Parturition physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Parturition physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Parturition physiology US Medical PG Question 1: A 26-year-old woman comes to the emergency department because of a 3-day history of nausea and vomiting. Her last menstrual period was 9 weeks ago. A urine pregnancy test is positive. Ultrasonography shows an intrauterine pregnancy consistent in size with a 7-week gestation. The hormone that was measured in this patient's urine to detect the pregnancy is also directly responsible for which of the following processes?
- A. Development of breast tissue
- B. Preparation of the uterine endometrium for implantation
- C. Inhibition of preterm uterine contractions
- D. Maintenance of the corpus luteum (Correct Answer)
- E. Inhibition of ovulation
Parturition physiology Explanation: ***Maintenance of the corpus luteum***
- The hormone measured in the urine pregnancy test is **human chorionic gonadotropin (hCG)**.
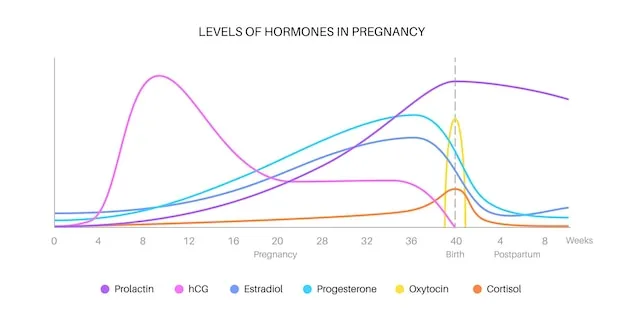
- **hCG** acts like **luteinizing hormone (LH)** to maintain the **corpus luteum** in early pregnancy, ensuring continued progesterone production until the placenta takes over.
*Development of breast tissue*
- **Estrogen** and **progesterone** are the primary hormones responsible for the development of breast tissue during pregnancy, preparing the breasts for lactation.
- While hCG indirectly supports these hormones, it does not directly cause breast tissue development.
*Preparation of the uterine endometrium for implantation*
- The **preparation of the uterine endometrium** for implantation is primarily driven by **progesterone**, produced by the corpus luteum initially and later by the placenta.
- hCG’s role is to maintain the corpus luteum, thus indirectly supporting progesterone production.
*Inhibition of preterm uterine contractions*
- **Progesterone** is the main hormone responsible for **inhibiting uterine contractions** during pregnancy to prevent preterm labor.
- While hCG supports progesterone production, it does not directly inhibit uterine contractions itself.
*Inhibition of ovulation*
- High levels of **estrogen** and **progesterone** during pregnancy suppress the hypothalamic-pituitary-gonadal axis, thereby **inhibiting ovulation**.
- While hCG maintains the corpus luteum which produces these hormones, hCG itself is not the direct inhibitor of ovulation.
Parturition physiology US Medical PG Question 2: A 19-year-old woman comes to the physician because of a delayed menstrual period. She has had regular menses since menarche at age 11. Her last menstrual period was 7 weeks ago. She is sexually active with two male partners. A urine pregnancy test is positive. An ultrasound of the pelvis shows a viable intrauterine pregnancy with an estimated gestational age of 6 weeks and 5 days. She does not wish to continue with the pregnancy. After carefully weighing the options with her physician, she is prescribed two medications, one of which is mifepristone. Which of the following is this drug's primary mechanism of action?
- A. Activation of prostaglandin E1 receptors
- B. Inhibition of dihydrofolate reductase
- C. Blockage of progesterone receptor (Correct Answer)
- D. Agonist at oxytocin receptors
- E. Antagonist at gonadotropin-releasing hormone receptors
Parturition physiology Explanation: ***Blockage of progesterone receptor***
- **Mifepristone** is a **progesterone receptor antagonist**, meaning it blocks the action of progesterone.
- Progesterone is essential for maintaining early pregnancy by supporting the **endometrium** and preventing uterine contractions.
*Activation of prostaglandin E1 receptors*
- This is the primary mechanism of action for **misoprostol**, the second medication often used in medical abortion protocols.
- **Misoprostol** causes **uterine contractions** and cervical ripening, which expels the uterine contents after mifepristone has prepared the uterus.
*Inhibition of dihydrofolate reductase*
- This is the mechanism of action for **methotrexate**, an antifolate drug that can also be used for medical abortion.
- **Methotrexate** inhibits DNA synthesis in rapidly dividing cells, leading to the termination of the pregnancy.
*Agonist at oxytocin receptors*
- **Oxytocin agonists** (like oxytocin itself) are typically used for labor induction or to control postpartum hemorrhage, not for early medical abortion.
- They cause strong uterine contractions but are usually administered later in pregnancy or postpartum.
*Antagonist at gonadotropin-releasing hormone receptors*
- **GnRH antagonists** (e.g., cetrorelix, ganirelix) are used in assisted reproductive technologies to prevent premature ovulation.
- They do not directly cause medical abortion by blocking progesterone's action or directly inducing uterine contractions.
Parturition physiology US Medical PG Question 3: A 39-year-old woman, gravida 5, para 4, at 41 weeks' gestation is brought to the hospital because of regular uterine contractions that started 2 hours ago. Pregnancy has been complicated by iron deficiency anemia treated with iron supplements. Pelvic examination shows the cervix is 90% effaced and 7-cm dilated; the vertex is at -1 station. Fetal heart tracing is shown. The patient is repositioned, O2 therapy is initiated, and amnioinfusion is done. A repeat assessment after 20 minutes shows a similar cervical status, and no changes in the fetal heart tracing, and less than 5 contractions in a period of 10 minutes.What is the most appropriate next step in management?
- A. Emergent cesarean delivery (Correct Answer)
- B. Monitor without intervention
- C. Begin active pushing
- D. Retry maternal repositioning
- E. Administer tocolytics
Parturition physiology Explanation: ***Emergent cesarean delivery***
- The fetal heart tracing shows **recurrent late decelerations** unresponsive to **intrauterine resuscitation** (repositioning, O2, amnioinfusion), indicating fetal distress and uteroplacental insufficiency.
- Given the fetal distress and persistent late decelerations despite interventions, **expedited delivery** via cesarean section is indicated to prevent further fetal compromise.
*Monitor without intervention*
- This approach is inappropriate as the fetal heart tracing indicates **fetal distress** with recurrent **late decelerations** that have not resolved with initial interventions.
- Continued monitoring without action would place the fetus at risk for **hypoxia** and acidosis.
*Begin active pushing*
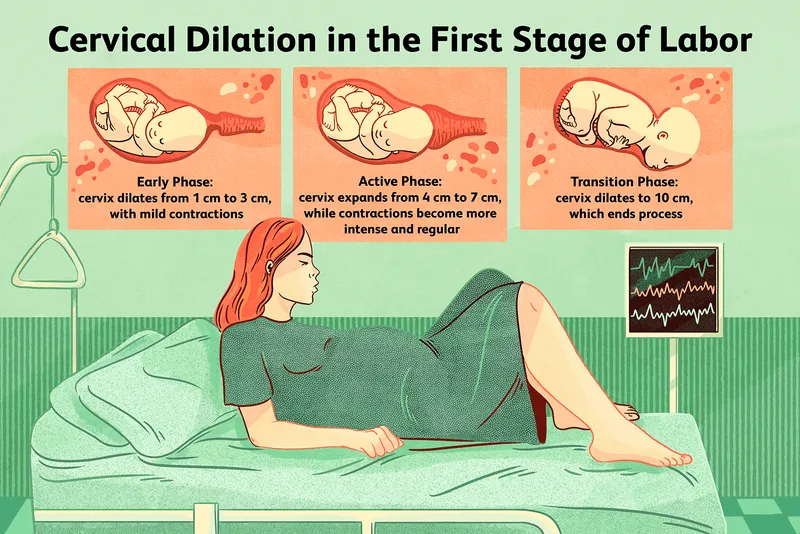
- The cervix is 7-cm dilated, meaning the patient is still in the **active phase of labor** and has not reached **complete cervical dilation** (10 cm) necessary for effective pushing.
- Pushing at this stage is unlikely to resolve the fetal distress and can potentially worsen **fetal acidosis** and maternal exhaustion.
*Retry maternal repositioning*
- The patient has already been repositioned and received other intrauterine resuscitation measures (O2 therapy, amnioinfusion) without improvement in the fetal heart tracing.
- Repeated repositioning alone is unlikely to resolve the underlying cause of the **late decelerations** in this context.
*Administer tocolytics*
- Tocolytics are used to **reduce uterine contractions** and manage conditions like **uterine tachysystole** or arrested labor, which are not explicitly present as the primary problem here (less than 5 contractions in 10 minutes).
- While they can temporarily improve uterine blood flow, they do not address the persistent **fetal distress** indicated by the recurrent late decelerations unresponsive to other interventions.
Parturition physiology US Medical PG Question 4: A 32-year-old female presents to her obstetrician 3 weeks postpartum for failure to lactate. Of note, she has been unable to tolerate cold environments since the birth of her child. Review of systems is positive for fatigue, lightheadedness, and a 3-pound weight gain over the last 3 weeks. Her delivery was complicated by placenta accreta with postpartum blood loss. Her newborn infant is doing well on formula. She denies any personal or family history of thyroid disease. Physical exam is overall unremarkable. On a panel of hormone testing, which of the following levels is most likely to be normal in this patient?
- A. Thyroid hormone
- B. Cortisol
- C. Luteinizing hormone
- D. Antidiuretic hormone (Correct Answer)
- E. Aldosterone
Parturition physiology Explanation: ***Antidiuretic hormone***
- This patient is presenting with symptoms consistent with **Sheehan syndrome**, which is postpartum pituitary necrosis due to severe hemorrhage and hypovolemic shock.
- Sheehan syndrome **primarily affects the anterior pituitary**, where most pituitary hormones are produced.
- **Antidiuretic hormone (ADH)** is synthesized by the **hypothalamus** and stored/released by the **posterior pituitary**, which is typically **spared** in Sheehan syndrome due to its separate blood supply.
- Therefore, **ADH levels would be normal** in this patient, making this the correct answer.
*Aldosterone*
- The **renin-angiotensin-aldosterone system (RAAS)** is regulated independently by the kidneys and is preserved in pituitary disorders.
- Aldosterone levels would also likely be **normal** in this patient.
- However, ADH is the better answer as it specifically demonstrates the anatomical distinction between anterior and posterior pituitary function.
*Thyroid hormone*
- The **anterior pituitary** fails to produce **thyroid-stimulating hormone (TSH)** in Sheehan syndrome, leading to secondary hypothyroidism.
- This results in **low thyroid hormone levels**.
- Her symptoms of **cold intolerance**, **fatigue**, and **weight gain** are classic manifestations of hypothyroidism.
*Cortisol*
- The anterior pituitary produces **adrenocorticotropic hormone (ACTH)**, which stimulates cortisol release from the adrenal glands.
- In Sheehan syndrome, failure of ACTH production leads to **secondary adrenal insufficiency** with **low cortisol levels**.
- This contributes to her **fatigue** and **lightheadedness**.
*Luteinizing hormone*
- The anterior pituitary produces **luteinizing hormone (LH)**, which is crucial for ovarian function and ovulation.
- The patient's **failure to lactate** is due to **prolactin deficiency** (another anterior pituitary hormone), not LH deficiency.
- Lack of LH and other gonadotropins would contribute to amenorrhea and loss of reproductive function that often accompany Sheehan syndrome.
Parturition physiology US Medical PG Question 5: A 23-year-old woman comes to the emergency department because of a 5-day history of nausea and vomiting. There is no associated fever, abdominal pain, constipation, diarrhea, or dysuria. She is sexually active and uses condoms inconsistently. Her last menstrual period was 10 weeks ago. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 18/min, and blood pressure is 110/70 mm Hg. There is no rebound tenderness or guarding. A urine pregnancy test is positive. Ultrasonography shows an intrauterine pregnancy consistent in size with an 8-week gestation. The hormone that was measured in this patient's urine to detect the pregnancy is also directly responsible for which of the following processes?
- A. Hypertrophy of the uterine myometrium
- B. Fetal angiogenesis
- C. Maintenance of the corpus luteum (Correct Answer)
- D. Inhibition of ovulation
- E. Stimulation of uterine contractions at term
Parturition physiology Explanation: ***Maintenance of the corpus luteum***
- The hormone measured in the urine pregnancy test is **human chorionic gonadotropin (hCG)**. hCG's primary role early in pregnancy is to **maintain the corpus luteum**, which in turn produces progesterone to support the uterine lining.
- The **corpus luteum** is essential for progesterone production until the placenta is sufficiently developed to take over this function, typically around 8-10 weeks gestation.
*Hypertrophy of the uterine myometrium*
- **Estrogen** and **progesterone** are primarily responsible for the hypertrophy and hyperplasia of the uterine myometrium during pregnancy.
- While hCG indirectly supports this by maintaining the corpus luteum (which produces estrogen and progesterone), it does not directly cause myometrial hypertrophy itself.
*Fetal angiogenesis*
- **Vascular endothelial growth factor (VEGF)** and **fibroblast growth factor (FGF)** are key factors directly involved in fetal angiogenesis (the formation of new blood vessels in the fetus).
- While proper placental function, supported by hCG, is critical for fetal growth, hCG itself is not the direct mediator of fetal angiogenesis.
*Inhibition of ovulation*
- High levels of **estrogen** and **progesterone** (produced by the corpus luteum, maintained by hCG) provide **negative feedback** to the hypothalamus and pituitary, thus inhibiting the release of GnRH, FSH, and LH, which prevents further ovulation.
- hCG itself does not directly inhibit ovulation; rather, it sets in motion the hormonal cascade that leads to its inhibition.
*Stimulation of uterine contractions at term*
- **Oxytocin** is the primary hormone responsible for stimulating uterine contractions, particularly at term, often in conjunction with prostaglandins.
- hCG levels peak early in pregnancy and then decline, and it plays no direct role in stimulating labor contractions.
Parturition physiology US Medical PG Question 6: A 22-year-old woman, gravida 2, para 1, at 41 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been uncomplicated. At the beginning of the second stage of labor, the cervix is 100% effaced and 10 cm dilated; the vertex is at -1 station. The fetal heart rate is reactive with no decelerations. As she pushes, it is noted that the fetal heart rate decreases, as seen on cardiotocography (CTG). Which of the following is the most likely cause of this finding?
- A. Fetal myocardial depression
- B. Maternal hypotension
- C. Placental insufficiency
- D. Umbilical cord compression
- E. Fetal head compression (Correct Answer)
Parturition physiology Explanation: ***Fetal head compression***
- During the second stage of labor, **fetal head compression** commonly occurs with uterine contractions and maternal pushing efforts.
- This compression leads to a reflex vagal response, causing a **decrease in fetal heart rate (early decelerations)**, which is typically benign and resolves after the contraction.
*Fetal myocardial depression*
- **Fetal myocardial depression** can cause a decrease in fetal heart rate, but it is typically associated with **prolonged hypoxia or acidosis** and would likely manifest as late or prolonged decelerations or bradycardia, not just during pushing.
- There are no indications in the scenario of fetal distress or metabolic compromise that would point to myocardial depression.
*Maternal hypotension*
- **Maternal hypotension** would lead to **decreased placental perfusion**, resulting in **late decelerations** due to uteroplacental insufficiency.
- The scenario describes a reactive fetal heart rate with decelerations specifically during pushing, not a pattern consistent with sustained maternal hypotension impacting placental blood flow.
*Placental insufficiency*
- **Placental insufficiency** typically manifests as **late decelerations**, which are gradual decreases in fetal heart rate that begin after the peak of the contraction and return to baseline after the contraction ends.
- The fetal heart rate in the scenario is described as reactive with no decelerations prior to pushing, making placental insufficiency less likely as the primary cause of an acute deceleration during pushing.
*Umbilical cord compression*
- **Umbilical cord compression** causes **variable decelerations**, which are abrupt, often dramatic drops in fetal heart rate.
- While cord compression can occur during labor, the described pattern of deceleration specifically with pushing and the absence of other signs of cord impingement makes head compression a more direct and common cause in this context.
Parturition physiology US Medical PG Question 7: A 28-year-old primigravid woman at 36 weeks' gestation comes to the emergency department for 2 hours of contractions. Her pregnancy has been uncomplicated. The contractions occur once every 20–30 minutes, last less than 30 seconds, and have been consistent in intensity and duration since onset. During that time there has been an increase in fetal movements. Her temperature is 37.1°C (98.8°F), pulse is 98/min, and blood pressure is 104/76 mm Hg. Pelvic examination shows clear cervical mucus and a firm uterus consistent in size with a 36-week gestation. The cervix is 0% effaced and undilated; the vertex is at -3 station. The fetal heart rate is reassuring. After an hour of monitoring in the emergency department, the character of the contractions and pelvic examination findings remain unchanged. Which of the following is the most appropriate next step?
- A. Admit for continuous monitoring
- B. Reassurance and discharge (Correct Answer)
- C. Administer tocolytics
- D. Perform cesarean delivery
- E. Offer local or regional anesthesia
Parturition physiology Explanation: ***Reassurance and discharge***
- The patient's symptoms (contractions every 20-30 minutes, lasting less than 30 seconds, consistent in intensity and duration, **no cervical changes**) are consistent with **Braxton Hicks contractions** rather than true labor.
- Given the reassuring fetal movements, normal vital signs, and unchanged cervical examination after an hour of monitoring, **reassurance and discharge** with instructions to return for signs of true labor are appropriate.
*Admit for continuous monitoring*
- Admission for continuous monitoring is indicated for **true labor**, suspected fetal distress, or complications requiring close observation.
- This patient's findings, including lack of cervical change and stable contraction pattern, do not meet criteria for admission.
*Administer tocolytics*
- **Tocolytics** are used to stop or slow down premature labor.
- This patient is at **36 weeks' gestation** (near term) and is not in true labor, making tocolytic administration inappropriate and unnecessary.
*Perform cesarean delivery*
- **Cesarean delivery** is indicated for obstetric emergencies, fetal distress, or failed vaginal delivery.
- There are no indications for an operative delivery at this time; the patient is not in active labor and both mother and fetus are stable.
*Offer local or regional anesthesia*
- **Local or regional anesthesia** (e.g., epidural) is typically offered for pain management during active labor.
- Since the patient is not in active labor, pain management for labor is not necessary.
Parturition physiology US Medical PG Question 8: A 30-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the hospital for regular, painful contractions that have been increasing in frequency. Her pregnancy has been complicated by gestational diabetes treated with insulin. Pelvic examination shows the cervix is 50% effaced and 4 cm dilated; the vertex is at -1 station. Ultrasonography shows no abnormalities. A tocometer and Doppler fetal heart monitor are placed on the patient's abdomen. The fetal heart rate monitoring strip shows a baseline heart rate of 145/min with a variability of ≥ 15/min. Within a 20-minute recording, there are 7 uterine contractions, 4 accelerations, and 3 decelerations that have a nadir occurring within half a minute. The decelerations occur at differing intervals relative to the contractions. Which of the following is the most appropriate next step in the management of this patient?
- A. Vibroacoustic stimulation
- B. Routine monitoring (Correct Answer)
- C. Administer tocolytics
- D. Emergent cesarean delivery
- E. Placement of fetal scalp electrode
Parturition physiology Explanation: ***Routine monitoring***
- The presented FHR tracing exhibits a **normal baseline rate** (145/min), **moderate variability** (≥15/min), and the presence of **accelerations**, indicating a reassuring fetal status.
- The described decelerations are **variable decelerations** due to their sudden onset, nadir within 30 seconds, and variable relationship to contractions, which are generally benign unless prolonged, deep, or repetitive. Given the otherwise reassuring status, continued routine monitoring is appropriate.
*Vibroacoustic stimulation*
- This intervention is used to elicit **fetal accelerations** or movement during non-stress tests (NSTs) when the fetus is quiet or shows a non-reactive pattern.
- In this case, the fetus is already showing **accelerations** and moderate variability, so stimulation is not needed to assess fetal well-being.
*Administer tocolytics*
- **Tocolytics** are used to stop or slow down labor, typically in cases of preterm labor or uterine tachysystole causing fetal distress.
- This patient is at **38 weeks' gestation** and in active labor, and there are no signs of fetal distress warranting the cessation of contractions.
*Emergent cesarean delivery*
- **Emergent cesarean delivery** is indicated for acute fetal distress, such as prolonged decelerations, significant bradycardia, or absent variability in conjunction with other concerning FHR patterns.
- The FHR tracing described is largely reassuring with moderate variability and accelerations, and the variable decelerations are not indicative of immediate threat, making emergent delivery unnecessary.
*Placement of fetal scalp electrode*
- A **fetal scalp electrode** provides a more accurate and continuous measure of the FHR, often used when external monitoring is difficult or when there are concerns about the reliability of the tracing.
- While it can be useful in some situations, the current tracing is **interpretable as reassuring**, making invasive monitoring currently unnecessary.
Parturition physiology US Medical PG Question 9: Thirty minutes after vaginal delivery of a 2780-g (6-lb 2-oz) newborn at term, a 25-year-old woman, gravida 1, para 1, has heavy vaginal bleeding. Her pregnancy was complicated by pre-eclampsia. Her pulse is 111/min and blood pressure is 95/65 mm Hg. Physical examination shows a fundal height 2 inches below the xiphoid process of the sternum. A drug with which of the following mechanisms of action is most appropriate for this patient?
- A. Activation of phospholipase C (Correct Answer)
- B. Depolarization of the motor end plate
- C. Increased synthesis of cyclic AMP
- D. Inhibition of norepinephrine reuptake
- E. Binding to prostaglandin I2 receptors
Parturition physiology Explanation: ***Activation of phospholipase C***
- This patient presents with **postpartum hemorrhage (PPH)**, characterized by heavy vaginal bleeding, tachycardia, hypotension, and a poorly contracted uterus (normal fundal height is at the umbilicus immediately after delivery; 2 inches below the xiphoid is high indicating uterine atony).
- The most appropriate first-line treatment for uterine atony is **oxytocin**, which acts by binding to G protein-coupled receptors, leading to the **activation of phospholipase C** and an increase in intracellular calcium, causing uterine muscle contraction.
*Depolarization of the motor end plate*
- This mechanism describes the action of **neuromuscular blocking agents** or agonists at the nicotinic acetylcholine receptor, which are not used for treating postpartum hemorrhage.
- The motor end plate is involved in skeletal muscle contraction, not smooth muscle contraction of the uterus.
*Increased synthesis of cyclic AMP*
- **Increased cyclic AMP** generally leads to smooth muscle relaxation (e.g., beta-2 agonists like terbutaline), which would worsen uterine atony and postpartum hemorrhage.
- Tocolytic agents that would cause uterine relaxation would be contraindicated in this scenario.
*Inhibition of norepinephrine reuptake*
- This mechanism describes the action of certain **antidepressants** (e.g., tricyclic antidepressants, SNRIs) or **stimulants**, which primarily affect the central nervous system and are not used to manage postpartum hemorrhage.
- This action does not directly cause uterine contraction.
*Binding to prostaglandin I2 receptors*
- **Prostaglandin I2 (PGI2)**, also known as prostacyclin, is a potent vasodilator and inhibitor of platelet aggregation. Binding to its receptors would lead to smooth muscle relaxation and would increase bleeding, directly worsening postpartum hemorrhage.
- Uterotonic agents like carboprost (PGF2α analog) act on different prostaglandin receptors to induce uterine contraction.
Parturition physiology US Medical PG Question 10: Twenty minutes after delivery of a newborn infant, a 22-year-old woman starts breastfeeding. Initially, the expressed milk is thick and yellowish. Three days later, the mother's breasts swell and the expressed milk becomes thinner and whiter. A decrease in maternal serum concentration of which of the following is most likely responsible for the observed changes in milk production?
- A. Human chorionic gonadotropin
- B. Oxytocin
- C. Thyroxine
- D. Progesterone (Correct Answer)
- E. Estrogen
Parturition physiology Explanation: ***Progesterone***
- The drop in **progesterone** levels after birth removes its inhibitory effect on **milk production**, allowing for the transition from **colostrum** to **mature milk**.
- High levels of **progesterone** during pregnancy inhibit the full effects of **prolactin** on the mammary glands, preventing lactation (lactogenesis II).
- After placental delivery, the dramatic fall in progesterone allows prolactin to stimulate copious milk secretion, typically occurring around day 3-5 postpartum.
*Human chorionic gonadotropin*
- **hCG** maintains the corpus luteum during early pregnancy but is not directly involved in the regulation of postpartum milk production.
- Its levels decrease significantly after delivery, but this decrease is not the primary driver of milk changes.
*Oxytocin*
- **Oxytocin** is responsible for **milk ejection (let-down)**, not milk production or changes in milk composition.
- Its levels tend to increase during breastfeeding due to suckling, rather than decrease.
*Thyroxine*
- **Thyroxine** (thyroid hormones) is essential for overall metabolism and can affect milk supply, but a decrease in its levels is not primarily responsible for the switch from colostrum to mature milk.
- Decreased thyroxine would more likely lead to *reduced* milk production or broader metabolic disturbances.
*Estrogen*
- **Estrogen** levels decrease significantly after delivery, similar to progesterone, but progesterone's inhibitory effect on lactation is more direct and critical for the transition in milk type.
- While high estrogen during pregnancy also inhibits lactation, the removal of progesterone's block is the key trigger for copious milk secretion.
More Parturition physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.