Integrated respiratory responses US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Integrated respiratory responses. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Integrated respiratory responses US Medical PG Question 1: A 21-year-old man presents to his physician because he has been feeling increasingly tired and short of breath at work. He has previously had these symptoms but cannot recall the diagnosis he was given. Chart review reveals the following results:
Oxygen tension in inspired air = 150 mmHg
Alveolar carbon dioxide tension = 50 mmHg
Arterial oxygen tension = 71 mmHg
Respiratory exchange ratio = 0.80
Diffusion studies reveal normal diffusion distance. The patient is administered 100% oxygen but the patient's blood oxygen concentration does not improve. Which of the following conditions would best explain this patient's findings?
- A. Septal defect since birth (Correct Answer)
- B. Use of opioid medications
- C. Pulmonary fibrosis
- D. Pulmonary embolism
- E. Vacation at the top of a mountain
Integrated respiratory responses Explanation: ***Septal defect since birth***
- A congenital heart disease like a **septal defect** causes a right-to-left **shunt**, meaning deoxygenated blood bypasses the lungs and mixes with oxygenated blood.
- This type of shunt leads to **hypoxemia that is refractory to 100% oxygen** because the shunted blood will never pick up oxygen from the lungs.
*Use of opioid medications*
- Opioid use causes **respiratory depression**, leading to **hypoventilation** and increased arterial CO2 with decreased arterial O2.
- However, the hypoxemia from hypoventilation would typically improve significantly with **100% oxygen administration**, unlike in this case.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** causes thickening of the alveolar-capillary membrane, leading to impaired gas exchange and **diffusion limitation**.
- While it causes hypoxemia, the diffusion studies are stated to be **normal**, and hypoxemia due to diffusion limitation often improves with supplemental oxygen.
*Pulmonary embolism*
- A **pulmonary embolism** leads to V/Q mismatch by blocking blood flow to a portion of the lung, causing ventilation with no perfusion.
- Hypoxemia from V/Q mismatch generally **responds well to supplemental oxygen**, as the non-affected lung areas can compensate, unlike the scenario described.
*Vacation at the top of a mountain*
- Being at a high altitude causes **hypobaric hypoxia**, meaning there is a reduced partial pressure of oxygen in the inspired air.
- This type of hypoxemia typically **improves with supplemental oxygen** as it increases the inspired oxygen tension, which is contrary to the patient's findings.
Integrated respiratory responses US Medical PG Question 2: A 54-year-old man comes to the physician because of excessive daytime sleepiness for 5 months. He wakes up frequently at night, and his wife says his snoring has become louder. He is 180 cm (5 ft 10 in) tall and weighs 104 kg (230 lb); his BMI is 33 kg/m2. His pulse is 80/min and his respiratory rate is 11/min. His jugular venous pressure is 7 cm H2O. He has 2+ pitting edema of the lower legs and ankles. Arterial blood gas analysis on room air shows a pH of 7.42 and a PCO2 of 41 mm Hg. An x-ray of the chest shows normal findings. Which of the following is the most likely underlying cause of this patient's condition?
- A. Daytime alveolar hypoventilation
- B. Decreased levels of hypocretin-1
- C. Increased medullary ventilatory responsiveness
- D. Impaired myocardial relaxation
- E. Intermittent collapse of the oropharynx (Correct Answer)
Integrated respiratory responses Explanation: ***Intermittent collapse of the oropharynx***
- The patient's symptoms of **excessive daytime sleepiness**, frequent night awakenings, and **loud snoring** are classic signs of **obstructive sleep apnea (OSA)**.
- OSA is characterized by the **intermittent collapse of the oropharynx** during sleep, leading to obstructed airflow. His obesity (BMI 33 kg/m2) is a significant risk factor for OSA.
*Daytime alveolar hypoventilation*
- This would typically present with **elevated PCO2** on arterial blood gas, indicating CO2 retention. The patient's PCO2 of 41 mm Hg is within the normal range, ruling out significant daytime alveolar hypoventilation.
- While chronic severe OSA can eventually lead to obesity hypoventilation syndrome, the current ABG does not support this as the primary underlying cause.
*Decreased levels of hypocretin-1*
- **Decreased hypocretin-1** (also known as orexin) levels in the cerebrospinal fluid are a hallmark of **narcolepsy type 1**.
- While narcolepsy causes excessive daytime sleepiness, it is not associated with loud snoring or night awakenings due to respiratory effort, which are prominent in this patient.
*Increased medullary ventilatory responsiveness*
- **Increased medullary ventilatory responsiveness** would lead to an enhanced drive to breathe, often resulting in **hypocapnia (low PCO2)**, especially in response to metabolic acidosis or hypoxemia.
- This is contrary to the patient's normal PCO2 and clinical picture, which points towards an obstructive rather than a central ventilatory issue.
*Impaired myocardial relaxation*
- **Impaired myocardial relaxation** is a feature of **diastolic heart failure**, which could explain the elevated JVP and peripheral edema.
- However, it does not explain the primary presenting symptoms of excessive daytime sleepiness and loud snoring, which point directly to a sleep-related breathing disorder rather than primarily a cardiac issue.
Integrated respiratory responses US Medical PG Question 3: A 3-year-old boy is brought to the emergency department with a history of unintentional ingestion of seawater while swimming in the sea. The amount of seawater ingested is not known. There is no history of vomiting. On physical examination, the boy appears confused and is asking for more water to drink. His serum sodium is 152 mmol/L (152 mEq/L). Which of the following changes in volumes and osmolality of body fluids are most likely to be present in this boy?
- A. Decreased ECF volume, unaltered ICF volume, unaltered body osmolality
- B. Increased ECF volume, decreased ICF volume, increased body osmolality (Correct Answer)
- C. Increased ECF volume, unaltered ICF volume, unaltered body osmolality
- D. Increased ECF volume, increased ICF volume, decreased body osmolality
- E. Decreased ECF volume, decreased ICF volume, increased body osmolality
Integrated respiratory responses Explanation: ***Increased ECF volume, decreased ICF volume, increased body osmolality***
- Ingesting **seawater**, which is **hypertonic** (higher sodium concentration than plasma), leads to an increase in total body osmolality because the ingested sodium is absorbed into the extracellular fluid (ECF). This causes water to shift from the intracellular fluid (ICF) to the ECF to equilibrate osmolality, leading to a **decreased ICF volume** and an **increased ECF volume**, consistent with the patient's **serum sodium of 152 mmol/L**.
- The patient's confusion and excessive thirst ("asking for more water") are classic symptoms of **hypernatremia** and **dehydration** at the cellular level, as cells shrink due to water loss.
*Decreased ECF volume, unaltered ICF volume, unaltered body osmolality*
- This option does not align with the ingestion of **hypertonic seawater**, which would inevitably increase ECF volume and body osmolality due to the absorption of excess sodium.
- An **unaltered ICF volume** and body osmolality would imply no significant osmotic shift or change in solute concentration, which contradicts the clinical picture of hypernatremia.
*Increased ECF volume, unaltered ICF volume, unaltered body osmolality*
- While ECF volume would increase due to fluid shift, the ingested **hypertonic** seawater would significantly **increase body osmolality**, not leave it unaltered.
- An **unaltered ICF volume** is unlikely as the osmotic gradient created by hypernatremia would draw water out of cells.
*Increased ECF volume, increased ICF volume, decreased body osmolality*
- Both **increased ECF and ICF volumes** are inconsistent with the hypernatremia caused by seawater ingestion; hypernatremia typically causes fluid to shift *out* of cells, thereby decreasing ICF volume.
- A **decreased body osmolality** would be seen in cases of hyponatremia (excessive water intake or solute loss), which is the opposite of this clinical scenario.
*Decreased ECF volume, decreased ICF volume, increased body osmolality*
- While ICF volume would decrease and body osmolality would increase, the ECF volume is more likely to **increase** initially due to the ingested volume of seawater and the subsequent osmotic shift of water from the ICF.
- A **decreased ECF volume** would typically occur only with massive dehydration or severe fluid loss, not with the ingestion of a significant amount of fluid, even if hypertonic.
Integrated respiratory responses US Medical PG Question 4: A 17-year-old previously healthy, athletic male suddenly falls unconscious while playing soccer. His athletic trainer comes to his aid and notes that he is pulseless. He begins performing CPR on the patient until the ambulance arrives but the teenager is pronounced dead when the paramedics arrived. Upon investigation of his primary care physician's office notes, it was found that the child had a recognized murmur that was ruled to be "benign." Which of the following conditions would have increased the intensity of the murmur?
- A. Inspiration
- B. Placing the patient in a squatting position
- C. Valsalva (Correct Answer)
- D. Passive leg raise
- E. Handgrip
Integrated respiratory responses Explanation: ***Valsalva***
- The patient's sudden death after collapsing during soccer, coupled with a previously noted "benign" murmur, strongly suggests **hypertrophic obstructive cardiomyopathy (HOCM)**, which is a common cause of sudden cardiac death in young athletes. The **Valsalva maneuver** decreases preload and left ventricular volume, thereby **increasing the left ventricular outflow tract (LVOT) obstruction** and hence the intensity of the HOCM murmur.
- This maneuver reduces venous return to the heart, leading to reduced ventricular filling and decreased stroke volume. This exacerbates the obstruction in HOCM, making the murmur louder.
*Inspiration*
- **Inspiration** typically **increases venous return to the right side of the heart**, which would generally intensify right-sided murmurs (e.g., tricuspid regurgitation).
- It would have **minimal effect or slightly decrease** the intensity of a left-sided obstructive murmur like that in HOCM, as it does not directly increase the LVOT obstruction.
*Placing the patient in a squatting position*
- Squatting increases both **preload** and **afterload** by increasing systemic vascular resistance and venous return.
- This increase in ventricular volume would **reduce the outflow tract obstruction** in HOCM, thereby **decreasing the intensity of the murmur**.
*Passive leg raise*
- A **passive leg raise** increases **venous return** and thus **preload**, leading to increased ventricular filling.
- Similar to squatting, this increased left ventricular volume would **reduce the left ventricular outflow tract obstruction** associated with HOCM, thereby **decreasing the murmur's intensity**.
*Handgrip*
- The **handgrip maneuver** primarily **increases afterload** and, to some extent, preload by increasing systemic vascular resistance.
- While it can increase the intensity of murmurs like mitral regurgitation and ventricular septal defect, it would generally **decrease or have no significant effect** on the murmur of HOCM due to the increased ventricular volume reducing the outflow obstruction.
Integrated respiratory responses US Medical PG Question 5: An investigator is studying muscle tissue in high-performance athletes. He obtains blood samples from athletes before and after a workout session consisting of short, fast sprints. Which of the following findings is most likely upon evaluation of blood obtained after the workout session?
- A. Decreased concentration of NADH
- B. Increased concentration of H+ (Correct Answer)
- C. Decreased concentration of lactate
- D. Increased concentration of insulin
- E. Increased concentration of ATP
Integrated respiratory responses Explanation: ***Increased concentration of H+***
- During **anaerobic metabolism** in high-intensity exercise like sprints, pyruvate is converted to **lactate** by **lactate dehydrogenase** to regenerate NAD+. This process produces H+, leading to a decrease in pH and an increase in H+ concentration in the blood.
- The accumulation of **hydrogen ions (H+)** contributes to metabolic acidosis, muscle fatigue, and the burning sensation experienced during intense exertion.
- Blood gas analysis would show **decreased pH** and **increased H+ concentration**.
*Decreased concentration of NADH*
- NADH is primarily an **intracellular metabolite** and is not typically measured in blood samples as it does not circulate freely in significant concentrations.
- Within muscle cells during anaerobic glycolysis, NADH is consumed by lactate dehydrogenase to convert pyruvate to lactate, regenerating NAD+ for continued glycolysis.
- This option is not a realistic blood finding from a clinical laboratory perspective.
*Decreased concentration of lactate*
- **High-intensity sprints** primarily rely on **anaerobic metabolism**, which rapidly produces **lactate** from pyruvate.
- Therefore, the concentration of lactate in the blood would significantly **increase** after such a workout, not decrease.
- Elevated blood lactate is a hallmark finding after intense anaerobic exercise.
*Increased concentration of insulin*
- **Insulin** levels typically **decrease** during exercise, especially high-intensity exercise, due to **sympathetic nervous system activation** and the body's need to mobilize glucose from liver glycogen and fatty acids.
- Exercise promotes glucose uptake through **insulin-independent mechanisms** (GLUT4 translocation via AMP-activated protein kinase).
- Increased insulin would be counterproductive during intense exercise when glucose mobilization is needed.
*Increased concentration of ATP*
- ATP does not circulate in blood in measurable concentrations as a typical laboratory finding.
- Within muscle cells, ATP is rapidly **consumed** during intense exercise to fuel muscle contraction.
- While cells work to maintain ATP levels through anaerobic glycolysis and the creatine phosphate system, net ATP does not accumulate in the blood.
Integrated respiratory responses US Medical PG Question 6: A 27-year-old man is running on the treadmill at his gym. His blood pressure prior to beginning his workout was 110/72. Which of the following changes in his cardiovascular system may be seen in this man now that he is exercising?
- A. Decreased blood pressure
- B. Decreased systemic vascular resistance (Correct Answer)
- C. Increased systemic vascular resistance
- D. Decreased stroke volume
- E. Decreased heart rate
Integrated respiratory responses Explanation: ***Decreased systemic vascular resistance***
- During dynamic exercise, metabolic vasodilation in exercising muscles leads to a substantial **decrease in systemic vascular resistance (SVR)** to accommodate increased blood flow.
- This vasodilation overrides the systemic vasoconstriction driven by the sympathetic nervous system, resulting in a net decrease in overall SVR.
*Decreased blood pressure*
- While SVR decreases, **systolic blood pressure typically increases** during exercise due to increased cardiac output.
- **Diastolic blood pressure** usually remains stable or may slightly decrease, but overall blood pressure, specifically the mean arterial pressure, is generally maintained or elevated.
*Increased systemic vascular resistance*
- This is incorrect as **vasodilation in active muscles** causes a significant decrease in overall systemic vascular resistance.
- An increase in SVR would typically hinder blood flow to working muscles and is not a characteristic cardiovascular response to dynamic exercise.
*Decreased stroke volume*
- Stroke volume generally **increases significantly** during exercise due to enhanced venous return, increased contractility, and reduced afterload (from decreased SVR).
- A decreased stroke volume would limit cardiac output and exercise performance.
*Decreased heart rate*
- Heart rate **increases proportionally with exercise intensity** to boost cardiac output and oxygen delivery to active muscles.
- A decreased heart rate would counteract the body's physiological demand for increased blood flow during physical activity.
Integrated respiratory responses US Medical PG Question 7: A 37-year-old G1P0 woman presents to her primary care physician for a routine checkup. She has a history of diabetes and hypertension but has otherwise been healthy with no change in her health status since the last visit. She is expecting her first child 8 weeks from now. She also enrolled in a study about pregnancy where serial metabolic panels and arterial blood gases are obtained. Partial results from these studies are shown below:
Serum:
Na+: 141 mEq/L
Cl-: 108 mEq/L
pH: 7.47
pCO2: 30 mmHg
HCO3-: 21 mEq/L
Which of the following disease processes would most likely present with a similar panel of metabolic results?
- A. Diarrheal disease
- B. Loop diuretic abuse
- C. Living at high altitude (Correct Answer)
- D. Ingestion of metformin
- E. Anxiety attack
Integrated respiratory responses Explanation: ***Living at high altitude***
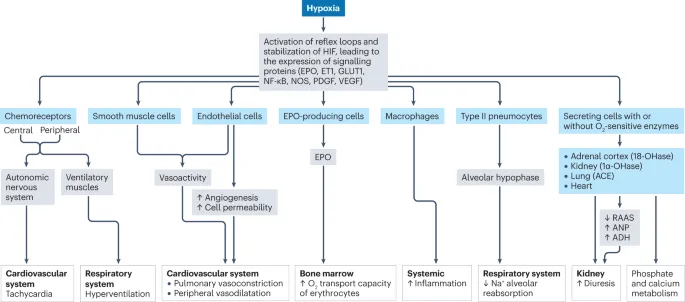
- Chronic exposure to **high altitude** leads to sustained **hypoxia**, which stimulates **hyperventilation** as a compensatory mechanism.
- This persistent hyperventilation causes a **respiratory alkalosis** (high pH, low pCO2) and a compensatory **metabolic acidosis** (low HCO3-) to normalize pH, mimicking the presented metabolic panel.
*Diarrheal disease*
- Severe **diarrhea** leads to the loss of bicarbonate from the gastrointestinal tract, causing a **non-anion gap metabolic acidosis**.
- This would present with a **low pH**, **low HCO3-**, and a **compensatory drop in pCO2**, not a respiratory alkalosis with a high pH.
*Loop diuretic abuse*
- Chronic abuse of **loop diuretics** can cause **metabolic alkalosis** due to increased renal excretion of hydrogen ions and potassium, leading to volume contraction.
- This would typically present with a **high pH**, high HCO3-, and a compensatory rise in pCO2, which is different from the given values.
*Ingestion of metformin*
- **Metformin** can cause **lactic acidosis** (a type of high anion gap metabolic acidosis), especially in patients with renal impairment.
- This would manifest as a **low pH**, **low HCO3-**, and a **compensatory decrease in pCO2**, along with an elevated anion gap, not the respiratory alkalosis seen here.
*Anxiety attack*
- An **anxiety attack** causes acute **hyperventilation**, leading to **acute respiratory alkalosis** (high pH, low pCO2).
- However, in an acute setting, there is insufficient time for significant renal compensation, so the HCO3- would remain near normal, unlike the compensated state shown in the panel.
Integrated respiratory responses US Medical PG Question 8: A 60-year-old woman with a history of emphysema has been referred by her pulmonologist for follow-up pulmonary function testing. During the test, the patient reaches a point where her airway pressure is equal to the atmospheric pressure. Which of the following is most likely to be found during this respiratory state?
- A. Pulmonary vascular resistance is at a maximum
- B. Transmural pressure of the lung-chest wall system is at a maximum
- C. Transmural pressure of the chest wall is at a minimum
- D. Pulmonary vascular resistance is at a minimum (Correct Answer)
- E. Transmural pressure of the lung-chest wall system is at a minimum
Integrated respiratory responses Explanation: ***Pulmonary vascular resistance is at a minimum***
- When airway pressure equals atmospheric pressure during a pulmonary function test, the lungs are at **functional residual capacity (FRC)** or resting state.
- At FRC, **pulmonary vascular resistance (PVR)** is at its lowest point due to the optimal balance between alveolar and extra-alveolar vessel compression/distension.
- Extra-alveolar vessels are compressed at low lung volumes, while alveolar vessels are compressed at high lung volumes. At FRC, both are optimally distended, resulting in **minimal PVR**.
*Pulmonary vascular resistance is at a maximum*
- PVR increases at very low lung volumes (due to extra-alveolar vessel compression) and very high lung volumes (due to alveolar vessel compression).
- The resting state (airway pressure equals atmospheric pressure) corresponds to FRC, where PVR is **minimal, not maximal**.
*Transmural pressure of the lung-chest wall system is at a maximum*
- Transmural pressure of the lung-chest wall system represents the pressure difference across the entire respiratory system.
- This pressure is higher during inspiration or forced expiration when the system is stretched or compressed.
- At FRC (airway pressure equals atmospheric pressure), the system is at **resting equilibrium**, not at maximal transmural pressure.
*Transmural pressure of the chest wall is at a minimum*
- Transmural pressure across the chest wall is the difference between intrapleural pressure and atmospheric pressure.
- This pressure is not at a minimum when airway pressure equals atmospheric pressure.
- Chest wall transmural pressure is actually minimal near **residual volume (RV)**, where the chest wall recoils inward most strongly.
*Transmural pressure of the lung-chest wall system is at a minimum*
- Transmural pressure of the lung-chest wall system reflects the elastic recoil forces of the combined system.
- At FRC (airway pressure equals atmospheric pressure), elastic recoil forces are balanced at equilibrium, but transmural pressure is **not at a minimum**—it represents the neutral resting state.
Integrated respiratory responses US Medical PG Question 9: A 15-year-old boy and his mother were referred to a pulmonology clinic. She is concerned that her son is having some breathing difficulty for the past few months, which is aggravated with exercise. The family is especially concerned because the patient’s older brother has cystic fibrosis. The past medical history is noncontributory. Today, the vital signs include: blood pressure 119/80 mm Hg, heart rate 90/min, respiratory rate 17/min, and temperature 37.0°C (98.6°F). On physical exam, he appears well-developed and well-nourished. The heart has a regular rate and rhythm, and the lungs are clear to auscultation bilaterally. During the exam, he is brought into a special room to test his breathing. A clamp is placed on his nose and he is asked to take in as much air as he can, and then forcefully expire all the air into a spirometer. The volume of expired air represents which of the following?
- A. Tidal volume
- B. Total lung capacity
- C. Functional residual capacity
- D. Expiratory reserve volume
- E. Vital capacity (Correct Answer)
Integrated respiratory responses Explanation: ***Vital capacity***
- **Vital capacity (VC)** is the maximum volume of air exhaled after a maximal inspiration. The maneuver described ("take in as much air as he can, and then forcefully expire all the air") directly measures vital capacity.
- VC includes the **tidal volume (TV)**, **inspiratory reserve volume (IRV)**, and **expiratory reserve volume (ERV)**.
*Tidal volume*
- **Tidal volume (TV)** is the volume of air inspired or expired with a normal breath, not the maximal forceful expiration described.
- It represents the usual volume of air exchanged during quiet breathing.
*Total lung capacity*
- **Total lung capacity (TLC)** is the maximum volume of air that the lungs can hold after a maximal inspiration, including the residual volume.
- This cannot be measured directly by spirometry alone, as it includes the **residual volume** which is the air remaining in the lungs after maximal expiration.
*Functional residual capacity*
- **Functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal, quiet expiration.
- Like TLC and residual volume, FRC cannot be measured directly by standard spirometry.
*Expiratory reserve volume*
- **Expiratory reserve volume (ERV)** is the maximum volume of air that can be *additionally* exhaled after a normal exhalation.
- The patient was asked to expire all the air after a maximal inspiration, which is a measure of vital capacity, not just ERV.
Integrated respiratory responses US Medical PG Question 10: A 35-year-old woman volunteers for a study on respiratory physiology. Pressure probes A and B are placed as follows:
Probe A: between the parietal and visceral pleura
Probe B: within the cavity of an alveolus
The probes provide a pressure reading relative to atmospheric pressure. To obtain a baseline reading, she is asked to sit comfortably and breathe normally. Which of the following sets of values will most likely be seen at the end of inspiration?
- A. Probe A: -6 mm Hg; Probe B: 0 mm Hg (Correct Answer)
- B. Probe A: 0 mm Hg; Probe B: -1 mm Hg
- C. Probe A: -4 mm Hg; Probe B: 0 mm Hg
- D. Probe A: -4 mm Hg; Probe B: -1 mm Hg
- E. Probe A: -6 mm Hg; Probe B: -1 mm Hg
Integrated respiratory responses Explanation: ***Probe A: -6 mm Hg; Probe B: 0 mm Hg***
- At the **end of inspiration**, the **intrapleural pressure (Probe A)** is at its most negative, typically around -6 to -8 cm H2O (equivalent to -4 to -6 mmHg), reflecting the maximum expansion of the thoracic cavity.
- At the **end of inspiration**, just before exhalation begins, there is **no airflow**, so the **intrapulmonary pressure (Probe B)** equalizes with atmospheric pressure, resulting in a 0 mm Hg reading.
*Probe A: 0 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of 0 mm Hg** would indicate a **pneumothorax** since it should always be negative to prevent lung collapse.
- An **intrapulmonary pressure of -1 mm Hg** would indicate that **inspiration is still ongoing**, as air would be flowing into the lungs.
*Probe A: -4 mm Hg; Probe B: 0 mm Hg*
- While an **intrapulmonary pressure of 0 mm Hg** is correct at the end of inspiration, an **intrapleural pressure of -4 mm Hg** is typical for the **end of expiration (Functional Residual Capacity)** during quiet breathing, not the end of inspiration.
- The **intrapleural pressure becomes more negative** during inspiration due to increased thoracic volume, so -4 mm Hg would be insufficient.
*Probe A: -4 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of -4 mm Hg** is the normal pressure at the **end of expiration**, not the end of inspiration, where it becomes more negative.
- An **intrapulmonary pressure of -1 mm Hg** indicates that **inspiration is still in progress**, not at its end, as air would still be flowing into the lungs.
*Probe A: -6 mm Hg; Probe B: -1 mm Hg*
- While an **intrapleural pressure of -6 mm Hg** is consistent with the end of inspiration, an **intrapulmonary pressure of -1 mm Hg** means that **airflow is still occurring into the lungs**.
- At the **very end of inspiration**, just before the start of exhalation, airflow momentarily ceases, and intrapulmonary pressure becomes zero relative to the atmosphere.
More Integrated respiratory responses US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.