Central and peripheral chemoreceptors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Central and peripheral chemoreceptors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Central and peripheral chemoreceptors US Medical PG Question 1: A 39-year-old woman is brought to the emergency room by her husband because of severe dyspnea and dizziness. Her symptoms started suddenly 30 minutes ago. She appears distressed. Arterial blood gas shows a pH of 7.51, pO2 of 100 mm Hg, and a pCO2 of 30 mm Hg. Which of the following is the most likely cause?
- A. Myasthenia gravis
- B. Opioid toxicity
- C. Panic attack (Correct Answer)
- D. Epiglottitis
- E. Pulmonary fibrosis
Central and peripheral chemoreceptors Explanation: ***Panic attack***
- The sudden onset of **severe dyspnea** and **dizziness** in a distressed patient, along with ABG results indicating **respiratory alkalosis** (pH 7.51, pCO2 30 mm Hg), is highly characteristic of a panic attack with hyperventilation.
- **Hyperventilation** leads to excessive CO2 exhalation, causing the pCO2 to drop and the pH to rise, resulting in symptoms like lightheadedness and dyspnea.
*Myasthenia gravis*
- This is a **neuromuscular disorder** causing muscle weakness, which can lead to respiratory compromise over time, but typically does not present with such acute, sudden dyspnea and dizziness without prior symptoms.
- The ABG findings of respiratory alkalosis are not typical for a primary myasthenic crisis, which would likely show respiratory acidosis if respiratory failure were imminent.
*Opioid toxicity*
- Opioid overdose causes **respiratory depression**, leading to reduced respiratory rate and shallow breathing, which would result in **respiratory acidosis** (increased pCO2 and decreased pH), not alkalosis.
- The patient's pO2 of 100 mm Hg also argues against significant respiratory depression.
*Epiglottitis*
- Epiglottitis presents with a **rapidly worsening sore throat**, difficulty swallowing, drooling, and stridor, indicating upper airway obstruction.
- While it causes severe dyspnea, the ABG would likely show signs of hypoxemia and potentially acidosis due to airway compromise, not hyperventilation-induced alkalosis.
*Pulmonary fibrosis*
- This is a **chronic interstitial lung disease** that causes progressive dyspnea, often with a dry cough.
- The onset of symptoms is typically gradual, over months to years, not sudden within 30 minutes, and ABG would likely show hypoxemia with compensated respiratory alkalosis or acidosis depending on the stage, but not acutely severe hyperventilation-induced alkalosis.
Central and peripheral chemoreceptors US Medical PG Question 2: A 24-year-old woman presents to the emergency department after she was found agitated and screaming for help in the middle of the street. She says she also has dizziness and tingling in the lips and hands. Her past medical history is relevant for general anxiety disorder, managed medically with paroxetine. At admission, her pulse is 125/min, respiratory rate is 25/min, and body temperature is 36.5°C (97.7°F). Physical examination is unremarkable. An arterial blood gas sample is taken. Which of the following results would you most likely expect to see in this patient?
- A. pH: increased, HCO3-: increased, Pco2: increased
- B. pH: decreased, HCO3-: decreased, Pco2: decreased
- C. pH: decreased, HCO3-: increased, Pco2: increased
- D. pH: increased, HCO3-: decreased, Pco2: decreased (Correct Answer)
- E. pH: normal, HCO3-: increased, Pco2: increased
Central and peripheral chemoreceptors Explanation: ***pH: increased, HCO3-: decreased, Pco2: decreased***
- The patient's presentation with **agitation**, **dizziness**, **paresthesias** (tingling in lips and hands), and **tachypnea** (respiratory rate 25/min) is highly suggestive of **hyperventilation** due to an anxiety attack.
- **Hyperventilation** leads to excessive **CO2 expulsion**, causing a decrease in Pco2, which results in respiratory alkalosis (increased pH) and a compensatory decrease in HCO3-.
*pH: increased, HCO3-: increased, Pco2: increased*
- An **increased pH** coupled with **increased HCO3-** and **increased Pco2** would suggest a **metabolic alkalosis with respiratory compensation**, which is not consistent with the patient's acute hyperventilation.
- While pH is increased, the other values contradict the primary respiratory cause suggested by the symptoms.
*pH: decreased, HCO3-: decreased, Pco2: decreased*
- This profile describes **metabolic acidosis with respiratory compensation**, which would typically present with **Kussmaul breathing** and other signs of acidosis, not acute hyperventilation and agitation.
- Symptoms such as dizziness and tingling are associated with alkalosis, not acidosis.
*pH: decreased, HCO3-: increased, Pco2: increased*
- This pattern is characteristic of **respiratory acidosis with metabolic compensation**, often seen in conditions like **COPD exacerbation** or **opioid overdose** with hypoventilation.
- The patient's rapid breathing and clinical picture are not consistent with respiratory acidosis.
*pH: normal, HCO3-: increased, Pco2: increased*
- A **normal pH** with **increased HCO3-** and **increased Pco2** would indicate a **compensated metabolic alkalosis**.
- Her acute symptoms point to an uncompensated or acutely compensated respiratory disorder, not a compensated metabolic issue.
Central and peripheral chemoreceptors US Medical PG Question 3: A histological examination of the carotid body reveals glomus cells containing dense-core vesicles. These cells function primarily as chemoreceptors for which of the following?
- A. Partial pressure of oxygen (Correct Answer)
- B. Blood pH
- C. Temperature
- D. Blood glucose levels
Central and peripheral chemoreceptors Explanation: ***Partial pressure of oxygen***
- Carotid body **glomus cells** are highly specialized **chemoreceptors** that primarily sense changes in the **partial pressure of oxygen (PO2)** in arterial blood.
- When PO2 decreases (e.g., hypoxia), these cells are activated and stimulate the respiratory and cardiovascular systems to increase oxygen uptake.
*Blood pH*
- While carotid body chemoreceptors can sense large changes in blood pH, their primary and most sensitive role is in detecting changes in **PO2**.
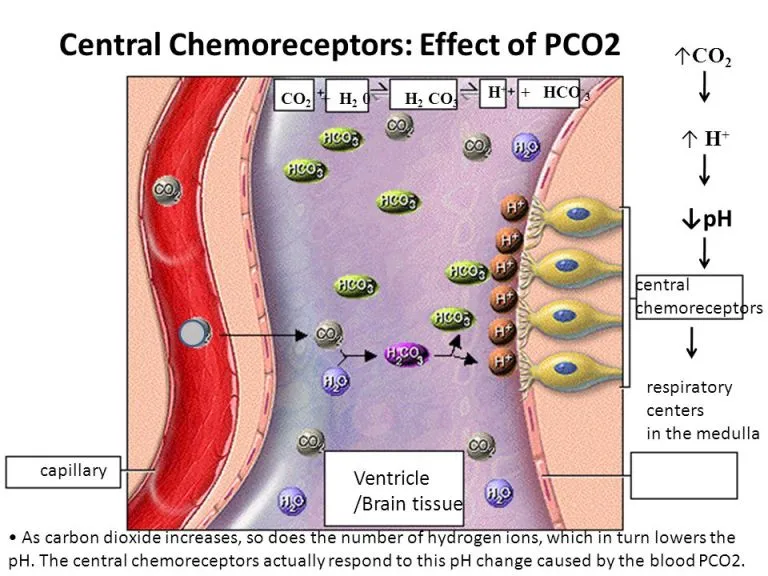
- Central chemoreceptors in the brainstem are more crucial for routine regulation of respiration in response to changes in **pH and PCO2**.
*Temperature*
- **Thermoreceptors** located in the skin, hypothalamus, and other internal organs are responsible for sensing body temperature, not the carotid body.
- The carotid body's main function is related to blood gas homeostasis, not temperature regulation.
*Blood glucose levels*
- Blood glucose levels are regulated by specialized cells in the **pancreas** (islets of Langerhans) that secrete hormones like insulin and glucagon.
- The carotid body is not directly involved in sensing or regulating glucose homeostasis.
Central and peripheral chemoreceptors US Medical PG Question 4: Two hours after undergoing elective cholecystectomy with general anesthesia, a 41-year-old woman is evaluated for decreased mental status. BMI is 36.6 kg/m2. Respirations are 18/min and blood pressure is 126/73 mm Hg. Physical examination shows the endotracheal tube in normal position. She does not respond to sternal rub and gag reflex is absent. Arterial blood gas analysis on room air shows normal PO2 and PCO2 levels. Which of the following anesthetic properties is the most likely cause of these findings?
- A. Low blood solubility
- B. High lipid solubility (Correct Answer)
- C. Low brain-blood partition coefficient
- D. High minimal alveolar concentration
- E. Low cytochrome P450 activity
Central and peripheral chemoreceptors Explanation: ***High lipid solubility***
- Anesthetics with **high lipid solubility** accumulate in **adipose tissue** and are slowly released, prolonging their effect, especially in obese patients.
- The patient's **obesity (BMI 36.6 kg/m2)** contributes to a larger reservoir for lipid-soluble drugs, leading to delayed recovery and decreased mental status.
*Low blood solubility*
- **Low blood solubility** implies a rapid equilibrium between the lungs and the blood, leading to a **faster onset and offset** of anesthetic action.
- This property would result in a quicker recovery from anesthesia, which contradicts the patient's prolonged unconsciousness.
*Low brain-blood partition coefficient*
- A **low brain-blood partition coefficient** means the anesthetic does not accumulate significantly in brain tissue relative to blood.
- Agents with this property equilibrate quickly and leave the brain rapidly upon discontinuation, resulting in **fast recovery**, which is inconsistent with the patient's persistent decreased mental status.
*High minimal alveolar concentration*
- **High minimal alveolar concentration (MAC)** means that a higher concentration of the anesthetic gas is required to produce immobility in 50% of patients.
- A high MAC describes the **potency** of an anesthetic and does not directly explain prolonged recovery or decreased mental status in an obese patient, but rather indicates that a larger dose or concentration was needed to achieve anesthesia.
*Low cytochrome P450 activity*
- **Low cytochrome P450 activity** would lead to slower metabolism of drugs that are primarily cleared by this system, potentially prolonging their effects.
- While relevant for some drugs, the primary issue for inhaled anesthetics is their **physical distribution and elimination**, not typically metabolic clearance via Cytochrome P450 enzymes.
Central and peripheral chemoreceptors US Medical PG Question 5: A 45-year-old woman presents to the physician with a 6-month history of progressive shortness of breath. She now has to stop to rest three or four times whenever she climbs the stairs to her apartment on the third floor. She reports chronic, nonproductive cough and wheezing, for which she uses ipratropium inhalers. She has a 25 pack-year smoking history. On examination, the blood pressure is 130/80 mm Hg, the pulse rate is 95/min, the temperature is 36.6°C (97.8°F), and the respiratory rate is 26/min. Chest auscultation reveals bilateral crepitations. Cardiac auscultation reveals normal S1 and S2 without murmurs or added sounds. Arterial blood gas analysis shows:
pH 7.36 (reference: 7.35–7.45)
HCO3- 32 mEq/L (reference 22–28 mEq/L)
Pco2 48 mm Hg (reference: 33–45 mm Hg)
Po2 63 mm Hg (reference: 75–105 mm Hg)
O2 saturation 91% (reference: 94–99%)
Which of the following would you expect to find in this patient?
- A. Shift of the flow volume loop to the right
- B. Decreased lung compliance
- C. Decreased diffusing capacity of the lungs for carbon monoxide (DLCO) (Correct Answer)
- D. Decreased lung residual volume
- E. Increased FEV1/FVC ratio
Central and peripheral chemoreceptors Explanation: ***Decreased diffusing capacity of the lungs for carbon monoxide (DLCO)***
- This patient's presentation with **progressive dyspnea**, **chronic cough**, **wheezing**, **25 pack-year smoking history**, and **chronic respiratory acidosis with metabolic compensation** (elevated PCO2 48, elevated HCO3- 32) is highly suggestive of **COPD with emphysema component**.
- The **ABG pattern shows chronic CO2 retention** with renal compensation (elevated bicarbonate), which is characteristic of **chronic obstructive lung disease**, not restrictive disease.
- In **emphysema**, there is **destruction of alveolar walls** and loss of elastic recoil, leading to **impaired gas exchange** and **decreased DLCO** due to reduced surface area for gas diffusion.
- Decreased DLCO is a hallmark finding in emphysema and helps differentiate it from chronic bronchitis (where DLCO may be normal).
*Incorrect: Shift of the flow volume loop to the right*
- While this patient likely has **obstructive lung disease (COPD)**, a shift of the flow-volume loop to the **right** indicates **increased lung volumes and hyperinflation**, not the loop shape itself.
- In COPD, the flow-volume loop shows **decreased flow rates** (scooped appearance) rather than a simple rightward shift, making this description imprecise.
*Incorrect: Decreased lung compliance*
- **Decreased lung compliance** is characteristic of **restrictive lung diseases** (e.g., pulmonary fibrosis, ARDS) where lungs become stiff.
- In **emphysema/COPD**, lung compliance is typically **increased** (lungs become more compliant/floppy) due to loss of elastic tissue, not decreased.
- This patient's ABG pattern of chronic hypercapnia indicates obstructive disease, not restrictive disease.
*Incorrect: Decreased lung residual volume*
- This is the **opposite** of what would be expected in COPD/emphysema.
- In **obstructive lung disease**, residual volume is **increased** due to **air trapping** and inability to fully exhale.
- **Decreased residual volume** would be seen in **restrictive lung diseases**, which does not fit this patient's chronic hypercapnic respiratory acidosis.
*Incorrect: Increased FEV1/FVC ratio*
- This is the **opposite** of what would be expected in COPD.
- In **obstructive lung disease**, the FEV1/FVC ratio is **decreased** (typically <0.70) because airflow limitation reduces FEV1 more than FVC.
- An **increased FEV1/FVC ratio** is seen in **restrictive lung diseases**, where both volumes decrease but FVC decreases proportionally more than FEV1.
Central and peripheral chemoreceptors US Medical PG Question 6: A man returns home late at night to find his 15-year-old son and 40-year-old wife unconscious in the family room. He immediately summons emergency services. In the field, pulse oximetry shows oxygen saturation at 100% for both patients. 100%, yet they both appear cyanotic. Both patients are provided with 2L of oxygen by way of nasal cannula on the way to the hospital. An arterial blood gas is performed on the teenager and reveals pH of 7.35, PaCO2 of 31.8 mm Hg, PaO2 of 150 mm Hg, HCO3- of 20 mEq/L, SaO2 of 80%, and a COHb of 18%. What is the most likely cause of his condition?
- A. Ischemic hypoxia
- B. Methemoglobinemia
- C. Diffusion-limited hypoxia
- D. Carbon monoxide poisoning (Correct Answer)
- E. Anemic hypoxia
Central and peripheral chemoreceptors Explanation: ***Carbon monoxide poisoning***
- The combination of **cyanosis**, **normal pulse oximetry readings (due to inaccurate readings for CO)**, and a **high COHb level (18%)** is highly indicative of carbon monoxide poisoning.
- Exposure to carbon monoxide forms **carboxyhemoglobin (COHb)**, which has a higher affinity for hemoglobin than oxygen, leading to **tissue hypoxia** despite normal PaO2.
*Ischemic hypoxia*
- This type of hypoxia occurs when there is **reduced blood flow** to a tissue, often due to conditions like **heart failure, shock**, or **arterial occlusion**.
- There is no clinical or lab evidence in the scenario to suggest reduced blood flow as the primary cause of the patient's symptoms.
*Methemoglobinemia*
- While methemoglobinemia can also cause **cyanosis** and an **oxygen saturation gap** (discrepancy between SaO2 and pulse oximetry), it is characterized by a high level of **methemoglobin (MetHb)**.
- The patient's COHb level is elevated at 18%, but there's no information suggesting elevated MetHb, distinguishing it from carbon monoxide poisoning.
*Diffusion-limited hypoxia*
- This occurs when the **diffusion of oxygen from the alveoli to the blood is impaired**, as seen in conditions like **pulmonary fibrosis** or **severe emphysema**.
- The patient's PaO2 of 150 mmHg is very high, indicating excellent oxygen loading in the lungs, which rules out a diffusion limitation.
*Anemic hypoxia*
- Anemic hypoxia results from a **decreased oxygen-carrying capacity of the blood** due to a **low hemoglobin concentration**.
- The scenario does not provide information about the patient's hemoglobin level, and the primary issue is the inability of hemoglobin to release oxygen due to CO binding, not a lack of hemoglobin itself.
Central and peripheral chemoreceptors US Medical PG Question 7: A 17-year-old girl comes to the emergency department because of numbness around her mouth and uncontrolled twitching of the mouth for the past 30 minutes. Her symptoms began while she was at a concert. Her temperature is 37°C (98.6°F), pulse is 69/min, and respirations are 28/min. When the blood pressure cuff is inflated, painful contractions of the hand muscles occur. Arterial blood gas shows a pH of 7.53, pO2 of 100 mm Hg, and a pCO2 of 29 mm Hg. Which of the following additional findings is most likely in this patient?
- A. Increased serum potassium concentration
- B. Increased serum phosphate concentration
- C. Decreased serum ionized calcium concentration (Correct Answer)
- D. Increased peripheral oxygen unloading from hemoglobin
- E. Decreased cerebral blood flow
Central and peripheral chemoreceptors Explanation: ***Decreased serum ionized calcium concentration***
- The patient presents with **circumoral numbness** and **muscle twitching** (consistent with tetany), and a positive **Trousseau's sign** (painful contractions of hand muscles with blood pressure cuff inflation). These are classic signs of **hypocalcemia**.
- The **arterial blood gas** shows **respiratory alkalosis** (elevated pH 7.53, decreased pCO2 29 mm Hg). In alkalosis, more calcium binds to albumin, causing a **decrease in ionized (free) calcium** even when total calcium is normal. It is the ionized calcium that is physiologically active and responsible for neuromuscular function.
- The **decreased ionized calcium** directly causes the tetany and neuromuscular irritability observed in this patient.
*Increased serum potassium concentration*
- **Hyperkalemia** typically presents with muscle weakness, fatigue, and cardiac arrhythmias, not tetany or circumoral numbness.
- The symptoms described are not characteristic of high potassium levels.
*Increased serum phosphate concentration*
- **Hyperphosphatemia** can lead to decreased serum calcium due to the formation of calcium-phosphate complexes, but it is not the primary direct cause of the symptoms in the setting of acute respiratory alkalosis.
- Furthermore, hyperphosphatemia itself does not directly cause muscle twitching or circumoral numbness as a primary effect.
*Increased peripheral oxygen unloading from hemoglobin*
- **Increased oxygen unloading** from hemoglobin (a right shift of the oxygen dissociation curve) is typically associated with acidosis, fever, or increased 2,3-BPG.
- **Alkalosis** (as seen in this patient) causes a **left shift** of the oxygen dissociation curve, leading to **decreased oxygen unloading** in the periphery.
*Decreased cerebral blood flow*
- **Hyperventilation** causes **respiratory alkalosis**, which in turn leads to **cerebral vasoconstriction** and therefore **decreased cerebral blood flow**.
- While this is a true physiological consequence of the patient's hyperventilation, it does not directly explain the **tetany** and **circumoral numbness** (which are due to decreased ionized calcium). The neuromuscular symptoms are specifically caused by hypocalcemia, making ionized calcium the most relevant additional finding.
Central and peripheral chemoreceptors US Medical PG Question 8: A 24-year-old male is brought in by ambulance to the emergency department after he was found unresponsive at home for an unknown length of time. Upon arrival, he is found to be severely altered and unable to answer questions about his medical history. Based on clinical suspicion, a panel of basic blood tests are obtained including an arterial blood gas, which shows a pH of 7.32, a pCO2 of 70, and a bicarbonate level of 30 mEq/L. Which of the following is most likely the primary disturbance leading to the values found in the ABG?
- A. Respiratory acidosis (Correct Answer)
- B. Metabolic alkalosis
- C. Respiratory alkalosis
- D. Metabolic acidosis
- E. Mixed alkalosis
Central and peripheral chemoreceptors Explanation: ***Respiratory acidosis***
- The **pH (7.32)** is acidic (normal 7.35-7.45), and the **pCO2 (70 mmHg)** is significantly elevated (normal 35-45 mmHg), indicating **primary respiratory acidosis** due to hypoventilation.
- The **bicarbonate (30 mEq/L)** is elevated above normal (22-26 mEq/L), indicating **partial metabolic compensation** by the kidneys retaining bicarbonate to buffer the acidosis.
- This pattern suggests **chronic respiratory acidosis** (e.g., from COPD, CNS depression, neuromuscular disease) with renal compensation.
*Metabolic alkalosis*
- This would present with **elevated pH** (>7.45) and **elevated bicarbonate** as the primary disturbance, often with compensatory elevation in pCO2.
- The patient's **pH is acidic (7.32)**, not alkalotic, ruling out metabolic alkalosis as the primary process.
*Respiratory alkalosis*
- This would present with **elevated pH** (>7.45) and **decreased pCO2** (<35 mmHg) due to hyperventilation.
- The patient has the opposite: **acidic pH and elevated pCO2**, ruling out respiratory alkalosis.
*Metabolic acidosis*
- This would present with **decreased pH** and **decreased bicarbonate** (<22 mEq/L) as the primary disturbance.
- While the pH is low, the **bicarbonate is elevated (30 mEq/L)**, not decreased, ruling out metabolic acidosis as the primary disorder.
*Mixed alkalosis*
- A mixed alkalosis would involve simultaneous respiratory and metabolic processes causing **elevated pH**.
- The patient's **pH is acidic (7.32)**, making any form of alkalosis impossible as the primary disturbance.
Central and peripheral chemoreceptors US Medical PG Question 9: A 28-year-old female comes to the emergency department complaining of heart palpitations. She has had multiple episodes of these in the past few months. She has found that if she wears tight clothing then sometimes these episodes will stop spontaneously. On presentation to the ED, she feels like her heart is pounding and reports feeling nauseous. She appears mildly diaphoretic. Her blood pressure is 125/75 mmHg, pulse is 180/min, and respirations are 22/min with an O2 saturation of 99% on room air. A neck maneuver is performed and her pulse returns to 90/min with improvement of her symptoms. Stimulation of afferent fibers from which nerve are most responsible for the resolution of her symptoms?
- A. Facial
- B. Hypoglossal
- C. Glossopharyngeal (Correct Answer)
- D. Trigeminal
- E. Vagus
Central and peripheral chemoreceptors Explanation: ***Glossopharyngeal***
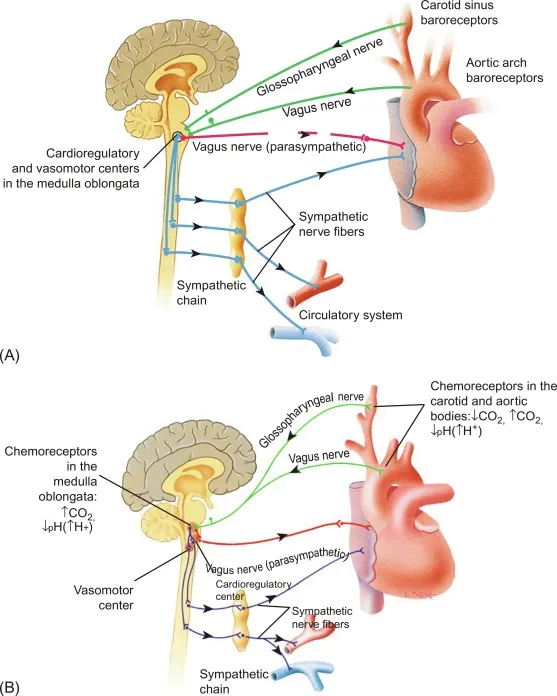
- The question specifically asks about **afferent fibers** responsible for the resolution of symptoms during the neck maneuver (carotid sinus massage).
- The **glossopharyngeal nerve (cranial nerve IX)** provides the **afferent (sensory) limb** of the baroreflex by carrying signals from **baroreceptors in the carotid sinus** to the nucleus tractus solitarius in the medulla.
- When the carotid sinus is massaged, baroreceptors are stimulated → afferent signals travel via **CN IX** → medullary cardiovascular centers → efferent vagal output → heart rate slows.
- This is the afferent pathway that initiates the reflex response to terminate **supraventricular tachycardia (SVT)**.
*Vagus*
- The **vagus nerve (cranial nerve X)** is crucial for treating SVT, but it provides the **efferent (motor) limb** of the baroreflex, not the afferent limb.
- After afferent signals from CN IX reach the medulla, the vagus nerve carries parasympathetic output to the SA node to slow the heart rate.
- If the question asked about efferent fibers, vagus would be correct, but it asks specifically about **afferent fibers**.
*Facial*
- The **facial nerve (cranial nerve VII)** primarily controls **facial expressions**, carries taste sensation from the anterior two-thirds of the tongue, and innervates salivary glands.
- It has no role in the baroreflex or cardiac rhythm regulation via neck maneuvers.
*Hypoglossal*
- The **hypoglossal nerve (cranial nerve XII)** is responsible for **tongue movement**.
- It has no involvement in cardiac rhythm regulation or the afferent pathways of the baroreflex.
*Trigeminal*
- The **trigeminal nerve (cranial nerve V)** mediates sensation from the face and controls the muscles of **mastication (chewing)**.
- While trigeminal stimulation via the **diving reflex** (cold water on face) can cause bradycardia, this is not the mechanism involved in carotid sinus massage for SVT treatment.
Central and peripheral chemoreceptors US Medical PG Question 10: A researcher is studying proteins that contribute to intestinal epithelial permeability. He has isolated intestinal tissue from several mice. After processing the tissue into its individual components, he uses a Western blot analysis to identify a protein that forms part of a multi-protein complex at the apical aspect of epithelial cells. The complex is known to provide a diffusion barrier between the apical and basolateral aspects of epithelial cells. Which of the following proteins is this researcher most likely investigating?
- A. Integrin
- B. Connexon
- C. Desmoglein
- D. E-cadherin
- E. Claudin (Correct Answer)
Central and peripheral chemoreceptors Explanation: ***Claudin***
- **Claudins** are integral membrane proteins that are primary components of **tight junctions** (zonulae occludentes), which form a diffusion barrier at the **apical aspect** of epithelial cells.
- They regulate **paracellular permeability**, crucial for maintaining the integrity of the intestinal epithelial barrier.
*Integrin*
- **Integrins** are transmembrane receptors that mediate cell-extracellular matrix (ECM) adhesion and cell-cell adhesion, but they are not the primary components of tight junction diffusion barriers.
- They are involved in cell signaling and structural support, rather than forming a direct paracellular seal.
*Connexon*
- A **connexon** is a protein assembly that forms a **gap junction**, allowing direct communication and passage of small molecules between adjacent cells.
- Gap junctions facilitate intercellular communication, but do not primarily contribute to sealing the paracellular space as a diffusion barrier.
*Desmoglein*
- **Desmoglein** is a cadherin family protein found in **desmosomes** (maculae adherens), which are cell-cell adhesion complexes that provide strong mechanical attachments between cells.
- Desmosomes resist shearing forces and provide structural integrity but do not regulate paracellular permeability as tight junctions do.
*E-cadherin*
- **E-cadherin** is a crucial component of **adherens junctions** (zonula adherens), which provide cell-cell adhesion and help establish and maintain cell polarity.
- While important for epithelial integrity, E-cadherin primarily links cells to the actin cytoskeleton and is not directly responsible for forming the selective diffusion barrier itself.
More Central and peripheral chemoreceptors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.