across body surface
- Highest density: 400-500/cm² on palms and soles
- Sympathetic cholinergic innervation via acetylcholine
- Response time: 30-60 seconds after thermal stimulus
⭐ Clinical Pearl: Heat stroke occurs when evaporative cooling fails and core temperature exceeds 40°C. Mortality risk increases 13% for every 1°C above 40°C without immediate cooling.
Cardiovascular Adjustments for heat dissipation involve massive redistribution of blood flow from splanchnic circulation to cutaneous vessels. Skin blood flow can increase from 200-300 mL/min at rest to 6-8 L/min during heat stress.
- Vascular Heat Transfer Mechanisms
- Arteriovenous anastomoses in hands, feet, ears
- Countercurrent heat exchange in extremities
- Venous return temperature: 2-3°C cooler than arterial
- Heat conservation efficiency: 85-90% in cold conditions
💡 Master This: When ambient temperature exceeds 32°C, evaporation becomes the only effective heat loss mechanism, making humidity the critical environmental factor determining heat tolerance.
Understanding heat dissipation mechanisms reveals why anticholinergic medications (atropine, antihistamines) increase heat stroke risk by blocking sweat production, and why dehydration impairs both sweating and cardiovascular heat transfer.
❄️ Heat Dissipation Networks: The Body's Cooling Infrastructure
🎯 Thermoregulatory Integration: The Neural Command Network
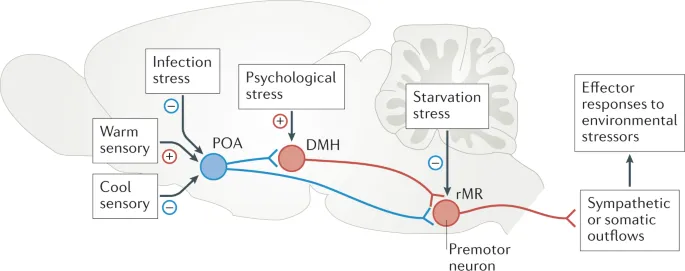
-
Hypothalamic Control Centers
- Preoptic Anterior Hypothalamus (POAH): Primary integration center
- Posterior Hypothalamus: Heat production coordination
- Paraventricular Nucleus: Autonomic output control
- Warm-sensitive neurons: 3:1 ratio over cold-sensitive
- Integration time constant: 10-30 seconds
- Set-point precision: ±0.1°C under normal conditions
-
Neural Pathway Integration
- Ascending pathways: Spinothalamic tract → POAH (100-500 ms delay)
- Descending pathways: Hypothalamus → sympathetic preganglionic neurons
- Sympathetic outflow: Controls vasoconstriction, sweating, shivering
- Parasympathetic modulation: Fine-tunes cardiovascular responses
📌 Remember: POAH - Processes Overall Automatic Heat control with 3:1 warm-to-cold neuron ratio for heat-sensitive protection
| Control System Component | Response Time | Precision | Temperature Range | Primary Function | Clinical Relevance |
|---|---|---|---|---|---|
| POAH integration | 10-30 sec | ±0.1°C | 36-38°C | Set-point control | Fever mechanisms |
| Sympathetic outflow | 1-5 sec | ±0.2°C | 35-40°C | Effector activation | Drug interactions |
| Behavioral responses | 0.1-1 sec | ±1.0°C | 10-45°C | Conscious actions | Cognitive impairment |
| Hormonal modulation | 1-24 hours | ±0.5°C | 35-39°C | Long-term adaptation | Endocrine disorders |
| Spinal reflexes | 0.1-0.5 sec | ±2.0°C | 0-50°C | Emergency responses | Spinal cord injury |
⭐ Clinical Pearl: Antipyretic medications (acetaminophen, NSAIDs) work by blocking PGE₂ synthesis, not by enhancing heat loss mechanisms. This explains why they're ineffective in heat stroke where set-point remains normal.
Circadian Temperature Rhythm demonstrates ±1°C variation over 24 hours, with lowest temperatures at 4-6 AM (36.1°C) and highest at 4-8 PM (37.2°C). This rhythm persists even during fever, with the entire curve shifted upward.
- Circadian Integration Mechanisms
- Suprachiasmatic nucleus provides timing signals to POAH
- Melatonin and cortisol modulate temperature set-point
- Temperature nadir: 4-6 AM (↓0.5-1.0°C from mean)
- Temperature peak: 4-8 PM (↑0.5-1.0°C from mean)
- Rhythm amplitude: ±0.5°C in healthy adults
💡 Master This: The 3:1 warm-to-cold neuron ratio in POAH creates asymmetric responses - heat detection is 3x more sensitive than cold detection, providing evolutionary protection against lethal hyperthermia.
Thermoregulatory integration explains why anesthesia disrupts temperature control (blocks neural integration), why spinal cord injuries above T6 impair thermoregulation (interrupts descending pathways), and why alcohol causes heat loss (vasodilation without appropriate behavioral responses).
🎯 Thermoregulatory Integration: The Neural Command Network
🔬 Clinical Temperature Disorders: Pathophysiology and Recognition Patterns
- Fever vs. Hyperthermia (Critical Distinction)
- Fever: Set-point elevation with intact thermoregulation
- Hyperthermia: Normal set-point with failed heat dissipation
- Fever: Shivering during temperature rise phase
- Hyperthermia: No shivering, immediate heat loss attempts
- Fever: Responds to antipyretics (PGE₂ blockade)
- Hyperthermia: No response to antipyretics, requires external cooling
📌 Remember: FEVER - Feel cold initially, Elevated set-point, Vasodilation later, Effective antipyretics, Responds to cooling
| Temperature Disorder | Core Temp | Set-Point | Shivering | Sweating | Antipyretic Response | Mortality Risk |
|---|---|---|---|---|---|---|
| Mild fever | 37.5-38.5°C | Elevated | During rise | During fall | Effective | <1% |
| High fever | 38.5-41°C | Elevated | During rise | During fall | Effective | 5-15% |
| Heat exhaustion | 37-40°C | Normal | Absent | Profuse | None | 1-5% |
| Heat stroke | >40°C | Normal | Absent | Absent/minimal | None | 20-70% |
| Malignant hyperthermia | >38.5°C | Normal | Muscle rigidity | Variable | None | 80% untreated |
- Heat Stroke Recognition Criteria
- Core temperature >40°C (104°F)
- Central nervous system dysfunction (confusion, seizures, coma)
- Hot, dry skin (classic) or hot, sweaty skin (exertional)
- Classic heat stroke: Elderly, medications, environmental
- Exertional heat stroke: Young athletes, high humidity
- Mortality: 13% increase per 1°C above 40°C
⭐ Clinical Pearl: Anhidrosis (absent sweating) in heat stroke indicates complete thermoregulatory failure. However, 25% of exertional heat stroke patients continue sweating, making CNS dysfunction the key diagnostic criterion.
Hypothermia Classification based on core temperature correlates with specific physiological responses and survival probability:
- Hypothermia Staging System
- Mild: 32-35°C - Shivering, vasoconstriction, tachycardia
- Moderate: 28-32°C - Shivering stops, bradycardia, confusion
- Severe: <28°C - Cardiac arrhythmias, coma, apparent death
- Shivering cessation: 32°C (muscle glycogen depletion)
- Cardiac instability: <30°C (ventricular fibrillation risk)
- Survival limit: 13.7°C (lowest recorded survival)
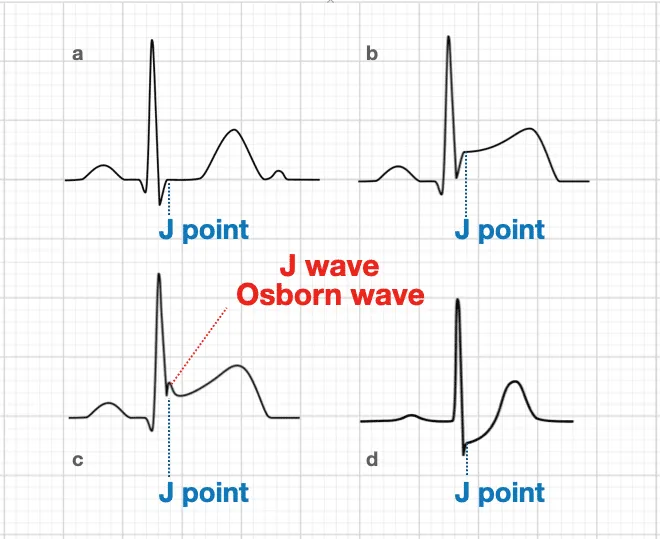
💡 Master This: Osborn J waves appear on ECG when core temperature drops below 32°C, representing delayed ventricular repolarization. J wave amplitude increases as temperature decreases, serving as a non-invasive temperature indicator.
Drug-Induced Temperature Disorders result from interference with specific thermoregulatory mechanisms:
- Hyperthermia-Inducing Medications
- Anticholinergics: Block sweating (atropine, antihistamines)
- Sympathomimetics: Increase heat production (amphetamines, cocaine)
- Serotonin syndrome: 5-HT excess causing muscle rigidity
- Temperature rise: 1-2°C per hour in severe cases
- Mortality: 10-15% without immediate treatment
Understanding clinical temperature disorders enables rapid recognition of thermoregulatory emergencies and guides appropriate cooling or rewarming strategies based on underlying pathophysiology.
🔬 Clinical Temperature Disorders: Pathophysiology and Recognition Patterns
🌡️ Therapeutic Temperature Management: Precision Control Strategies

- Therapeutic Hypothermia Protocols
- Target temperature: 32-34°C for 12-24 hours
- Cooling rate: 1-2°C per hour to prevent complications
- Rewarming rate: 0.25-0.5°C per hour (slower than cooling)
- Neuroprotection mechanism: ↓cerebral metabolism 6-7% per 1°C
- Oxygen consumption: ↓50% at 32°C vs 37°C
- Survival benefit: 15-20% improvement in cardiac arrest
📌 Remember: COOL - Cerebral metabolism ↓6% per degree, Oxygen needs ↓50% at 32°C, Outcome improves 15-20%, Low and slow rewarming
| Cooling Method | Cooling Rate | Precision | Complications | Cost | Clinical Use |
|---|---|---|---|---|---|
| Surface cooling | 0.5-1°C/h | ±1°C | Shivering, skin injury | Low | General wards |
| Intravascular | 1-3°C/h | ±0.2°C | Infection, thrombosis | High | ICU only |
| Peritoneal lavage | 2-4°C/h | ±0.5°C | Perforation risk | Medium | Emergency |
| Extracorporeal | 3-5°C/h | ±0.1°C | Bleeding, complexity | Very high | Specialized centers |
| Evaporative | 1-2°C/h | ±1°C | Dehydration | Low | Heat stroke |
- Aggressive Cooling Techniques
- Ice water immersion: 0.15-0.35°C/min cooling rate
- Evaporative cooling: 0.31°C/min with fans and misting
- Cold IV fluids: 1-2°C reduction with 30 mL/kg cold saline
- Target: Core temperature <39°C within 30 minutes
- Monitoring: Continuous core temperature (esophageal/rectal)
- Endpoint: 38.5°C to prevent overshoot hypothermia
⭐ Clinical Pearl: Ice water immersion provides fastest cooling (0.35°C/min) but may cause peripheral vasoconstriction that impairs heat transfer. Massage extremities during immersion to maintain circulation.
Pharmacological Temperature Management involves medications that either enhance or impair thermoregulatory responses:
-
Shivering Suppression (During Therapeutic Hypothermia)
- Meperidine: 0.5-1 mg/kg - blocks shivering at α₂ receptors
- Dexmedetomidine: 0.2-0.7 μg/kg/h - central α₂ agonist
- Neuromuscular blockade: Vecuronium for refractory shivering
- Shivering increases heat production 2-5x baseline
- Counteracts cooling efforts and increases oxygen consumption
-
Fever Reduction Mechanisms
- Acetaminophen: Blocks COX-3 in hypothalamus (PGE₂ ↓)
- NSAIDs: Block COX-1/2 peripherally and centrally
- Dose: Acetaminophen 15 mg/kg q6h (max 4g/day)
- Onset: 30-60 minutes for temperature reduction
- Duration: 4-6 hours therapeutic effect
💡 Master This: Therapeutic hypothermia requires active shivering suppression because shivering can generate 200-400 watts of heat, completely counteracting external cooling efforts.
Temperature Monitoring Precision becomes critical during therapeutic interventions, with core temperature sites providing different accuracy levels:
- Core Temperature Measurement Sites
- Pulmonary artery: Gold standard (±0.1°C)
- Esophageal: ±0.2°C (preferred for procedures)
- Bladder: ±0.3°C (requires adequate urine flow)
- Avoid: Oral (±1°C), axillary (±2°C), temporal (±1.5°C)
- Update frequency: Continuous during active cooling/warming
Understanding therapeutic temperature management enables evidence-based protocols for neuroprotection, heat stroke treatment, and perioperative hypothermia prevention while minimizing complications through precise physiological control.
🌡️ Therapeutic Temperature Management: Precision Control Strategies
🎯 Temperature Regulation Mastery: Clinical Command Arsenal
📌 Remember: TEMP - Thermostat location (hypothalamus), Effectors (shiver/sweat), Mechanisms (4 heat loss), Pathology patterns (fever vs hyperthermia)
-
Essential Clinical Thresholds
- Normal core range: 36.1-37.2°C (circadian variation ±0.5°C)
- Fever definition: >38°C oral, >38.3°C rectal
- Hypothermia stages: Mild 32-35°C, Moderate 28-32°C, Severe <28°C
- Heat stroke threshold: >40°C + CNS dysfunction
- Therapeutic hypothermia: 32-34°C for 12-24 hours
- Shivering cessation: 32°C (muscle glycogen depletion)
-
Rapid Diagnostic Framework
- Fever: Shivering → elevated set-point → responds to antipyretics
- Hyperthermia: No shivering → normal set-point → external cooling only
- Heat stroke: >40°C + altered mental status + hot skin
- Drug fever: 38-40°C + medication history + no other source
- Malignant hyperthermia: Muscle rigidity + CO₂ ↑ + CK ↑
| Clinical Scenario | Core Temp | Key Features | Immediate Action | Mortality Risk | Time Sensitivity |
|---|---|---|---|---|---|
| Septic fever | 38-41°C | Shivering, responds to antipyretics | Blood cultures, antibiotics | Variable | Hours |
| Heat stroke | >40°C | CNS dysfunction, hot skin | Aggressive cooling | 20-70% | Minutes |
| Hypothermia severe | <28°C | No shivering, J waves | Gentle rewarming | 50-80% | Hours |
| Malignant hyperthermia | >38.5°C | Muscle rigidity, high CO₂ | Dantrolene 2.5 mg/kg | 80% untreated | Minutes |
| Drug hyperthermia | 38-42°C | Medication history, rigidity | Stop drug, cooling | 10-15% | Hours |
Emergency Cooling Protocols prioritize speed and safety based on underlying pathophysiology:
- Heat Stroke Cooling Algorithm
- Target: <39°C within 30 minutes
- Method: Ice water immersion (0.35°C/min) or evaporative cooling
- Monitoring: Continuous core temperature + neurological status
- Stop cooling at 38.5°C to prevent overshoot
- Massage extremities during ice immersion
- Avoid antipyretics (ineffective, may mask progress)
💡 Master This: Shivering presence distinguishes fever (intact thermoregulation) from hyperthermia (failed heat dissipation), determining whether antipyretics or external cooling will be effective.
High-Yield Clinical Correlations connect thermoregulatory physiology to common clinical scenarios:
- Medication Effects on Thermoregulation
- Anticholinergics: Block sweating → heat stroke risk
- Beta-blockers: Impair shivering → hypothermia risk
- Anesthetics: Disrupt hypothalamic integration → perioperative hypothermia
- Elderly patients: ↓muscle mass, ↓brown fat → poor temperature control
- Spinal cord injury: Disrupted autonomic pathways → poikilothermia
- Thyroid disorders: Altered metabolic rate → temperature instability
This clinical mastery framework transforms thermoregulatory knowledge into diagnostic precision, therapeutic effectiveness, and improved patient outcomes across emergency medicine, critical care, and perioperative settings.
🎯 Temperature Regulation Mastery: Clinical Command Arsenal
Practice Questions: Temperature regulation
Test your understanding with these related questions
A 37-year-old man with a history of schizophrenia, obesity, anxiety, recurrent pneumonia, and depression is brought to the emergency department. He was recently discharged from inpatient psychiatric care where he was treated for an acute psychotic episode with fluphenazine and started on a new antidepressant. One week after discharge, during a period of cold weather, he is found outdoors confused and poorly dressed. His rectal temperature is 93.2°F (34°C). Which of the following medications is most likely contributing to his hypothermia?













