Exercise respiratory physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Exercise respiratory physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
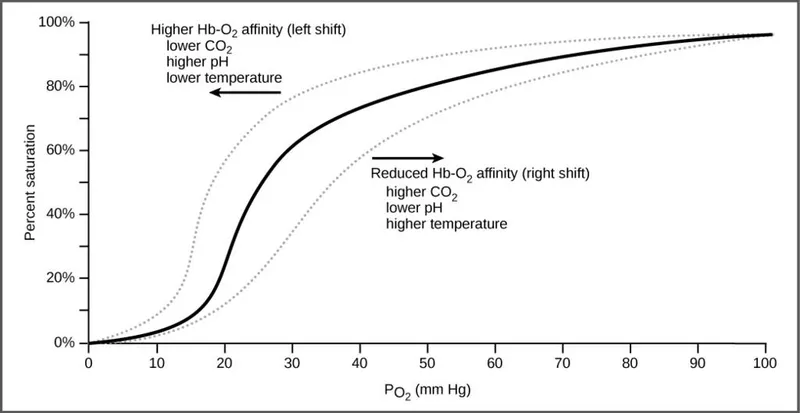
Exercise respiratory physiology US Medical PG Question 1: A 24-year-old professional athlete is advised to train in the mountains to enhance his performance. After 5 months of training at an altitude of 1.5 km (5,000 feet), he is able to increase his running pace while competing at sea-level venues. Which of the following changes would produce the same effect on the oxygen-hemoglobin dissociation curve as this athlete's training did?
- A. Decreased 2,3-bisphosphoglycerate (Correct Answer)
- B. Increased carbon monoxide inhalation
- C. Decreased temperature
- D. Decreased pH
- E. Increased partial pressure of oxygen
Exercise respiratory physiology Explanation: ***Decreased 2,3-bisphosphoglycerate***
- This is **NOT** the correct physiological adaptation from altitude training, making this question conceptually flawed.
- Altitude training causes **increased erythropoietin → polycythemia → increased total hemoglobin**, which increases oxygen-carrying capacity.
- 2,3-BPG is **initially increased** at altitude (right shift) to facilitate O2 release, and remains elevated or returns to normal with acclimatization, **not decreased**.
- While decreased 2,3-BPG would cause a left shift (increased O2 affinity), this does NOT replicate altitude training adaptations.
*Increased carbon monoxide inhalation*
- Carbon monoxide binds hemoglobin with **200-250× higher affinity** than oxygen, forming carboxyhemoglobin.
- This **reduces oxygen-carrying capacity** and causes a left shift for remaining hemoglobin.
- This is harmful and does NOT replicate beneficial altitude adaptations.
*Decreased temperature*
- Decreases metabolic rate and causes a **left shift** (increased O2 affinity).
- Oxygen is held more tightly and released less readily to tissues.
- This does NOT replicate altitude training benefits.
*Decreased pH*
- Acidosis causes the **Bohr effect**: **right shift** (decreased O2 affinity).
- Facilitates O2 release to tissues during exercise.
- This is beneficial during exercise but does NOT replicate the chronic altitude adaptation of increased oxygen-carrying capacity.
*Increased partial pressure of oxygen*
- Higher PO2 increases hemoglobin saturation but does NOT shift the curve.
- This increases oxygen availability but does NOT replicate the physiological adaptation (polycythemia) from altitude training.
**Note:** This question is conceptually problematic as none of the options accurately replicate the primary altitude training adaptation (increased RBC mass/hemoglobin concentration).
Exercise respiratory physiology US Medical PG Question 2: During exercise, what is the primary mechanism for increased oxygen delivery to active muscles?
- A. Decreased blood viscosity
- B. Increased cardiac output (Correct Answer)
- C. Increased hemoglobin affinity
- D. Enhanced oxygen diffusion
Exercise respiratory physiology Explanation: ***Increased cardiac output***
- During exercise, **cardiac output** increases significantly due to both an elevated **heart rate** and increased **stroke volume**, directly pushing more oxygenated blood to the active muscles.
- This augmentation in blood flow is the primary factor ensuring a sufficient supply of oxygen and nutrients to meet the heightened metabolic demands of exercising muscles.
*Decreased blood viscosity*
- While factors like **hemodilution** can decrease blood viscosity during prolonged exercise, this effect is relatively minor and not the primary mechanism for acute increases in oxygen delivery compared to the dramatic increase in cardiac output.
- A decrease in blood viscosity can slightly improve flow efficiency, but it doesn't fundamentally change the amount of blood pumped per minute to the muscles.
*Increased hemoglobin affinity*
- An *increased* hemoglobin affinity for oxygen would actually make it *harder* for oxygen to unload from hemoglobin to the tissues, which is counterproductive for oxygen delivery during exercise.
- In fact, during exercise, local conditions like increased temperature, decreased pH (**Bohr effect**), and increased 2,3-BPG tend to *decrease* hemoglobin's affinity for oxygen, facilitating oxygen release to active muscles.
*Enhanced oxygen diffusion*
- While exercise does improve the efficiency of oxygen extraction at the tissue level due to a steeper partial pressure gradient and increased capillary recruitment, the *rate* of oxygen diffusion across the capillary membrane isn't the primary modulator of overall oxygen delivery.
- The main determinant is the *amount* of oxygenated blood reaching the muscle, which is governed by cardiac output and local blood flow regulation.
Exercise respiratory physiology US Medical PG Question 3: A 60-year-old male engineer who complains of shortness of breath when walking a few blocks undergoes a cardiac stress test because of concern for coronary artery disease. During the test he asks his cardiologist about what variables are usually used to quantify the functioning of the heart. He learns that one of these variables is stroke volume. Which of the following scenarios would be most likely to lead to a decrease in stroke volume?
- A. Anxiety
- B. Heart failure (Correct Answer)
- C. Exercise
- D. Pregnancy
- E. Digitalis
Exercise respiratory physiology Explanation: ***Heart failure***
- In **heart failure**, the heart's pumping ability is impaired, leading to a reduced **ejection fraction** and thus a decreased **stroke volume**.
- The weakened myocardium cannot effectively contract to expel the normal volume of blood, resulting in lower blood output per beat.
*Anxiety*
- **Anxiety** typically causes an increase in **sympathetic nervous system** activity, leading to increased heart rate and myocardial contractility.
- This often results in a temporary **increase in stroke volume** due to enhanced cardiac performance, not a decrease.
*Exercise*
- During **exercise**, there is a significant **increase in venous return** and sympathetic stimulation, leading to increased **end-diastolic volume** and contractility.
- This physiological response causes a substantial **increase in stroke volume** to meet the body's higher oxygen demands.
*Pregnancy*
- **Pregnancy** leads to significant **physiological adaptations** to accommodate the growing fetus, including a substantial increase in **blood volume**.
- This increased blood volume and cardiac output result in an **increase in stroke volume** to maintain adequate perfusion for both mother and fetus.
*Digitalis*
- **Digitalis** is a cardiac glycoside that **increases intracellular calcium** in myocardial cells, enhancing the **force of contraction**.
- This positive inotropic effect leads to an **increased stroke volume** by improving the heart's pumping efficiency.
Exercise respiratory physiology US Medical PG Question 4: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Exercise respiratory physiology Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
*Myogenic response*
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
Exercise respiratory physiology US Medical PG Question 5: A 32-year-old woman comes to the physician for a screening health examination that is required for scuba diving certification. The physician asks her to perform a breathing technique: following deep inspiration, she is instructed to forcefully exhale against a closed airway and contract her abdominal muscles while different cardiovascular parameters are evaluated. Which of the following effects is most likely after 10 seconds in this position?
- A. Decreased intra-abdominal pressure
- B. Decreased left ventricular stroke volume (Correct Answer)
- C. Decreased pulse rate
- D. Decreased systemic vascular resistance
- E. Increased venous return to left atrium
Exercise respiratory physiology Explanation: ***Decreased left ventricular stroke volume***
- After 10 seconds of performing the **Valsalva maneuver**, the increased intrathoracic pressure significantly reduces **venous return** to the heart.
- Reduced venous return leads to decreased **ventricular filling** (preload), which in turn diminishes **left ventricular stroke volume** and cardiac output.
*Decreased intra-abdominal pressure*
- The instruction to "contract her abdominal muscles" during forceful exhalation against a closed airway (Valsalva maneuver) directly leads to an **increase** in **intra-abdominal pressure**, not a decrease.
- This increase in intra-abdominal pressure further impedes venous return from the lower extremities to the heart.
*Decreased pulse rate*
- In the initial phase of the Valsalva maneuver (first 5-10 seconds), the decrease in cardiac output triggers a **reflex tachycardia** to maintain blood pressure, leading to an **increased pulse rate**.
- A decrease in pulse rate (bradycardia) is more characteristic of the release phase, not during the sustained strain.
*Decreased systemic vascular resistance*
- During the Valsalva maneuver, the body attempts to compensate for the drop in cardiac output and blood pressure by increasing **sympathetic tone**, which causes **vasoconstriction** and thus **increases systemic vascular resistance**.
- A decrease in systemic vascular resistance would further drop blood pressure and is not the physiological response during this phase.
*Increased venous return to left atrium*
- The Valsalva maneuver dramatically **reduces venous return** to both the right and left atria due to the high intrathoracic pressure compressing the great veins.
- This decreased venous return is the primary mechanism leading to the subsequent fall in cardiac output during the maneuver.
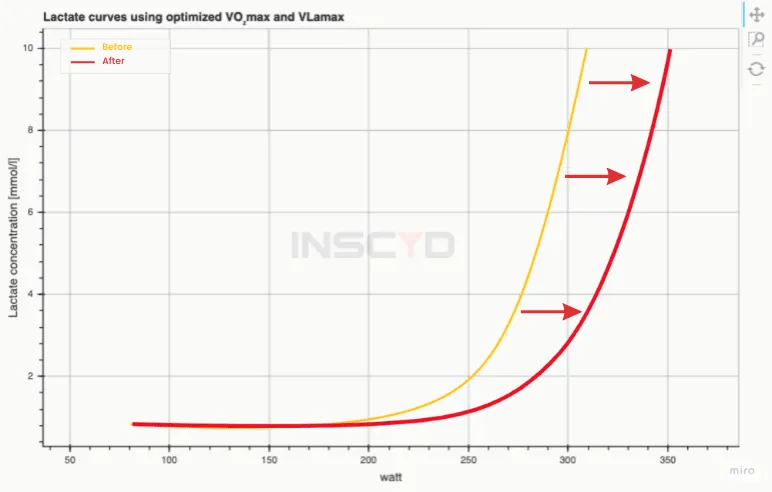
Exercise respiratory physiology US Medical PG Question 6: An investigator is studying muscle tissue in high-performance athletes. He obtains blood samples from athletes before and after a workout session consisting of short, fast sprints. Which of the following findings is most likely upon evaluation of blood obtained after the workout session?
- A. Decreased concentration of NADH
- B. Increased concentration of H+ (Correct Answer)
- C. Decreased concentration of lactate
- D. Increased concentration of insulin
- E. Increased concentration of ATP
Exercise respiratory physiology Explanation: ***Increased concentration of H+***
- During **anaerobic metabolism** in high-intensity exercise like sprints, pyruvate is converted to **lactate** by **lactate dehydrogenase** to regenerate NAD+. This process produces H+, leading to a decrease in pH and an increase in H+ concentration in the blood.
- The accumulation of **hydrogen ions (H+)** contributes to metabolic acidosis, muscle fatigue, and the burning sensation experienced during intense exertion.
- Blood gas analysis would show **decreased pH** and **increased H+ concentration**.
*Decreased concentration of NADH*
- NADH is primarily an **intracellular metabolite** and is not typically measured in blood samples as it does not circulate freely in significant concentrations.
- Within muscle cells during anaerobic glycolysis, NADH is consumed by lactate dehydrogenase to convert pyruvate to lactate, regenerating NAD+ for continued glycolysis.
- This option is not a realistic blood finding from a clinical laboratory perspective.
*Decreased concentration of lactate*
- **High-intensity sprints** primarily rely on **anaerobic metabolism**, which rapidly produces **lactate** from pyruvate.
- Therefore, the concentration of lactate in the blood would significantly **increase** after such a workout, not decrease.
- Elevated blood lactate is a hallmark finding after intense anaerobic exercise.
*Increased concentration of insulin*
- **Insulin** levels typically **decrease** during exercise, especially high-intensity exercise, due to **sympathetic nervous system activation** and the body's need to mobilize glucose from liver glycogen and fatty acids.
- Exercise promotes glucose uptake through **insulin-independent mechanisms** (GLUT4 translocation via AMP-activated protein kinase).
- Increased insulin would be counterproductive during intense exercise when glucose mobilization is needed.
*Increased concentration of ATP*
- ATP does not circulate in blood in measurable concentrations as a typical laboratory finding.
- Within muscle cells, ATP is rapidly **consumed** during intense exercise to fuel muscle contraction.
- While cells work to maintain ATP levels through anaerobic glycolysis and the creatine phosphate system, net ATP does not accumulate in the blood.
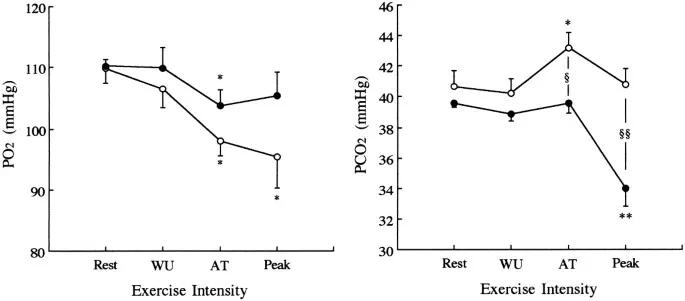
Exercise respiratory physiology US Medical PG Question 7: During heavy exercise, what is the primary mechanism for maintaining arterial pH despite increased lactic acid production?
- A. Increased bicarbonate reabsorption
- B. Phosphate buffering
- C. Increased hydrogen secretion
- D. Hyperventilation (Correct Answer)
Exercise respiratory physiology Explanation: ***Hyperventilation***
- **Hyperventilation** during heavy exercise increases the expulsion of **carbon dioxide (CO2)**, shifting the **bicarbonate buffer system** equilibrium to the left.
- This reduction in **CO2** effectively removes **hydrogen ions (H+)**, thereby helping to maintain **arterial pH** despite rising **lactic acid** levels.
*Increased bicarbonate reabsorption*
- While the kidneys adapt by increasing **bicarbonate reabsorption** to compensate for acidosis, this is a **slower renal mechanism** for pH regulation, taking hours to days, rather than an immediate response during acute exercise.
- The rapid pH regulation during exercise primarily relies on respiratory and chemical buffer systems, not renal function.
*Phosphate buffering*
- The **phosphate buffer system** is indeed important for intracellular and renal tubular fluid buffering.
- However, its buffering capacity in the extracellular fluid and plasma is relatively limited compared to the **bicarbonate system** due to its lower concentration.
*Increased hydrogen secretion*
- **Increased hydrogen secretion** by the renal tubules is a long-term mechanism for compensating for acidosis, which helps excrete excess **acid** and regenerate **bicarbonate**.
- This is a slow, renal regulatory process and not the primary rapid mechanism for maintaining pH during the immediate demands of heavy exercise.
Exercise respiratory physiology US Medical PG Question 8: A person is exercising strenuously on a treadmill for 1 hour. An arterial blood gas measurement is then taken. Which of the following are the most likely values?
- A. pH 7.56, PaO2 100, PCO2 44, HCO3 38
- B. pH 7.32, PaO2 42, PCO2 50, HCO3 27
- C. pH 7.57 PaO2 100, PCO2 23, HCO3 21 (Correct Answer)
- D. pH 7.38, PaO2 100, PCO2 69 HCO3 42
- E. pH 7.36, PaO2 100, PCO2 40, HCO3 23
Exercise respiratory physiology Explanation: ***pH 7.57, PaO2 100, PCO2 23, HCO3 21***
- After 1 hour of strenuous exercise, this represents **respiratory alkalosis with mild metabolic compensation**, which is the expected finding in a healthy individual during sustained vigorous exercise.
- The **low PCO2 (23 mmHg)** reflects appropriate **hyperventilation** in response to increased metabolic demands and lactic acid production. During intense exercise, minute ventilation increases dramatically, often exceeding the rate of CO2 production.
- The **slightly elevated pH (7.57)** and **mildly decreased HCO3 (21 mEq/L)** indicate that respiratory compensation has slightly overshot, creating mild alkalosis, while the bicarbonate is consumed both in buffering lactate and through renal compensation.
- **Normal PaO2 (100 mmHg)** confirms adequate oxygenation maintained by increased ventilation.
*pH 7.36, PaO2 100, PCO2 40, HCO3 23*
- These are **completely normal arterial blood gas values** with no evidence of any physiological stress or compensation.
- After 1 hour of strenuous exercise, we would expect **hyperventilation with decreased PCO2**, not a normal PCO2 of 40 mmHg. This profile would be consistent with rest, not vigorous exercise.
- The absence of any respiratory or metabolic changes makes this inconsistent with the clinical scenario.
*pH 7.56, PaO2 100, PCO2 44, HCO3 38*
- This profile suggests **metabolic alkalosis** (high pH, high HCO3) with inadequate respiratory compensation (normal to slightly elevated PCO2).
- This is **not consistent with strenuous exercise**, which produces metabolic acid (lactate), not metabolic base. The elevated HCO3 suggests vomiting, diuretic use, or other causes of metabolic alkalosis.
*pH 7.32, PaO2 42, PCO2 50, HCO3 27*
- This indicates **respiratory acidosis** (low pH, high PCO2) with **severe hypoxemia** (PaO2 42 mmHg).
- During strenuous exercise, healthy individuals **increase ventilation** to enhance O2 delivery and remove CO2, so both hypoxemia and hypercapnia are unexpected and would suggest severe cardiopulmonary disease or hypoventilation.
*pH 7.38, PaO2 100, PCO2 69, HCO3 42*
- This demonstrates **compensated respiratory acidosis** (normal pH, markedly elevated PCO2 and HCO3).
- The **very high PCO2 (69 mmHg)** indicates severe **hypoventilation**, which is the opposite of what occurs during exercise. This profile suggests chronic respiratory failure with metabolic compensation, such as in severe COPD.
Exercise respiratory physiology US Medical PG Question 9: A 35-year-old woman volunteers for a study on respiratory physiology. Pressure probes A and B are placed as follows:
Probe A: between the parietal and visceral pleura
Probe B: within the cavity of an alveolus
The probes provide a pressure reading relative to atmospheric pressure. To obtain a baseline reading, she is asked to sit comfortably and breathe normally. Which of the following sets of values will most likely be seen at the end of inspiration?
- A. Probe A: -6 mm Hg; Probe B: 0 mm Hg (Correct Answer)
- B. Probe A: 0 mm Hg; Probe B: -1 mm Hg
- C. Probe A: -4 mm Hg; Probe B: 0 mm Hg
- D. Probe A: -4 mm Hg; Probe B: -1 mm Hg
- E. Probe A: -6 mm Hg; Probe B: -1 mm Hg
Exercise respiratory physiology Explanation: ***Probe A: -6 mm Hg; Probe B: 0 mm Hg***
- At the **end of inspiration**, the **intrapleural pressure (Probe A)** is at its most negative, typically around -6 to -8 cm H2O (equivalent to -4 to -6 mmHg), reflecting the maximum expansion of the thoracic cavity.
- At the **end of inspiration**, just before exhalation begins, there is **no airflow**, so the **intrapulmonary pressure (Probe B)** equalizes with atmospheric pressure, resulting in a 0 mm Hg reading.
*Probe A: 0 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of 0 mm Hg** would indicate a **pneumothorax** since it should always be negative to prevent lung collapse.
- An **intrapulmonary pressure of -1 mm Hg** would indicate that **inspiration is still ongoing**, as air would be flowing into the lungs.
*Probe A: -4 mm Hg; Probe B: 0 mm Hg*
- While an **intrapulmonary pressure of 0 mm Hg** is correct at the end of inspiration, an **intrapleural pressure of -4 mm Hg** is typical for the **end of expiration (Functional Residual Capacity)** during quiet breathing, not the end of inspiration.
- The **intrapleural pressure becomes more negative** during inspiration due to increased thoracic volume, so -4 mm Hg would be insufficient.
*Probe A: -4 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of -4 mm Hg** is the normal pressure at the **end of expiration**, not the end of inspiration, where it becomes more negative.
- An **intrapulmonary pressure of -1 mm Hg** indicates that **inspiration is still in progress**, not at its end, as air would still be flowing into the lungs.
*Probe A: -6 mm Hg; Probe B: -1 mm Hg*
- While an **intrapleural pressure of -6 mm Hg** is consistent with the end of inspiration, an **intrapulmonary pressure of -1 mm Hg** means that **airflow is still occurring into the lungs**.
- At the **very end of inspiration**, just before the start of exhalation, airflow momentarily ceases, and intrapulmonary pressure becomes zero relative to the atmosphere.
Exercise respiratory physiology US Medical PG Question 10: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Exercise respiratory physiology Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
More Exercise respiratory physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.