Sleep effects on respiration US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sleep effects on respiration. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sleep effects on respiration US Medical PG Question 1: Which of the following physiologic changes decreases pulmonary vascular resistance (PVR)?
- A. Inhaling the inspiratory reserve volume (IRV)
- B. Exhaling the entire vital capacity (VC)
- C. Exhaling the expiratory reserve volume (ERV)
- D. Breath holding maneuver at functional residual capacity (FRC)
- E. Inhaling the entire vital capacity (VC) (Correct Answer)
Sleep effects on respiration Explanation: ***Inhaling the entire vital capacity (VC)***
- As lung volume increases from FRC to TLC (which includes inhaling the entire VC), alveolar vessels are **stretched open**, and extra-alveolar vessels are **pulled open** by the increased radial traction, leading to a decrease in PVR.
- This **maximizes the cross-sectional area** of the pulmonary vascular bed, lowering resistance.
*Inhaling the inspiratory reserve volume (IRV)*
- While inhaling IRV increases lung volume, it's not the maximal inspiration of the entire VC where **PVR is typically at its lowest**.
- PVR continues to decrease as lung volume approaches total lung capacity (TLC).
*Exhaling the entire vital capacity (VC)*
- Exhaling the entire vital capacity leads to very low lung volumes, where PVR significantly **increases**.
- At low lung volumes, **alveolar vessels become compressed** and extra-alveolar vessels **narrow**, increasing resistance.
*Exhaling the expiratory reserve volume (ERV)*
- Exhaling the ERV results in a lung volume below FRC, which causes a **marked increase in PVR**.
- This is due to the **compression of alveolar vessels** and decreased radial traction on extra-alveolar vessels.
*Breath holding maneuver at functional residual capacity (FRC)*
- At FRC, the PVR is at an **intermediate level**, not its lowest.
- This is the point where the opposing forces affecting alveolar and extra-alveolar vessels are somewhat balanced, but not optimized for minimal resistance.
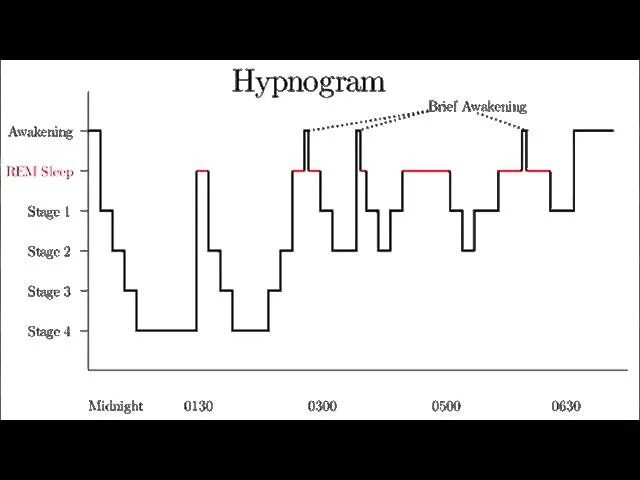
Sleep effects on respiration US Medical PG Question 2: A mother brings her 7-year-old son to the pediatrician because she is worried about his sleep. She reports that the child has repeatedly woken up in the middle of the night screaming and thrashing. Although she tries to reassure the child, he does not respond to her or acknowledge her presence. Soon after she arrives, he stops screaming and appears confused and lethargic before falling back asleep. When asked about these events, the child reports that he cannot recall ever waking up or having any bad dreams. These events typically occur within four hours of the child going to sleep. The child’s past medical history is notable for asthma and type I diabetes mellitus. He uses albuterol and long-acting insulin. There have been no recent changes in this patient’s medication regimen. His family history is notable for obesity and obstructive sleep apnea in his father. Physical examination reveals a healthy male at the 40th and 45th percentiles for height and weight, respectively. Which of the following EEG waveforms is most strongly associated with this patient’s condition?
- A. Delta waves (Correct Answer)
- B. Theta waves
- C. Sleep spindles
- D. Beta waves
- E. Alpha waves
Sleep effects on respiration Explanation: ***Delta waves***
- The child's symptoms (screaming, thrashing, unresponsiveness during waking, confusion afterward, and no recall) are characteristic of **sleep terror (pavor nocturnus)**, which is a **non-REM parasomnia**.
- Sleep terrors typically occur during **slow-wave sleep (NREM stage 3/4 sleep)**, which is predominantly characterized by the presence of **delta waves** on an EEG.
*Theta waves*
- **Theta waves** are characteristic of **NREM stage 1 and 2 sleep**, which are lighter stages of sleep.
- Sleep terrors are arousal disorders that originate from the deep stages of non-REM sleep, not the lighter stages where theta waves are prominent.
*Sleep spindles*
- **Sleep spindles** and **K-complexes** are characteristic EEG findings of **NREM stage 2 sleep**.
- While stage 2 is part of NREM sleep, sleep terrors are specifically associated with the deeper NREM stage 3/4, which is dominated by delta waves, not sleep spindles.
*Beta waves*
- **Beta waves** are high-frequency, low-amplitude waves associated with **awake, alert, and active mental states**.
- Their presence indicates wakefulness or active mental engagement and is not associated with any stage of sleep.
*Alpha waves*
- **Alpha waves** are characteristic of a state of **relaxed wakefulness**, often with closed eyes, and are a precursor to sleep onset.
- They are not associated with the deep sleep stages where sleep terrors occur.
Sleep effects on respiration US Medical PG Question 3: A 15-year-old boy is brought to the physician with excessive daytime sleepiness over the past year. His parents are concerned with his below-average school performance over the last 3 months. He goes to bed around midnight and wakes up at 7 am on school days, but sleeps in late on weekends. He exercises regularly after school. He usually has a light snack an hour before bed. He does not snore or have awakenings during sleep. He has no history of a serious illness and takes no medications. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. He does not smoke or drink alcohol. There is no history of a similar problem in the family. His vital signs are within normal limits. His BMI is 22 kg/m2. Physical examination shows no abnormal findings. Which of the following is the most appropriate recommendation at this time?
- A. Take melatonin before bedtime
- B. Avoid snacks before bedtime
- C. Decrease exercise intensity
- D. Increase nighttime sleep hours (Correct Answer)
- E. Take a nap in the afternoon
Sleep effects on respiration Explanation: ***Increase nighttime sleep hours***
- The patient's pattern of going to bed at midnight and waking at 7 AM on school days, along with sleeping in late on weekends, suggests a **chronic sleep deficit** accumulated during the week. Adolescents typically require 8-10 hours of sleep per night.
- The excessive daytime sleepiness and declining school performance are strong indicators of insufficient sleep, and **prioritizing more sleep during school nights** is the most direct intervention.
*Take melatonin before bedtime*
- Melatonin supplements are typically used for **sleep-onset insomnia** or **circadian rhythm disorders**, neither of which is clearly indicated here.
- There is no evidence presented of difficulty falling asleep; rather, the issue appears to be insufficient duration of sleep due to **late bedtime schedules**.
*Avoid snacks before bedtime*
- While heavy meals before bedtime can disrupt sleep, this patient reports having only a **light snack**, which is unlikely to be the primary cause of his significant daytime sleepiness.
- There is no mention of indigestion or gastrointestinal discomfort after the snack that would point to this as a problem.
*Decrease exercise intensity*
- Regular exercise generally **improves sleep quality**, and there's no indication that the patient's exercise routine is negatively impacting his sleep.
- While very intense exercise too close to bedtime can be disruptive for some, exercise itself is generally beneficial for sleep and overall health; therefore, reducing it would not be a primary recommendation.
*Take a nap in the afternoon*
- While naps can temporarily alleviate daytime sleepiness, they can also **disrupt nighttime sleep patterns** by reducing sleep drive.
- Napping would be treating the symptom rather than the root cause, which is a **chronic lack of sufficient nighttime sleep**.
Sleep effects on respiration US Medical PG Question 4: A 25-year-old previously healthy woman is admitted to the hospital with progressively worsening shortness of breath. She reports a mild fever. Her vital signs at the admission are as follows: blood pressure 100/70 mm Hg, heart rate 111/min, respiratory rate 20/min, and temperature 38.1℃ (100.6℉); blood saturation on room air is 90%. Examination reveals a bilateral decrease of vesicular breath sounds and rales in the lower lobes. Plain chest radiograph demonstrates bilateral opacification of the lower lobes. Despite appropriate treatment, her respiratory status worsens. The patient is transferred to the intensive care unit and put on mechanical ventilation. Adjustment of which of the following ventilator settings will only affect the patient’s oxygenation?
- A. Tidal volume and respiratory rate
- B. FiO2 and PEEP (Correct Answer)
- C. Respiratory rate and PEEP
- D. Tidal volume and FiO2
- E. FiO2 and respiratory rate
Sleep effects on respiration Explanation: ***FiO2 and PEEP***
- **FiO2 (fraction of inspired oxygen)** directly controls the oxygen concentration delivered to the patient, thus solely impacting **oxygenation**.
- **PEEP (positive end-expiratory pressure)** prevents alveolar collapse and recruits collapsed alveoli, improving the **functional residual capacity** and thus **oxygenation** without significantly altering CO2 removal (ventilation).
*Tidal volume and respiratory rate*
- **Tidal volume (Vt)** directly impacts the amount of air moved with each breath, primarily affecting **ventilation** (CO2 removal).
- **Respiratory rate (RR)** also directly determines the total minute ventilation, thus influencing **ventilation** more than oxygenation.
*Respiratory rate and PEEP*
- As mentioned, **respiratory rate** significantly affects **ventilation** by altering minute ventilation (Vt x RR).
- While **PEEP** primarily affects oxygenation, the combination with respiratory rate means it's not exclusively targeting oxygenation.
*Tidal volume and FiO2*
- **Tidal volume** is a key determinant of **ventilation** (CO2 removal), not solely oxygenation.
- **FiO2** does affect oxygenation, but its combination with tidal volume makes this option incorrect for *only* affecting oxygenation.
*FiO2 and respiratory rate*
- **FiO2** directly impacts **oxygenation**.
- **Respiratory rate** primarily affects **ventilation** (CO2 removal), thereby influencing carbonic acid levels and pH.
Sleep effects on respiration US Medical PG Question 5: A 21-year-old man is admitted to the intensive care unit for respiratory failure requiring mechanical ventilation. His minute ventilation is calculated to be 7.0 L/min, and his alveolar ventilation is calculated to be 5.1 L/min. Which of the following is most likely to decrease the difference between minute ventilation and alveolar ventilation?
- A. Increasing the partial pressure of inhaled oxygen
- B. Decreasing the affinity of hemoglobin for oxygen
- C. Increasing the respiratory depth
- D. Decreasing the physiologic dead space (Correct Answer)
- E. Increasing the respiratory rate
Sleep effects on respiration Explanation: ***Decreasing the physiologic dead space***
- The difference between **minute ventilation (VE)** and **alveolar ventilation (VA)** is the **dead space ventilation (VD)**, calculated as: VE - VA = VD
- In this case: 7.0 L/min - 5.1 L/min = 1.9 L/min of dead space ventilation
- Decreasing the **physiologic dead space** directly reduces this difference by allowing a greater proportion of each breath to participate in gas exchange
- This is the most direct way to narrow the gap between VE and VA
*Increasing the partial pressure of inhaled oxygen*
- This intervention primarily affects **oxygenation** by increasing the driving pressure for oxygen diffusion into the blood
- It does not directly change the volume of air participating in alveolar ventilation or reduce dead space ventilation
- The distribution of ventilation between alveolar and dead space remains unchanged
*Decreasing the affinity of hemoglobin for oxygen*
- A decrease in hemoglobin affinity for oxygen facilitates **oxygen unloading** to the tissues (rightward shift of the oxygen-hemoglobin dissociation curve)
- This effect is related to **oxygen delivery** and does not alter the proportion of minute ventilation that reaches the alveoli for gas exchange
- Dead space ventilation remains unchanged
*Increasing the respiratory depth*
- Increasing respiratory depth increases **tidal volume (VT)**, which improves the **ratio** of alveolar ventilation to minute ventilation (VA/VE efficiency)
- However, the **absolute difference** (VE - VA) in L/min depends on the **total dead space volume**, which is not changed by increasing tidal volume alone
- While this improves ventilation efficiency, it does not directly reduce the dead space ventilation measured in L/min unless physiologic dead space itself decreases
*Increasing the respiratory rate*
- While increasing respiratory rate increases **minute ventilation (VE)**, it also increases the frequency of ventilating the **dead space** with each breath
- Since dead space ventilation (VD) = respiratory rate × dead space volume, increasing rate while keeping tidal volume constant will proportionally increase both VE and VD
- This can actually widen the absolute gap between VE and VA, making it less efficient
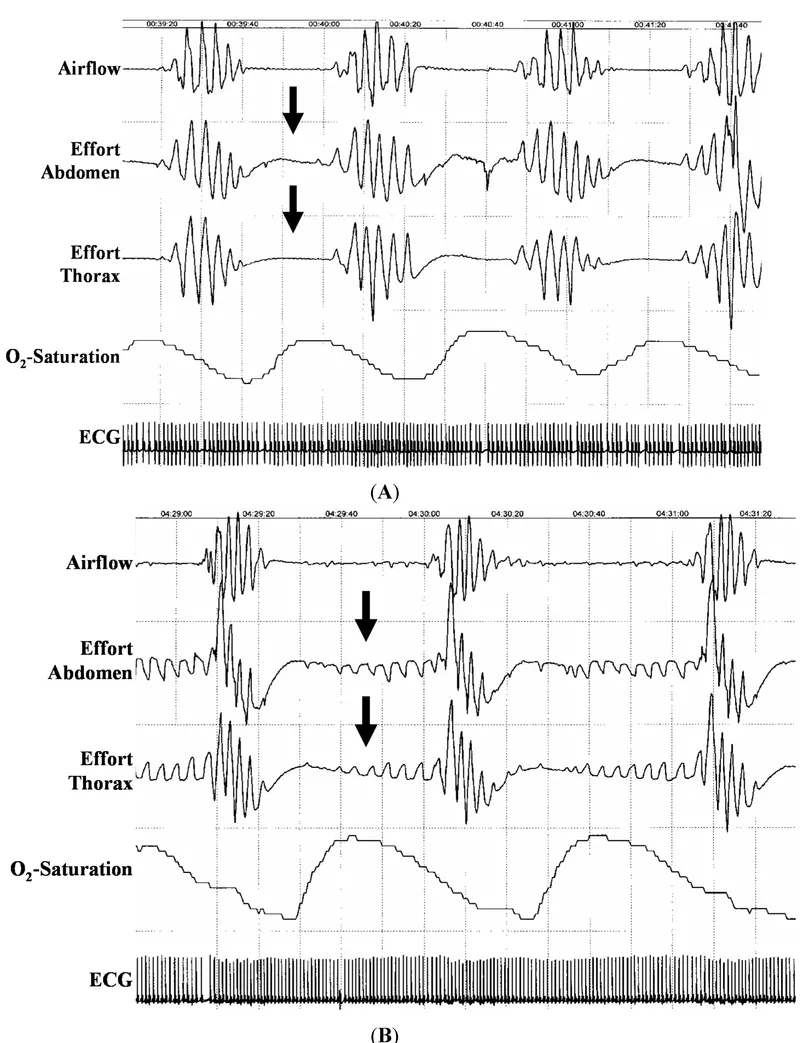
Sleep effects on respiration US Medical PG Question 6: A 64-year-old man with longstanding ischemic heart disease presents to the clinic with complaints of increasing exercise intolerance and easy fatigability for the past 2 weeks. He further states that he has been experiencing excessive daytime somnolence and shortness of breath with exertion. His wife adds that his shortness of breath is more in the recumbent position, and after approximately 2 hours of sleep, after which he suddenly wakes up suffocating and gasping for breath. This symptom is relieved after assuming an upright position for more than 30 minutes. The vital signs are as follows: heart rate, 126/min; respiratory rate, 16/min; temperature, 37.6°C (99.6°F); and blood pressure, 122/70 mm Hg. The physical examination reveals a S3 gallop on cardiac auscultation and positive hepatojugular reflux with distended neck veins. An electrocardiogram shows ischemic changes similar to ECG changes noted in the past. An echocardiogram reveals an ejection fraction of 33%. Which of the following best describes the respiratory pattern abnormality which occurs in this patient while sleeping?
- A. Decreased central hypercapnic ventilatory responsiveness
- B. Increased pulmonary artery pressure
- C. Decreased sympathetic activity
- D. Increased partial pressure of oxygen
- E. Prolonged lung-to-brain circulation time (Correct Answer)
Sleep effects on respiration Explanation: ***Prolonged lung-to-brain circulation time***
- The patient's symptoms, including **paroxysmal nocturnal dyspnea (PND)** and **Cheyne-Stokes respiration (CSR)**, are characteristic of **heart failure (HF)**. In HF, a **reduced cardiac output** leads to a **prolonged lung-to-brain circulation time**.
- This delay results in a lag between changes in blood gas levels at the lungs and their detection by central chemoreceptors in the brainstem, causing an **oscillatory ventilatory pattern**, where episodes of hyperpnea (over-breathing) and apnea (cessation of breathing) alternate.
*Decreased central hypercapnic ventilatory responsiveness*
- This would lead to **hypoventilation** and **hypercapnia (elevated CO2)**, not the alternating hyperpnea and apnea seen in **Cheyne-Stokes respiration**, which is driven by chemoreceptor instability.
- While patients with **severe chronic obstructive pulmonary disease (COPD)** can have decreased hypercapnic responsiveness, it does not explain the distinct pattern of **PND** and **CSR** observed here.
*Increased pulmonary artery pressure*
- **Increased pulmonary artery pressure (pulmonary hypertension)** is a common consequence of **heart failure** and contributes to dyspnea. However, it does not directly explain the specific **oscillatory breathing pattern** or the sudden awakening with suffocation.
- While it exacerbates respiratory symptoms, the primary mechanism of **Cheyne-Stokes respiration** relates to circulatory delay and chemoreceptor feedback.
*Decreased sympathetic activity*
- **Decreased sympathetic activity** would generally lead to a **slower heart rate** and **relaxation of airways**, which is contrary to the **tachycardia** (HR 126/min) and severe respiratory distress seen in the patient's presentation.
- **Heart failure**, especially when decompensated, is often associated with **increased sympathetic activity** as a compensatory mechanism.
*Increased partial pressure of oxygen*
- An **increased partial pressure of oxygen (PaO2)** would alleviate hypoxia and improve breathing, rather than causing **dyspnea** and a complex respiratory pattern like **Cheyne-Stokes respiration**.
- Patients with **heart failure** often experience **hypoxemia** due to pulmonary congestion, making an increased PaO2 an unlikely contributing factor to their respiratory distress.
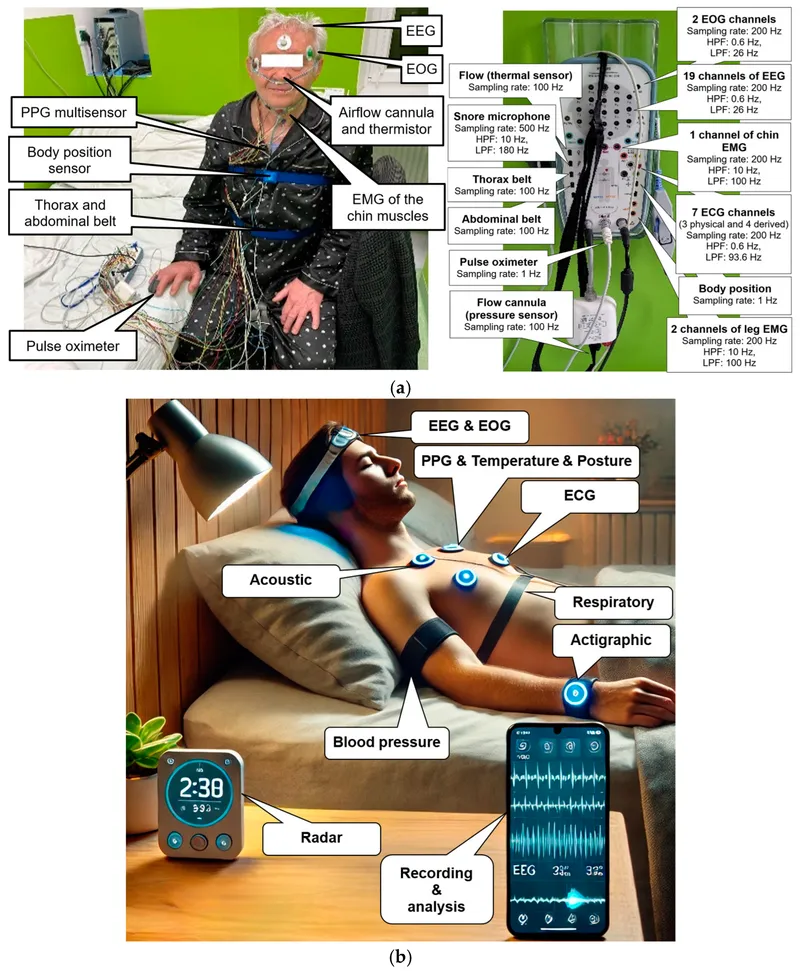
Sleep effects on respiration US Medical PG Question 7: A 55-year-old man presents to the physician for the evaluation of excessive daytime sleepiness over the past six months. Despite sleeping 8–9 hours a night and taking a nap during the day, he feels drowsy and is afraid to drive. His wife complains of loud snoring and gasping during the night. His blood pressure is 155/95 mm Hg. BMI is 37 kg/m2. Oropharyngeal examination shows a small orifice and an enlarged tongue and uvula. The soft palate is low-lying. The examination of the nasal cavity shows no septal deviation or polyps. Examination of the lungs and heart shows no abnormalities. Polysomnography shows an apnea-hypopnea index of 20 episodes/h. The patient is educated about weight loss, exercise, and regular sleep hours and duration. Which of the following is the most appropriate next step in management?
- A. Continuous positive airway pressure (Correct Answer)
- B. Upper airway neurostimulation
- C. Supplemental oxygen
- D. Oral appliances
- E. Upper airway surgery
Sleep effects on respiration Explanation: ***Continuous positive airway pressure***
- This patient presents with symptoms and polysomnography findings consistent with **moderate to severe obstructive sleep apnea (OSA)** (apnea-hypopnea index of 20 episodes/h). **CPAP is the first-line treatment** for such cases.
- CPAP works by **delivering pressurized air** via a mask, creating a pneumatic splint that prevents the collapse of the upper airway during sleep, thereby reducing apneas and hypopneas.
*Upper airway neurostimulation*
- This therapy involves stimulating the **hypoglossal nerve** to activate upper airway muscles, improving airway patency.
- However, it is generally considered a **second-line treatment** for patients with moderate to severe OSA who **cannot tolerate or fail CPAP therapy**.
*Supplemental oxygen*
- While oxygen therapy can reduce nocturnal desaturation, it **does not address the underlying airway obstruction** that causes apneas and hypopneas.
- It might even **worsen apnea by blunting the ventilatory drive**, making it an inappropriate primary treatment for OSA.
*Oral appliances*
- **Mandibular advancement devices (MADs)** can be effective for **mild to moderate OSA**, or for patients with severe OSA who cannot tolerate CPAP.
- They work by repositioning the jaw and tongue forward to enlarge the pharyngeal space, but CPAP is generally more effective for the severity described.
*Upper airway surgery*
- Various surgical procedures, such as **uvulopalatopharyngoplasty (UPPP)**, aim to remove excess tissue in the pharynx to enlarge the airway.
- Surgery is typically reserved for patients who **fail or cannot tolerate CPAP and oral appliances** and are carefully selected based on anatomical considerations.
Sleep effects on respiration US Medical PG Question 8: A 25-year-old male presents to his primary care physician with a chief complaint of anxiety and fatigue. The patient states that during this past week he has had final exams and has been unable to properly study and prepare because he is so exhausted. He states that he has been going to bed early but has been unable to get a good night’s sleep. The patient admits to occasional cocaine and marijuana use. Otherwise, the patient has no significant past medical history and is not taking any medications. On physical exam you note a tired and anxious appearing young man. His neurological exam is within normal limits. The patient states that he fears he will fail his courses if he does not come up with a solution. Which of the following is the best initial step in management?
- A. Polysomnography
- B. Sleep hygiene education (Correct Answer)
- C. Alprazolam
- D. Melatonin
- E. Zolpidem
Sleep effects on respiration Explanation: ***Sleep hygiene education***
- This is the **best initial step** because it addresses lifestyle factors that commonly contribute to **insomnia and fatigue**, especially during periods of stress like final exams.
- Helping the patient establish **regular sleep patterns**, avoid stimulants, and create a conducive sleep environment can significantly improve sleep quality without medication.
*Polysomnography*
- This is a diagnostic test typically reserved for when a **primary sleep disorder** like sleep apnea or restless legs syndrome is suspected.
- Given the patient's acute stressor (final exams) and **drug use**, lifestyle interventions should be tried first before pursuing expensive and invasive testing.
*Alprazolam*
- This is a **benzodiazepine** that can be used for acute anxiety or insomnia, but it carries a risk of **dependence, tolerance, and withdrawal**.
- It is not a first-line treatment for a patient experiencing sleep difficulties primarily due to stress and poor sleep habits, and its use should be avoided in those with a history of substance abuse.
*Melatonin*
- Melatonin can be helpful for **circadian rhythm disorders** or jet lag, but its efficacy for primary insomnia is limited and inconsistent.
- While it has fewer side effects than prescription hypnotics, **sleep hygiene education** is still a more fundamental and effective initial approach for this patient.
*Zolpidem*
- This is a **non-benzodiazepine hypnotic** often prescribed for short-term insomnia, but it has potential side effects like **next-day drowsiness** and can be abused, especially in individuals with a history of substance use.
- **Sleep hygiene** should always be optimized first, especially in a young patient whose sleep issues are clearly linked to stress and lifestyle.
Sleep effects on respiration US Medical PG Question 9: A 35-year-old woman volunteers for a study on respiratory physiology. Pressure probes A and B are placed as follows:
Probe A: between the parietal and visceral pleura
Probe B: within the cavity of an alveolus
The probes provide a pressure reading relative to atmospheric pressure. To obtain a baseline reading, she is asked to sit comfortably and breathe normally. Which of the following sets of values will most likely be seen at the end of inspiration?
- A. Probe A: -6 mm Hg; Probe B: 0 mm Hg (Correct Answer)
- B. Probe A: 0 mm Hg; Probe B: -1 mm Hg
- C. Probe A: -4 mm Hg; Probe B: 0 mm Hg
- D. Probe A: -4 mm Hg; Probe B: -1 mm Hg
- E. Probe A: -6 mm Hg; Probe B: -1 mm Hg
Sleep effects on respiration Explanation: ***Probe A: -6 mm Hg; Probe B: 0 mm Hg***
- At the **end of inspiration**, the **intrapleural pressure (Probe A)** is at its most negative, typically around -6 to -8 cm H2O (equivalent to -4 to -6 mmHg), reflecting the maximum expansion of the thoracic cavity.
- At the **end of inspiration**, just before exhalation begins, there is **no airflow**, so the **intrapulmonary pressure (Probe B)** equalizes with atmospheric pressure, resulting in a 0 mm Hg reading.
*Probe A: 0 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of 0 mm Hg** would indicate a **pneumothorax** since it should always be negative to prevent lung collapse.
- An **intrapulmonary pressure of -1 mm Hg** would indicate that **inspiration is still ongoing**, as air would be flowing into the lungs.
*Probe A: -4 mm Hg; Probe B: 0 mm Hg*
- While an **intrapulmonary pressure of 0 mm Hg** is correct at the end of inspiration, an **intrapleural pressure of -4 mm Hg** is typical for the **end of expiration (Functional Residual Capacity)** during quiet breathing, not the end of inspiration.
- The **intrapleural pressure becomes more negative** during inspiration due to increased thoracic volume, so -4 mm Hg would be insufficient.
*Probe A: -4 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of -4 mm Hg** is the normal pressure at the **end of expiration**, not the end of inspiration, where it becomes more negative.
- An **intrapulmonary pressure of -1 mm Hg** indicates that **inspiration is still in progress**, not at its end, as air would still be flowing into the lungs.
*Probe A: -6 mm Hg; Probe B: -1 mm Hg*
- While an **intrapleural pressure of -6 mm Hg** is consistent with the end of inspiration, an **intrapulmonary pressure of -1 mm Hg** means that **airflow is still occurring into the lungs**.
- At the **very end of inspiration**, just before the start of exhalation, airflow momentarily ceases, and intrapulmonary pressure becomes zero relative to the atmosphere.
Sleep effects on respiration US Medical PG Question 10: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Sleep effects on respiration Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
More Sleep effects on respiration US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.