Dyspnea mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Dyspnea mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Dyspnea mechanisms US Medical PG Question 1: A 21-year-old man presents to his physician because he has been feeling increasingly tired and short of breath at work. He has previously had these symptoms but cannot recall the diagnosis he was given. Chart review reveals the following results:
Oxygen tension in inspired air = 150 mmHg
Alveolar carbon dioxide tension = 50 mmHg
Arterial oxygen tension = 71 mmHg
Respiratory exchange ratio = 0.80
Diffusion studies reveal normal diffusion distance. The patient is administered 100% oxygen but the patient's blood oxygen concentration does not improve. Which of the following conditions would best explain this patient's findings?
- A. Septal defect since birth (Correct Answer)
- B. Use of opioid medications
- C. Pulmonary fibrosis
- D. Pulmonary embolism
- E. Vacation at the top of a mountain
Dyspnea mechanisms Explanation: ***Septal defect since birth***
- A congenital heart disease like a **septal defect** causes a right-to-left **shunt**, meaning deoxygenated blood bypasses the lungs and mixes with oxygenated blood.
- This type of shunt leads to **hypoxemia that is refractory to 100% oxygen** because the shunted blood will never pick up oxygen from the lungs.
*Use of opioid medications*
- Opioid use causes **respiratory depression**, leading to **hypoventilation** and increased arterial CO2 with decreased arterial O2.
- However, the hypoxemia from hypoventilation would typically improve significantly with **100% oxygen administration**, unlike in this case.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** causes thickening of the alveolar-capillary membrane, leading to impaired gas exchange and **diffusion limitation**.
- While it causes hypoxemia, the diffusion studies are stated to be **normal**, and hypoxemia due to diffusion limitation often improves with supplemental oxygen.
*Pulmonary embolism*
- A **pulmonary embolism** leads to V/Q mismatch by blocking blood flow to a portion of the lung, causing ventilation with no perfusion.
- Hypoxemia from V/Q mismatch generally **responds well to supplemental oxygen**, as the non-affected lung areas can compensate, unlike the scenario described.
*Vacation at the top of a mountain*
- Being at a high altitude causes **hypobaric hypoxia**, meaning there is a reduced partial pressure of oxygen in the inspired air.
- This type of hypoxemia typically **improves with supplemental oxygen** as it increases the inspired oxygen tension, which is contrary to the patient's findings.
Dyspnea mechanisms US Medical PG Question 2: A 60-year-old woman is brought to the emergency department by her husband because of worsening shortness of breath over the past 2 days. Last week, she had a sore throat and a low-grade fever. She has coughed up white sputum each morning for the past 2 years. She has hypertension and type 2 diabetes mellitus. She has smoked 2 packs of cigarettes daily for 35 years. Current medications include metformin and lisinopril. On examination, she occasionally has to catch her breath between sentences. Her temperature is 38.1°C (100.6°F), pulse is 85/min, respirations are 16/min, and blood pressure is 140/70 mm Hg. Expiratory wheezes with a prolonged expiratory phase are heard over both lung fields. Arterial blood gas analysis on room air shows:
pH 7.33
PCO2 53 mm Hg
PO2 68 mm Hg
An x-ray of the chest shows hyperinflation of bilateral lung fields and flattening of the diaphragm. Which of the following additional findings is most likely in this patient?
- A. Decreased urinary bicarbonate excretion (Correct Answer)
- B. Decreased urinary chloride concentration
- C. Increased serum anion gap
- D. Increased urine osmolar gap
- E. Increased urinary pH
Dyspnea mechanisms Explanation: ***Decreased urinary bicarbonate excretion***
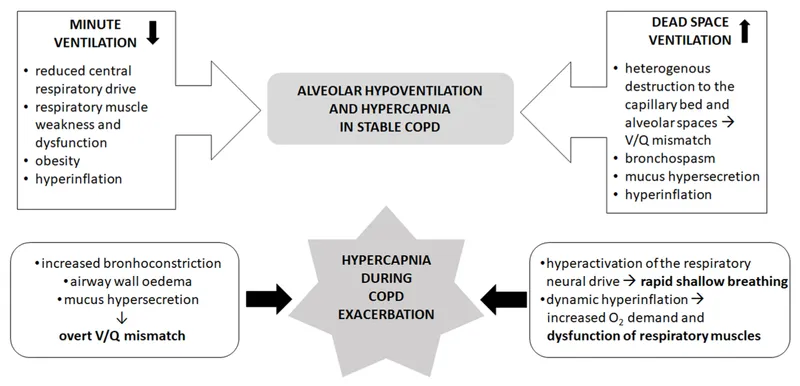
- The patient's ABG results (pH 7.33, PCO2 53 mmHg) indicate **chronic respiratory acidosis**, consistent with a **COPD exacerbation** on a background of chronic disease.
- In chronic respiratory acidosis, the kidneys compensate by **retaining bicarbonate** (increasing reabsorption) and **excreting hydrogen ions** to normalize pH.
- Therefore, urinary bicarbonate excretion is **decreased** as the kidneys conserve bicarbonate to buffer the chronic acidosis.
*Decreased urinary chloride concentration*
- This is typically seen in states of **metabolic alkalosis** (with volume contraction) or profound **volume depletion**, neither of which is the primary condition here.
- The patient has respiratory acidosis, not metabolic alkalosis.
*Increased serum anion gap*
- An increased anion gap indicates **metabolic acidosis** due to accumulation of unmeasured anions (e.g., lactate, ketones, toxins).
- The patient has **respiratory acidosis**, not metabolic acidosis with an anion gap.
- The anion gap is not directly affected by primary respiratory disorders.
*Increased urine osmolar gap*
- An increased urine osmolar gap suggests the presence of **unmeasured osmolytes** in the urine (e.g., from methanol or ethylene glycol ingestion).
- There is nothing in the patient's presentation to suggest toxic ingestion.
*Increased urinary pH*
- Increased urinary pH would occur if the kidneys were **excreting bicarbonate**, which happens in metabolic alkalosis or renal tubular acidosis.
- In chronic respiratory acidosis, the kidneys compensate by **excreting acid** (lowering urinary pH) and **retaining bicarbonate**.
- Therefore, urinary pH would be **decreased**, not increased.
Dyspnea mechanisms US Medical PG Question 3: A 27-year-old woman is admitted to the emergency room with dyspnea which began after swimming and progressed gradually over the last 3 days. She denies cough, chest pain, or other respiratory symptoms. She reports that for the past 4 months, she has had several dyspneic episodes that occurred after the exercising and progressed at rest, but none of these were as long as the current one. Also, she notes that her tongue becomes ‘wadded’ when she speaks and she tires very quickly during the day. The patient’s vital signs are as follows: blood pressure 125/60 mm Hg, heart rate 92/min, respiratory rate 34/min, and body temperature 36.2℃ (97.2℉). Blood saturation on room air is initially 92% but falls to 90% as she speaks up. On physical examination, the patient is slightly lethargic. Her breathing is rapid and shallow. Lung auscultation, as well as cardiac, and abdominal examinations show no remarkable findings. Neurological examination reveals slight bilateral ptosis increased by repetitive blinking, and easy fatigability of muscles on repeated movement worse on the face and distal muscles of the upper and lower extremities. Which arterial blood gas parameters would you expect to see in this patient?
- A. PaCO2 = 51 mm Hg, PaO2 = 58 mm Hg (Correct Answer)
- B. PaCO2 = 37 mm Hg, PaO2 = 46 mm Hg
- C. PaCO2 = 34 mm Hg, PaO2 = 61 mm Hg
- D. PaCO2 = 31 mm Hg, PaO2 = 67 mm Hg
- E. PaCO2 = 43 mm Hg, PaO2 = 55 mm Hg
Dyspnea mechanisms Explanation: ***PaCO2 = 51 mm Hg, PaO2 = 58 mm Hg***
- The patient presents with symptoms highly suggestive of a **myasthenic crisis**, including progressive dyspnea, worsened by exertion (speaking), ptosis, and generalized muscle fatigability. These symptoms indicate **respiratory muscle weakness**, leading to hypoventilation.
- **Hypoventilation** results in **hypercapnia (elevated PaCO2)** and **hypoxemia (decreased PaO2)**. An elevated PaCO2 of 51 mm Hg and decreased PaO2 of 58 mm Hg are consistent with this presentation, reflecting inadequate ventilation.
*PaCO2 = 37 mm Hg, PaO2= 46 mm Hg*
- A PaCO2 of 37 mm Hg is within the normal range or slightly low, suggesting that the patient is not significantly hypercapnic, which contradicts the clinical picture of **respiratory muscle weakness and hypoventilation**.
- While PaO2 is significantly low at 46 mm Hg (indicating hypoxemia), the normal/low PaCO2 would point to a primary **oxygenation defect** (e.g., V/Q mismatch) rather than a ventilatory failure.
*PaCO2 = 34 mm Hg, PaO2 = 61 mm Hg*
- A PaCO2 of 34 mm Hg indicates **hypocapnia**, which is more consistent with hyperventilation rather than the hypoventilation expected from **respiratory muscle weakness** in myasthenic crisis.
- While PaO2 of 61 mm Hg indicates hypoxemia, the accompanying hypocapnia suggests a primary **respiratory drive issue** or conditions causing hyperventilation, not ventilatory failure due to muscle weakness.
*PaCO2 = 31 mm Hg, PaO2 = 67 mm Hg*
- A PaCO2 of 31 mm Hg reflects significant **hypocapnia**, indicating that the patient is **hyperventilating**. This is contrary to what would be expected in a myasthenic crisis where respiratory muscle weakness leads to hypoventilation.
- While PaO2 is decreased, suggesting some respiratory compromise, the ventilatory pattern (hypocapnia) does not match the clinical syndrome of **respiratory muscle fatigue**.
*PaCO2 = 43 mm Hg, PaO2 = 55 mm Hg*
- A PaCO2 of 43 mm Hg is within the **normal reference range**, which would mean there is no CO2 retention and thus no obvious **alveolar hypoventilation** from respiratory muscle weakness.
- While PaO2 of 55 mm Hg indicates hypoxemia, the normal PaCO2 suggests that the hypoxemia is due to other causes like a **V/Q mismatch** rather than inadequate overall ventilation.
Dyspnea mechanisms US Medical PG Question 4: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Dyspnea mechanisms Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
Dyspnea mechanisms US Medical PG Question 5: During heavy exercise, what is the primary mechanism for maintaining arterial pH despite increased lactic acid production?
- A. Increased bicarbonate reabsorption
- B. Phosphate buffering
- C. Increased hydrogen secretion
- D. Hyperventilation (Correct Answer)
Dyspnea mechanisms Explanation: ***Hyperventilation***
- **Hyperventilation** during heavy exercise increases the expulsion of **carbon dioxide (CO2)**, shifting the **bicarbonate buffer system** equilibrium to the left.
- This reduction in **CO2** effectively removes **hydrogen ions (H+)**, thereby helping to maintain **arterial pH** despite rising **lactic acid** levels.
*Increased bicarbonate reabsorption*
- While the kidneys adapt by increasing **bicarbonate reabsorption** to compensate for acidosis, this is a **slower renal mechanism** for pH regulation, taking hours to days, rather than an immediate response during acute exercise.
- The rapid pH regulation during exercise primarily relies on respiratory and chemical buffer systems, not renal function.
*Phosphate buffering*
- The **phosphate buffer system** is indeed important for intracellular and renal tubular fluid buffering.
- However, its buffering capacity in the extracellular fluid and plasma is relatively limited compared to the **bicarbonate system** due to its lower concentration.
*Increased hydrogen secretion*
- **Increased hydrogen secretion** by the renal tubules is a long-term mechanism for compensating for acidosis, which helps excrete excess **acid** and regenerate **bicarbonate**.
- This is a slow, renal regulatory process and not the primary rapid mechanism for maintaining pH during the immediate demands of heavy exercise.
Dyspnea mechanisms US Medical PG Question 6: A 58-year-old man comes to the physician because of a 5-day history of progressively worsening shortness of breath and fatigue. He has smoked 1 pack of cigarettes daily for 30 years. His pulse is 96/min, respirations are 26/min, and blood pressure is 100/60 mm Hg. An x-ray of the chest is shown. Which of the following is the most likely cause of this patient's findings?
- A. Acute respiratory distress syndrome
- B. Interstitial pneumonia
- C. Tricuspid regurgitation
- D. Pulmonary embolism
- E. Left ventricular failure (Correct Answer)
Dyspnea mechanisms Explanation: ***Left ventricular failure***
- The chest x-ray shows diffuse **pulmonary edema** with **bilateral perihilar infiltrates** and prominent **vascular markings**, classic for **cardiogenic pulmonary edema** due to left ventricular failure.
- The patient's history of smoking, shortness of breath, fatigue, tachypnea, and hypotension are consistent with **acute decompensated heart failure**.
*Acute respiratory distress syndrome*
- While ARDS can cause diffuse pulmonary infiltrates, it's often more peripheral and patchy; the presented image shows a more **central perihilar distribution** typical of pulmonary edema.
- ARDS is usually characterized by a severe inflammatory response, often without the marked **cardiomegaly** that would suggest a primary cardiac cause.
*Interstitial pneumonia*
- Interstitial pneumonia typically presents with **reticular or nodular patterns** on chest x-ray, often with a more chronic course.
- The acute onset and rapid progression of symptoms, along with the specific pattern of pulmonary edema, make interstitial pneumonia less likely.
*Tricuspid regurgitation*
- **Tricuspid regurgitation** primarily affects the right side of the heart, leading to signs of **right heart failure** such as **venous congestion**, **hepatomegaly**, and **peripheral edema**.
- While it can indirectly contribute to pulmonary hypertension and congestion, it would not typically present with this specific appearance of **cardiogenic pulmonary edema** without significant left ventricular involvement.
*Pulmonary embolism*
- A **pulmonary embolism** typically causes **pleural effusions**, areas of **oligemia (Westermark sign)**, or **wedge-shaped infiltrates (Hampton hump)**, but rarely diffuse pulmonary edema.
- The patient's acute symptoms could be consistent with PE, but the x-ray findings are not typical for this condition.
Dyspnea mechanisms US Medical PG Question 7: A 55-year-old man presents with an unremitting cough and swelling of the lower limbs for the past 2 weeks. He says he has had a chronic cough for years, however, he feels it is getting worse. He reports a 30-pack-year smoking history. Physical examination reveals mild central cyanosis and expiratory wheezes throughout the chest. Oxygen therapy is ordered immediately but, soon after administering it, his respiratory rate starts to slow down and he becomes drowsy. Dysfunction of which of the following receptors most likely led to this patient’s current condition?
- A. Pleural pain receptors
- B. Central chemoreceptors
- C. Airway stretch receptors
- D. Pulmonary stretch receptors
- E. Peripheral chemoreceptors (Correct Answer)
Dyspnea mechanisms Explanation: ***Peripheral chemoreceptors***
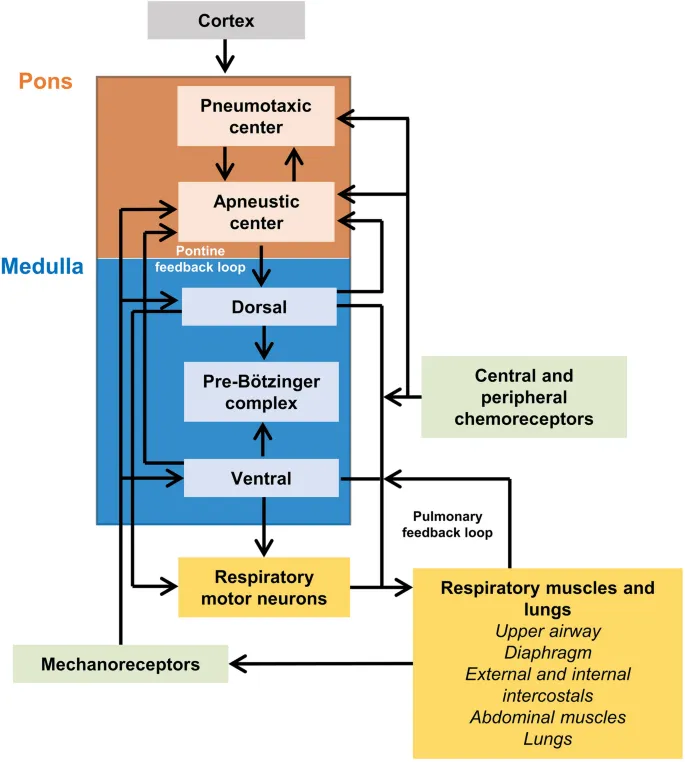
- In patients with chronic obstructive pulmonary disease (COPD) like this patient, the **central chemoreceptors** become desensitized to chronically elevated CO2 levels. Their primary respiratory drive then shifts to the **peripheral chemoreceptors** (carotid and aortic bodies), which are sensitive to **hypoxia**.
- Administering high-flow oxygen **eliminates the hypoxic stimulus** sensed by these normally functioning peripheral chemoreceptors, removing the hypoxic drive to breathe and leading to **hypoventilation, CO2 retention, respiratory acidosis**, and drowsiness (CO2 narcosis).
*Pleural pain receptors*
- These receptors are primarily involved in sensing pain associated with **pleural inflammation** or injury, contributing to the sensation of pain with breathing.
- They do not play a role in regulating the primary ventilatory drive in response to blood gas changes.
*Central chemoreceptors*
- These receptors are located in the **medulla** and are primarily sensitive to changes in **arterial PCO2** and pH (via H+ ions in CSF).
- In chronic respiratory diseases with CO2 retention, they become **desensitized** to elevated CO2, shifting the main respiratory drive to the peripheral chemoreceptors' response to hypoxia.
*Airway stretch receptors*
- These receptors, including **slowly adapting stretch receptors** and **rapidly adapting irritant receptors**, are located in the airways and respond to lung inflation and irritants.
- They are involved in the Hering-Breuer reflex and cough reflex but are not the primary drivers of ventilation in response to hypoxemia.
*Pulmonary stretch receptors*
- These receptors are located in the **bronchial smooth muscle** and respond to lung distension, contributing to the **Hering-Breuer reflex** which inhibits inspiration to prevent overinflation.
- While important for lung mechanics, they do not directly sense blood gas levels to drive ventilation in the context of hypoxia or hypercapnia.
Dyspnea mechanisms US Medical PG Question 8: A 63-year-old man undergoes workup for nocturnal dyspnea and what he describes as a "choking" sensation while sleeping. He also endorses fatigue and dyspnea on exertion. Physical exam reveals a normal S1, loud P2, and a neck circumference of 17 inches (43 cm) (normal < 14 inches (< 35 cm)). His temperature is 98.8°F (37°C), blood pressure is 128/82 mmHg, pulse is 86/min, and respirations are 19/min. He undergoes spirometry, which is unrevealing, and polysomnography, which shows 16 hypopneic and apneic events per hour. Mean pulmonary arterial pressure is 30 mmHg. Which of the following complications is this patient most at risk for?
- A. Left ventricular failure
- B. Right ventricular failure (Correct Answer)
- C. Pulmonary embolism
- D. Aspiration pneumonia
- E. Chronic obstructive pulmonary disease
Dyspnea mechanisms Explanation: ***Right ventricular failure***
- The patient's symptoms (nocturnal dyspnea, choking sensation, fatigue, exertional dyspnea), risk factors (large neck circumference), and polysomnography results (16 hypopneic/apneic events/hour) are consistent with **obstructive sleep apnea (OSA)**.
- OSA leads to **chronic intermittent hypoxia** and hypercapnia, causing **pulmonary vasoconstriction** and increased pulmonary arterial pressure (mean PAP 30 mmHg), which can result in **pulmonary hypertension** and eventually **right ventricular failure**.
*Left ventricular failure*
- While OSA can exacerbate cardiovascular conditions, the primary cardiac complication directly resulting from ongoing pulmonary hypertension due to OSA is typically right-sided, not primarily left-sided, failure.
- There are no specific findings in the description (e.g., S3 gallop, crackles) that strongly point to left ventricular dysfunction as the most immediate and direct complication.
*Pulmonary embolism*
- Although obesity (suggested by large neck circumference) is a risk factor for pulmonary embolism, there are no acute symptoms (e.g., sudden onset dyspnea, pleuritic chest pain, hemoptysis) or signs (e.g., tachycardia, hypoxemia) to suggest a pulmonary embolism.
- The patient's symptoms are chronic and related to sleep-disordered breathing and pulmonary hypertension.
*Aspiration pneumonia*
- While a "choking" sensation could potentially lead to aspiration, there's no evidence of infection (e.g., fever, productive cough, crackles) or recurrent aspiration events.
- The primary respiratory pathology is clearly defined by the polysomnography and elevated pulmonary pressures.
*Chronic obstructive pulmonary disease*
- Spirometry was reported as "unrevealing," which rules out significant airflow limitation characteristic of COPD.
- The patient's symptoms are more indicative of sleep-disordered breathing and its cardiovascular consequences rather than an intrinsic obstructive lung disease like COPD.
Dyspnea mechanisms US Medical PG Question 9: A 22-year-old woman presents to the emergency department with a chief concern of shortness of breath. She was hiking when she suddenly felt unable to breathe and had to take slow deep breaths to improve her symptoms. The patient is a Swedish foreign exchange student and does not speak any English. Her past medical history and current medications are unknown. Her temperature is 99.5°F (37.5°C), blood pressure is 127/68 mmHg, pulse is 120/min, respirations are 22/min, and oxygen saturation is 90% on room air. Physical exam is notable for poor air movement bilaterally and tachycardia. The patient is started on treatment. Which of the following best describes this patient's underlying pathology?
FEV1 = Forced expiratory volume in 1 second
FVC = Forced vital capacity
DLCO = Diffusing capacity of carbon monoxide
- A. Increased FVC
- B. Increased FEV1
- C. Increased FEV1/FVC
- D. Decreased airway tone
- E. Normal DLCO (Correct Answer)
Dyspnea mechanisms Explanation: ***Normal DLCO***
- This patient presents with an acute exacerbation of what is likely **asthma**, showing symptoms of **shortness of breath**, **tachycardia**, poor air movement bilaterally, and improvement with slow deep breaths. **Asthma** characteristically affects the airways and not the alveoli, thus the **diffusing capacity of carbon monoxide (DLCO)**, which measures gas exchange across the alveolar-capillary membrane, would be expected to be normal.
- In asthma, the primary problem is **bronchoconstriction** and **airway inflammation**, which restricts airflow but does not typically impair the diffusion of gases like carbon monoxide across the alveolar-capillary membrane.
*Increased FVC*
- **Forced vital capacity (FVC)** is often normal or even slightly reduced in asthma due to **air trapping** and early airway closure, not increased.
- An increased FVC is usually not associated with obstructive lung diseases like asthma but could potentially be seen in conditions where lung volumes are pathologically large, which is not the case here.
*Increased FEV1*
- **Forced expiratory volume in 1 second (FEV1)** is typically **decreased** in obstructive lung diseases like asthma due to **airflow limitation**.
- An increased FEV1 would indicate better-than-average expiratory flow, which contradicts the symptoms of shortness of breath and poor air movement in this patient.
*Increased FEV1/FVC*
- The **FEV1/FVC ratio** is characteristically **decreased** in obstructive lung diseases like asthma, indicating that a disproportionately smaller amount of air can be exhaled in the first second relative to the total forced vital capacity.
- An increased FEV1/FVC ratio would be a sign of a restrictive lung disease or normal lung function, not an exacerbation of an obstructive process.
*Decreased airway tone*
- The underlying pathology in asthma is typically **bronchoconstriction**, which means an **increased airway tone** and narrowing of the airways, rather than decreased.
- Decreased airway tone would imply bronchodilation, which would alleviate, not cause, the patient's symptoms of shortness of breath and poor air movement.
Dyspnea mechanisms US Medical PG Question 10: A 21-year-old man is admitted to the intensive care unit for respiratory failure requiring mechanical ventilation. His minute ventilation is calculated to be 7.0 L/min, and his alveolar ventilation is calculated to be 5.1 L/min. Which of the following is most likely to decrease the difference between minute ventilation and alveolar ventilation?
- A. Increasing the partial pressure of inhaled oxygen
- B. Decreasing the affinity of hemoglobin for oxygen
- C. Increasing the respiratory depth
- D. Decreasing the physiologic dead space (Correct Answer)
- E. Increasing the respiratory rate
Dyspnea mechanisms Explanation: ***Decreasing the physiologic dead space***
- The difference between **minute ventilation (VE)** and **alveolar ventilation (VA)** is the **dead space ventilation (VD)**, calculated as: VE - VA = VD
- In this case: 7.0 L/min - 5.1 L/min = 1.9 L/min of dead space ventilation
- Decreasing the **physiologic dead space** directly reduces this difference by allowing a greater proportion of each breath to participate in gas exchange
- This is the most direct way to narrow the gap between VE and VA
*Increasing the partial pressure of inhaled oxygen*
- This intervention primarily affects **oxygenation** by increasing the driving pressure for oxygen diffusion into the blood
- It does not directly change the volume of air participating in alveolar ventilation or reduce dead space ventilation
- The distribution of ventilation between alveolar and dead space remains unchanged
*Decreasing the affinity of hemoglobin for oxygen*
- A decrease in hemoglobin affinity for oxygen facilitates **oxygen unloading** to the tissues (rightward shift of the oxygen-hemoglobin dissociation curve)
- This effect is related to **oxygen delivery** and does not alter the proportion of minute ventilation that reaches the alveoli for gas exchange
- Dead space ventilation remains unchanged
*Increasing the respiratory depth*
- Increasing respiratory depth increases **tidal volume (VT)**, which improves the **ratio** of alveolar ventilation to minute ventilation (VA/VE efficiency)
- However, the **absolute difference** (VE - VA) in L/min depends on the **total dead space volume**, which is not changed by increasing tidal volume alone
- While this improves ventilation efficiency, it does not directly reduce the dead space ventilation measured in L/min unless physiologic dead space itself decreases
*Increasing the respiratory rate*
- While increasing respiratory rate increases **minute ventilation (VE)**, it also increases the frequency of ventilating the **dead space** with each breath
- Since dead space ventilation (VD) = respiratory rate × dead space volume, increasing rate while keeping tidal volume constant will proportionally increase both VE and VD
- This can actually widen the absolute gap between VE and VA, making it less efficient
More Dyspnea mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.