Respiratory centers in the brainstem US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Respiratory centers in the brainstem. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Respiratory centers in the brainstem US Medical PG Question 1: A 21-year-old man presents to his physician because he has been feeling increasingly tired and short of breath at work. He has previously had these symptoms but cannot recall the diagnosis he was given. Chart review reveals the following results:
Oxygen tension in inspired air = 150 mmHg
Alveolar carbon dioxide tension = 50 mmHg
Arterial oxygen tension = 71 mmHg
Respiratory exchange ratio = 0.80
Diffusion studies reveal normal diffusion distance. The patient is administered 100% oxygen but the patient's blood oxygen concentration does not improve. Which of the following conditions would best explain this patient's findings?
- A. Septal defect since birth (Correct Answer)
- B. Use of opioid medications
- C. Pulmonary fibrosis
- D. Pulmonary embolism
- E. Vacation at the top of a mountain
Respiratory centers in the brainstem Explanation: ***Septal defect since birth***
- A congenital heart disease like a **septal defect** causes a right-to-left **shunt**, meaning deoxygenated blood bypasses the lungs and mixes with oxygenated blood.
- This type of shunt leads to **hypoxemia that is refractory to 100% oxygen** because the shunted blood will never pick up oxygen from the lungs.
*Use of opioid medications*
- Opioid use causes **respiratory depression**, leading to **hypoventilation** and increased arterial CO2 with decreased arterial O2.
- However, the hypoxemia from hypoventilation would typically improve significantly with **100% oxygen administration**, unlike in this case.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** causes thickening of the alveolar-capillary membrane, leading to impaired gas exchange and **diffusion limitation**.
- While it causes hypoxemia, the diffusion studies are stated to be **normal**, and hypoxemia due to diffusion limitation often improves with supplemental oxygen.
*Pulmonary embolism*
- A **pulmonary embolism** leads to V/Q mismatch by blocking blood flow to a portion of the lung, causing ventilation with no perfusion.
- Hypoxemia from V/Q mismatch generally **responds well to supplemental oxygen**, as the non-affected lung areas can compensate, unlike the scenario described.
*Vacation at the top of a mountain*
- Being at a high altitude causes **hypobaric hypoxia**, meaning there is a reduced partial pressure of oxygen in the inspired air.
- This type of hypoxemia typically **improves with supplemental oxygen** as it increases the inspired oxygen tension, which is contrary to the patient's findings.
Respiratory centers in the brainstem US Medical PG Question 2: A 19-year-old man comes to the emergency department with sharp, left-sided chest pain and shortness of breath. He has no history of recent trauma. He does not smoke or use illicit drugs. He is 196 cm (6 feet 5 in) tall and weighs 70 kg (154 lb); BMI is 18 kg/m2. Examination shows reduced breath sounds over the left lung field. An x-ray of the chest is shown. Which of the following changes is most likely to immediately result from this patient's current condition?
- A. Increased intra-alveolar pressure
- B. Increased right-to-left shunting (Correct Answer)
- C. Increased lung compliance
- D. Increased transpulmonary pressure
- E. Increased physiological dead space
Respiratory centers in the brainstem Explanation: ***Increased right-to-left shunting***
- The patient has a **spontaneous pneumothorax** (common in tall, thin young males) causing **left lung collapse**.
- In the collapsed lung, alveoli are **not ventilated but continue to be perfused** (at least initially, before hypoxic pulmonary vasoconstriction fully develops), creating **perfusion without ventilation**.
- This represents a **low V/Q ratio approaching zero (true shunt)**, where deoxygenated blood bypasses functional gas exchange units, resulting in **increased right-to-left shunting** and immediate hypoxemia.
- This is the **immediate pathophysiologic change** that causes the patient's shortness of breath and hypoxemia.
*Increased intra-alveolar pressure*
- In a **pneumothorax**, air enters the pleural space, increasing **pleural pressure** and causing lung collapse.
- The collapsed alveoli have **reduced or zero pressure**, not increased pressure.
- Intra-alveolar pressure would only increase in a **tension pneumothorax** with a one-way valve effect, which is not described here.
*Increased lung compliance*
- **Compliance** (ΔV/ΔP) measures how easily the lung expands.
- A **collapsed lung** has **decreased compliance** because it is harder to re-expand due to loss of surfactant function and alveolar collapse.
- The chest wall compliance may increase, but lung parenchymal compliance decreases.
*Increased transpulmonary pressure*
- **Transpulmonary pressure** = alveolar pressure - pleural pressure; this is the pressure that keeps the lung inflated.
- In pneumothorax, air in the pleural space **increases pleural pressure** (makes it less negative or even positive).
- This **reduces the transpulmonary pressure gradient**, causing lung collapse, not an increase.
*Increased physiological dead space*
- **Physiological dead space** occurs when alveoli are **ventilated but not perfused** (high V/Q ratio or wasted ventilation).
- In pneumothorax, the primary immediate problem is the **opposite**: the collapsed lung has **perfusion without ventilation** (shunt, low V/Q ratio).
- While the contralateral lung may develop some dead space from compensatory hyperventilation and redistribution, the **immediate dominant change** is shunt physiology from the collapsed lung, not dead space.
Respiratory centers in the brainstem US Medical PG Question 3: During exercise, what is the primary mechanism for increased oxygen delivery to active muscles?
- A. Decreased blood viscosity
- B. Increased cardiac output (Correct Answer)
- C. Increased hemoglobin affinity
- D. Enhanced oxygen diffusion
Respiratory centers in the brainstem Explanation: ***Increased cardiac output***
- During exercise, **cardiac output** increases significantly due to both an elevated **heart rate** and increased **stroke volume**, directly pushing more oxygenated blood to the active muscles.
- This augmentation in blood flow is the primary factor ensuring a sufficient supply of oxygen and nutrients to meet the heightened metabolic demands of exercising muscles.
*Decreased blood viscosity*
- While factors like **hemodilution** can decrease blood viscosity during prolonged exercise, this effect is relatively minor and not the primary mechanism for acute increases in oxygen delivery compared to the dramatic increase in cardiac output.
- A decrease in blood viscosity can slightly improve flow efficiency, but it doesn't fundamentally change the amount of blood pumped per minute to the muscles.
*Increased hemoglobin affinity*
- An *increased* hemoglobin affinity for oxygen would actually make it *harder* for oxygen to unload from hemoglobin to the tissues, which is counterproductive for oxygen delivery during exercise.
- In fact, during exercise, local conditions like increased temperature, decreased pH (**Bohr effect**), and increased 2,3-BPG tend to *decrease* hemoglobin's affinity for oxygen, facilitating oxygen release to active muscles.
*Enhanced oxygen diffusion*
- While exercise does improve the efficiency of oxygen extraction at the tissue level due to a steeper partial pressure gradient and increased capillary recruitment, the *rate* of oxygen diffusion across the capillary membrane isn't the primary modulator of overall oxygen delivery.
- The main determinant is the *amount* of oxygenated blood reaching the muscle, which is governed by cardiac output and local blood flow regulation.
Respiratory centers in the brainstem US Medical PG Question 4: A 66-year-old man is brought to the emergency department because of shortness of breath and confusion. His pulse is 98/min, and blood pressure is 109/73 mm Hg. He is oriented to person but not time or place. A graph of his breathing pattern and oxygen saturation is shown. Which of the following additional findings is most likely present in this patient?
- A. Rib fracture
- B. Fruity breath odor
- C. Ventricular gallop (Correct Answer)
- D. Miotic pupils
- E. Barrel chest
Respiratory centers in the brainstem Explanation: ***Ventricular gallop***
- The patient's presentation with **shortness of breath**, **confusion**, and **oxygen desaturation** coupled with the breathing pattern shown (likely Cheyne-Stokes respiration from the image) strongly suggests **heart failure**. A **ventricular gallop (S3 heart sound)** is a classic finding in heart failure, indicating rapid ventricular filling into a stiff or dilated ventricle.
- The **confusional state** and **tachypnea (implied by oxygen desaturation)** are consistent with **hypoxia** and **reduced cardiac output** often seen in decompensated heart failure, where an S3 gallop is frequently heard.
*Rib fracture*
- While a rib fracture can cause shortness of breath due to pain and reduced chest expansion, it would not typically lead to **confusion** or a specific cyclical breathing pattern like Cheyne-Stokes, nor would it directly cause a ventricular gallop.
- The patient's vital signs and mental status point towards a more systemic issue rather than isolated chest trauma.
*Fruity breath odor*
- A **fruity breath odor** is a hallmark of **diabetic ketoacidosis (DKA)**, caused by the exhalation of acetone. This condition would also present with confusion and tachypnea, but would typically involve hyperglycemia and metabolic acidosis.
- There is no information to suggest diabetes, and the presentation of a specific breathing pattern in correlation with cardiac findings makes heart failure more likely.
*Miotic pupils*
- **Miotic pupils (pinpoint pupils)** are strongly associated with **opioid overdose** or organophosphate poisoning. These conditions would cause respiratory depression, not necessarily the specific breathing pattern, and would not explain the other findings in this specific context.
- The patient's pulse and blood pressure are also not typical of severe opioid overdose, which often involves bradycardia and hypotension.
*Barrel chest*
- A **barrel chest** is a physical finding typically associated with **chronic obstructive pulmonary disease (COPD)** due to chronic air trapping. While COPD can cause shortness of breath and confusion (in acute exacerbations), it does not directly lead to a ventricular gallop.
- Although the patient's age makes COPD possible, the acute presentation with a specific breathing pattern and the likelihood of heart failure make a barrel chest a less specific or primary finding in this context.
Respiratory centers in the brainstem US Medical PG Question 5: A 25-year-old previously healthy woman is admitted to the hospital with progressively worsening shortness of breath. She reports a mild fever. Her vital signs at the admission are as follows: blood pressure 100/70 mm Hg, heart rate 111/min, respiratory rate 20/min, and temperature 38.1℃ (100.6℉); blood saturation on room air is 90%. Examination reveals a bilateral decrease of vesicular breath sounds and rales in the lower lobes. Plain chest radiograph demonstrates bilateral opacification of the lower lobes. Despite appropriate treatment, her respiratory status worsens. The patient is transferred to the intensive care unit and put on mechanical ventilation. Adjustment of which of the following ventilator settings will only affect the patient’s oxygenation?
- A. Tidal volume and respiratory rate
- B. FiO2 and PEEP (Correct Answer)
- C. Respiratory rate and PEEP
- D. Tidal volume and FiO2
- E. FiO2 and respiratory rate
Respiratory centers in the brainstem Explanation: ***FiO2 and PEEP***
- **FiO2 (fraction of inspired oxygen)** directly controls the oxygen concentration delivered to the patient, thus solely impacting **oxygenation**.
- **PEEP (positive end-expiratory pressure)** prevents alveolar collapse and recruits collapsed alveoli, improving the **functional residual capacity** and thus **oxygenation** without significantly altering CO2 removal (ventilation).
*Tidal volume and respiratory rate*
- **Tidal volume (Vt)** directly impacts the amount of air moved with each breath, primarily affecting **ventilation** (CO2 removal).
- **Respiratory rate (RR)** also directly determines the total minute ventilation, thus influencing **ventilation** more than oxygenation.
*Respiratory rate and PEEP*
- As mentioned, **respiratory rate** significantly affects **ventilation** by altering minute ventilation (Vt x RR).
- While **PEEP** primarily affects oxygenation, the combination with respiratory rate means it's not exclusively targeting oxygenation.
*Tidal volume and FiO2*
- **Tidal volume** is a key determinant of **ventilation** (CO2 removal), not solely oxygenation.
- **FiO2** does affect oxygenation, but its combination with tidal volume makes this option incorrect for *only* affecting oxygenation.
*FiO2 and respiratory rate*
- **FiO2** directly impacts **oxygenation**.
- **Respiratory rate** primarily affects **ventilation** (CO2 removal), thereby influencing carbonic acid levels and pH.
Respiratory centers in the brainstem US Medical PG Question 6: A 64-year-old man with longstanding ischemic heart disease presents to the clinic with complaints of increasing exercise intolerance and easy fatigability for the past 2 weeks. He further states that he has been experiencing excessive daytime somnolence and shortness of breath with exertion. His wife adds that his shortness of breath is more in the recumbent position, and after approximately 2 hours of sleep, after which he suddenly wakes up suffocating and gasping for breath. This symptom is relieved after assuming an upright position for more than 30 minutes. The vital signs are as follows: heart rate, 126/min; respiratory rate, 16/min; temperature, 37.6°C (99.6°F); and blood pressure, 122/70 mm Hg. The physical examination reveals a S3 gallop on cardiac auscultation and positive hepatojugular reflux with distended neck veins. An electrocardiogram shows ischemic changes similar to ECG changes noted in the past. An echocardiogram reveals an ejection fraction of 33%. Which of the following best describes the respiratory pattern abnormality which occurs in this patient while sleeping?
- A. Decreased central hypercapnic ventilatory responsiveness
- B. Increased pulmonary artery pressure
- C. Decreased sympathetic activity
- D. Increased partial pressure of oxygen
- E. Prolonged lung-to-brain circulation time (Correct Answer)
Respiratory centers in the brainstem Explanation: ***Prolonged lung-to-brain circulation time***
- The patient's symptoms, including **paroxysmal nocturnal dyspnea (PND)** and **Cheyne-Stokes respiration (CSR)**, are characteristic of **heart failure (HF)**. In HF, a **reduced cardiac output** leads to a **prolonged lung-to-brain circulation time**.
- This delay results in a lag between changes in blood gas levels at the lungs and their detection by central chemoreceptors in the brainstem, causing an **oscillatory ventilatory pattern**, where episodes of hyperpnea (over-breathing) and apnea (cessation of breathing) alternate.
*Decreased central hypercapnic ventilatory responsiveness*
- This would lead to **hypoventilation** and **hypercapnia (elevated CO2)**, not the alternating hyperpnea and apnea seen in **Cheyne-Stokes respiration**, which is driven by chemoreceptor instability.
- While patients with **severe chronic obstructive pulmonary disease (COPD)** can have decreased hypercapnic responsiveness, it does not explain the distinct pattern of **PND** and **CSR** observed here.
*Increased pulmonary artery pressure*
- **Increased pulmonary artery pressure (pulmonary hypertension)** is a common consequence of **heart failure** and contributes to dyspnea. However, it does not directly explain the specific **oscillatory breathing pattern** or the sudden awakening with suffocation.
- While it exacerbates respiratory symptoms, the primary mechanism of **Cheyne-Stokes respiration** relates to circulatory delay and chemoreceptor feedback.
*Decreased sympathetic activity*
- **Decreased sympathetic activity** would generally lead to a **slower heart rate** and **relaxation of airways**, which is contrary to the **tachycardia** (HR 126/min) and severe respiratory distress seen in the patient's presentation.
- **Heart failure**, especially when decompensated, is often associated with **increased sympathetic activity** as a compensatory mechanism.
*Increased partial pressure of oxygen*
- An **increased partial pressure of oxygen (PaO2)** would alleviate hypoxia and improve breathing, rather than causing **dyspnea** and a complex respiratory pattern like **Cheyne-Stokes respiration**.
- Patients with **heart failure** often experience **hypoxemia** due to pulmonary congestion, making an increased PaO2 an unlikely contributing factor to their respiratory distress.
Respiratory centers in the brainstem US Medical PG Question 7: A 55-year-old man presents with an unremitting cough and swelling of the lower limbs for the past 2 weeks. He says he has had a chronic cough for years, however, he feels it is getting worse. He reports a 30-pack-year smoking history. Physical examination reveals mild central cyanosis and expiratory wheezes throughout the chest. Oxygen therapy is ordered immediately but, soon after administering it, his respiratory rate starts to slow down and he becomes drowsy. Dysfunction of which of the following receptors most likely led to this patient’s current condition?
- A. Pleural pain receptors
- B. Central chemoreceptors
- C. Airway stretch receptors
- D. Pulmonary stretch receptors
- E. Peripheral chemoreceptors (Correct Answer)
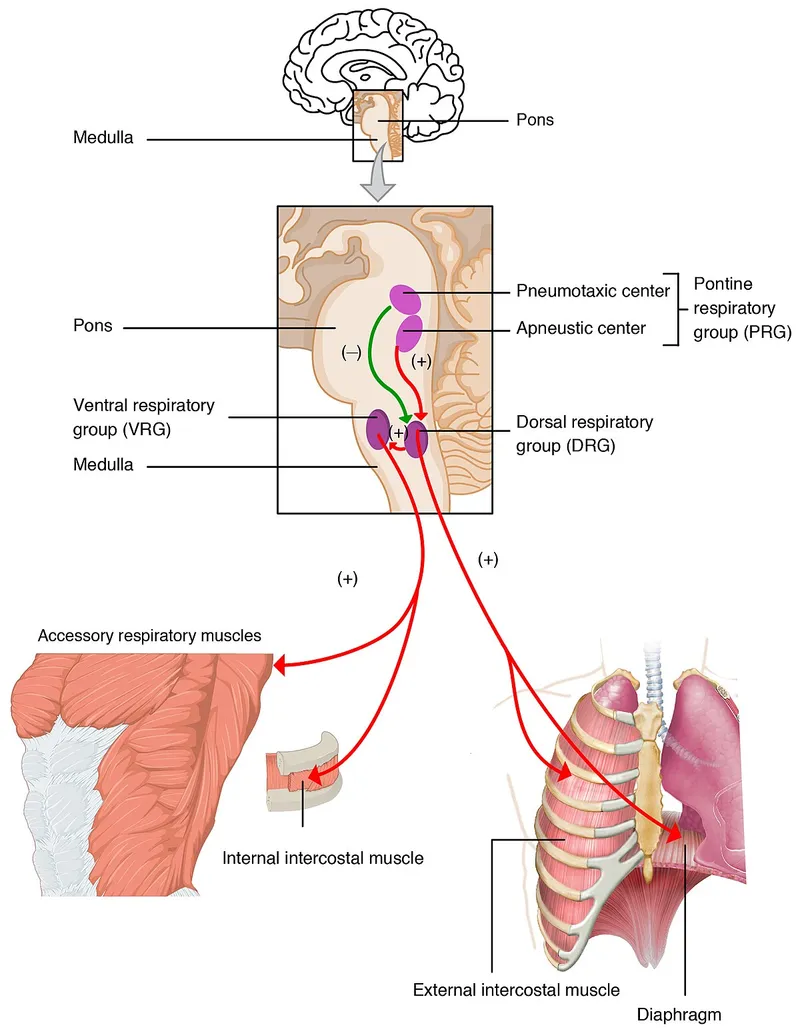
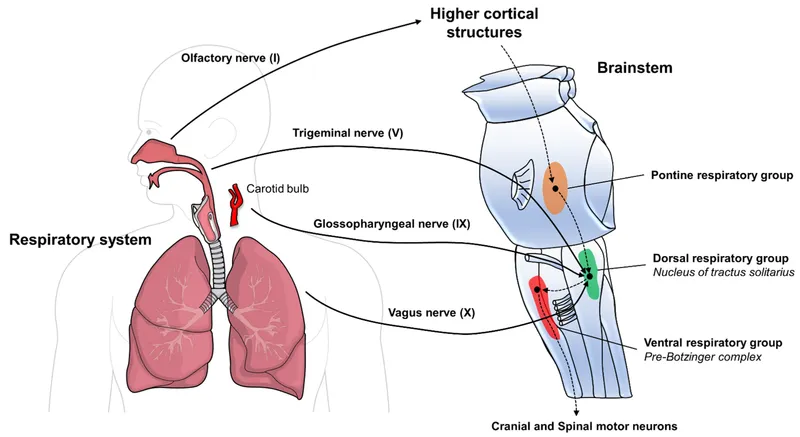
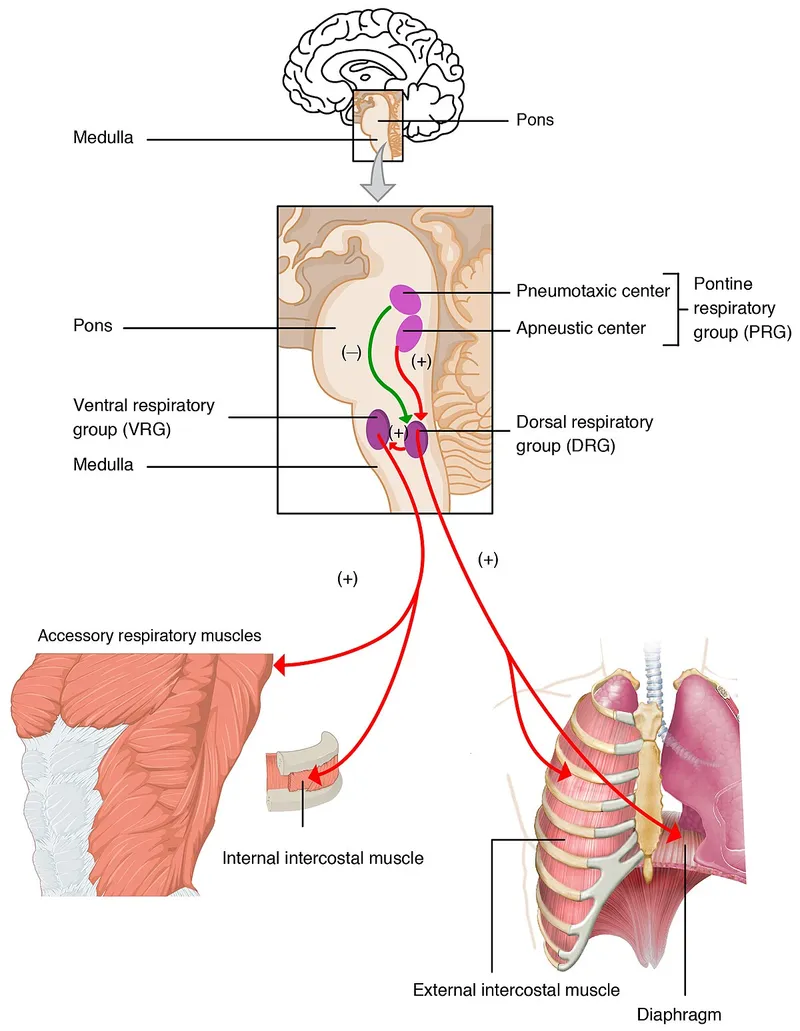
Respiratory centers in the brainstem Explanation: ***Peripheral chemoreceptors***
- In patients with chronic obstructive pulmonary disease (COPD) like this patient, the **central chemoreceptors** become desensitized to chronically elevated CO2 levels. Their primary respiratory drive then shifts to the **peripheral chemoreceptors** (carotid and aortic bodies), which are sensitive to **hypoxia**.
- Administering high-flow oxygen **eliminates the hypoxic stimulus** sensed by these normally functioning peripheral chemoreceptors, removing the hypoxic drive to breathe and leading to **hypoventilation, CO2 retention, respiratory acidosis**, and drowsiness (CO2 narcosis).
*Pleural pain receptors*
- These receptors are primarily involved in sensing pain associated with **pleural inflammation** or injury, contributing to the sensation of pain with breathing.
- They do not play a role in regulating the primary ventilatory drive in response to blood gas changes.
*Central chemoreceptors*
- These receptors are located in the **medulla** and are primarily sensitive to changes in **arterial PCO2** and pH (via H+ ions in CSF).
- In chronic respiratory diseases with CO2 retention, they become **desensitized** to elevated CO2, shifting the main respiratory drive to the peripheral chemoreceptors' response to hypoxia.
*Airway stretch receptors*
- These receptors, including **slowly adapting stretch receptors** and **rapidly adapting irritant receptors**, are located in the airways and respond to lung inflation and irritants.
- They are involved in the Hering-Breuer reflex and cough reflex but are not the primary drivers of ventilation in response to hypoxemia.
*Pulmonary stretch receptors*
- These receptors are located in the **bronchial smooth muscle** and respond to lung distension, contributing to the **Hering-Breuer reflex** which inhibits inspiration to prevent overinflation.
- While important for lung mechanics, they do not directly sense blood gas levels to drive ventilation in the context of hypoxia or hypercapnia.
Respiratory centers in the brainstem US Medical PG Question 8: A middle-aged homeless man is found lying unresponsive on the streets by the police and is rushed to the emergency department. His vital signs include: blood pressure 110/80 mm Hg, pulse rate 100/min, and respirations 10/min and shallow. On physical examination, his extremities are cold and clammy. Pupils are constricted and non-reactive. His blood glucose is 55 mg/dL. IV access is established immediately with the administration of dextrose and naloxone. In half an hour, the patient is fully conscious, alert and responsive. He denies any medical illnesses, hospitalizations, or surgeries in the past. Physical examination reveals injection track marks along both arms. He admits to the use of cocaine and heroin. He smokes cigarettes and consumes alcohol. His vital signs are now stable. A urine sample is sent for toxicology screening. Which of the following was the most likely cause of this patient’s respiratory depression?
- A. Opioid intoxication (Correct Answer)
- B. Alcohol intoxication
- C. Cocaine abuse
- D. Hallucinogen toxicity
- E. Hypoglycemia
Respiratory centers in the brainstem Explanation: ***Opioid intoxication***
- The patient's presentation with **respiratory depression** (respirations 10/min), **constricted pupils**, and rapid improvement after **naloxone administration** strongly indicates opioid overdose.
- The presence of **injection track marks** and admitted **heroin use** further supports opioid intoxication as the primary cause.
*Alcohol intoxication*
- While alcohol can cause respiratory depression and altered mental status, it typically presents with **dilated pupils** or normal pupils, not pinpoint pupils.
- The rapid reversal with **naloxone** would not occur in pure alcohol intoxication.
*Cocaine abuse*
- Cocaine is a **stimulant** and typically causes **tachycardia**, **hypertension**, **mydriasis (dilated pupils)**, and potentially agitation or seizures, rather than respiratory depression and constricted pupils.
- It would not respond to naloxone.
*Hallucinogen toxicity*
- Hallucinogens (e.g., LSD, PCP) primarily affect perception, mood, and thought, causing **psychosis**, **hallucinations**, and **agitation**, not severe respiratory depression or constricted pupils.
- Their effects are not reversed by naloxone.
*Hypoglycemia*
- Although the patient had a blood glucose of 55 mg/dL (mild hypoglycemia), the primary cause of respiratory depression was reversed by **naloxone**, not solely by dextrose.
- While hypoglycemia can cause altered mental status, it does not typically cause **pinpoint pupils** or such profound respiratory depression that is immediately reversed by an opioid antagonist.
Respiratory centers in the brainstem US Medical PG Question 9: A 60-year-old woman with a history of emphysema has been referred by her pulmonologist for follow-up pulmonary function testing. During the test, the patient reaches a point where her airway pressure is equal to the atmospheric pressure. Which of the following is most likely to be found during this respiratory state?
- A. Pulmonary vascular resistance is at a maximum
- B. Transmural pressure of the lung-chest wall system is at a maximum
- C. Transmural pressure of the chest wall is at a minimum
- D. Pulmonary vascular resistance is at a minimum (Correct Answer)
- E. Transmural pressure of the lung-chest wall system is at a minimum
Respiratory centers in the brainstem Explanation: ***Pulmonary vascular resistance is at a minimum***
- When airway pressure equals atmospheric pressure during a pulmonary function test, the lungs are at **functional residual capacity (FRC)** or resting state.
- At FRC, **pulmonary vascular resistance (PVR)** is at its lowest point due to the optimal balance between alveolar and extra-alveolar vessel compression/distension.
- Extra-alveolar vessels are compressed at low lung volumes, while alveolar vessels are compressed at high lung volumes. At FRC, both are optimally distended, resulting in **minimal PVR**.
*Pulmonary vascular resistance is at a maximum*
- PVR increases at very low lung volumes (due to extra-alveolar vessel compression) and very high lung volumes (due to alveolar vessel compression).
- The resting state (airway pressure equals atmospheric pressure) corresponds to FRC, where PVR is **minimal, not maximal**.
*Transmural pressure of the lung-chest wall system is at a maximum*
- Transmural pressure of the lung-chest wall system represents the pressure difference across the entire respiratory system.
- This pressure is higher during inspiration or forced expiration when the system is stretched or compressed.
- At FRC (airway pressure equals atmospheric pressure), the system is at **resting equilibrium**, not at maximal transmural pressure.
*Transmural pressure of the chest wall is at a minimum*
- Transmural pressure across the chest wall is the difference between intrapleural pressure and atmospheric pressure.
- This pressure is not at a minimum when airway pressure equals atmospheric pressure.
- Chest wall transmural pressure is actually minimal near **residual volume (RV)**, where the chest wall recoils inward most strongly.
*Transmural pressure of the lung-chest wall system is at a minimum*
- Transmural pressure of the lung-chest wall system reflects the elastic recoil forces of the combined system.
- At FRC (airway pressure equals atmospheric pressure), elastic recoil forces are balanced at equilibrium, but transmural pressure is **not at a minimum**—it represents the neutral resting state.
Respiratory centers in the brainstem US Medical PG Question 10: A 15-year-old boy and his mother were referred to a pulmonology clinic. She is concerned that her son is having some breathing difficulty for the past few months, which is aggravated with exercise. The family is especially concerned because the patient’s older brother has cystic fibrosis. The past medical history is noncontributory. Today, the vital signs include: blood pressure 119/80 mm Hg, heart rate 90/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical exam, he appears well-developed and well-nourished. The heart has a regular rate and rhythm, and the lungs are clear to auscultation bilaterally. During the exam, he is brought into a special room to test his breathing. A clamp is placed on his nose and he is asked to take in as much air as he can, and then forcefully expire all the air into a spirometer. The volume of expired air represents which of the following?
- A. Tidal volume
- B. Total lung capacity
- C. Functional residual capacity
- D. Expiratory reserve volume
- E. Vital capacity (Correct Answer)
Respiratory centers in the brainstem Explanation: ***Vital capacity***
- **Vital capacity (VC)** is the maximum volume of air exhaled after a maximal inspiration. The maneuver described ("take in as much air as he can, and then forcefully expire all the air") directly measures vital capacity.
- VC includes the **tidal volume (TV)**, **inspiratory reserve volume (IRV)**, and **expiratory reserve volume (ERV)**.
*Tidal volume*
- **Tidal volume (TV)** is the volume of air inspired or expired with a normal breath, not the maximal forceful expiration described.
- It represents the usual volume of air exchanged during quiet breathing.
*Total lung capacity*
- **Total lung capacity (TLC)** is the maximum volume of air that the lungs can hold after a maximal inspiration, including the residual volume.
- This cannot be measured directly by spirometry alone, as it includes the **residual volume** which is the air remaining in the lungs after maximal expiration.
*Functional residual capacity*
- **Functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal, quiet expiration.
- Like TLC and residual volume, FRC cannot be measured directly by standard spirometry.
*Expiratory reserve volume*
- **Expiratory reserve volume (ERV)** is the maximum volume of air that can be *additionally* exhaled after a normal exhalation.
- The patient was asked to expire all the air after a maximal inspiration, which is a measure of vital capacity, not just ERV.
More Respiratory centers in the brainstem US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.