Maternal physiological adaptations to pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Maternal physiological adaptations to pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Maternal physiological adaptations to pregnancy US Medical PG Question 1: A 25-year-old G2P1 woman at 12 weeks gestational age presents to the office to discuss the results of her routine prenatal screening labs, which were ordered during her 1st prenatal visit. She reports taking a daily prenatal vitamin but no other medications. She complains of mild fatigue and appears pale on exam. Her complete blood count (CBC) shows the following:
Hemoglobin (Hb) 9.5 g/dL
Hematocrit 29%
Mean corpuscular volume (MCV) 75 µm3
Which of the following are the most likely hematologic states of the patient and her fetus?
- A. Iron deficiency anemia in both the mother and the fetus
- B. Iron deficiency anemia in the mother; normal Hb levels in the fetus (Correct Answer)
- C. Pernicious anemia in the mother; normal Hb levels in the fetus
- D. Physiologic anemia in the mother; normal Hb levels in the fetus
- E. Folate deficiency anemia in both the mother and the fetus
Maternal physiological adaptations to pregnancy Explanation: ***Iron deficiency anemia in the mother; normal Hb levels in the fetus***
- The mother's lab values (Hb 9.5 g/dL, MCV 75 µm3) indicate **microcytic, hypochromic anemia**, consistent with **iron deficiency anemia**.
- The fetus prioritizes iron uptake, even in cases of severe maternal iron deficiency, meaning the **fetal hemoglobin levels** are typically normal unless maternal iron deficiency is profound and prolonged.
*Iron deficiency anemia in both the mother and the fetus*
- While the mother clearly has **iron deficiency anemia**, the fetus generally maintains **normal hemoglobin levels** by actively drawing iron from the mother, even at her expense.
- Fetal iron deficiency leading to anemia is rare unless maternal deficiency is extremely severe and prolonged, which is not indicated here.
*Pernicious anemia in the mother; normal Hb levels in the fetus*
- **Pernicious anemia** (vitamin B12 deficiency) typically presents as **macrocytic anemia** (high MCV), which contradicts the patient's MCV of 75 µm3 (microcytic).
- Although the fetus would likely have normal Hb levels in maternal pernicious anemia, the mother's lab findings do not support this diagnosis.
*Physiologic anemia in the mother; normal Hb levels in the fetus*
- **Physiologic anemia of pregnancy** is caused by a disproportionate increase in plasma volume compared to red blood cell mass, resulting in **dilutional anemia**, but usually with a **normal MCV**.
- The patient's **low MCV (75 µm3)** indicates a microcytic anemia, which is not characteristic of physiologic anemia of pregnancy.
*Folate deficiency anemia in both the mother and the fetus*
- **Folate deficiency anemia** is a type of **macrocytic anemia** (high MCV), which is inconsistent with the patient's MCV of 75 µm3.
- While severe maternal folate deficiency can affect the fetus, the maternal blood picture does not support this diagnosis.
Maternal physiological adaptations to pregnancy US Medical PG Question 2: A 27-year-old woman, gravida 2, para 1, at 26 weeks' gestation comes to the emergency department because of vaginal bleeding and epistaxis for the past 2 days. She missed her last prenatal visit 2 weeks ago. Physical examination shows blood in the posterior pharynx and a uterus consistent in size with 23 weeks' gestation. Her hemoglobin concentration is 7.2 g/dL. Ultrasonography shows an intrauterine pregnancy with a small retroplacental hematoma and absent fetal cardiac activity. Further evaluation is most likely to show which of the following findings?
- A. Decreased fibrinogen concentration (Correct Answer)
- B. Increased antithrombin concentration
- C. Increased factor V concentration
- D. Increased platelet count
- E. Decreased prothrombin time
Maternal physiological adaptations to pregnancy Explanation: ***Decreased fibrinogen concentration***
- The patient's presentation with **vaginal bleeding**, **epistaxis**, a **small retroplacental hematoma**, and **absent fetal cardiac activity** strongly suggests **abruptio placentae** complicated by **disseminated intravascular coagulation (DIC)**.
- In DIC, widespread activation of the **coagulation cascade** leads to consumption of clotting factors, including **fibrinogen**, resulting in **decreased plasma levels**.
*Increased antithrombin concentration*
- **Antithrombin** is a natural anticoagulant that inhibits activated clotting factors; its concentration is typically **decreased** in DIC due to its consumption in an attempt to control widespread coagulation.
- An increase in antithrombin would generally **reduce** clot formation, which is contrary to the hypercoagulable state seen initially in DIC.
*Increased factor V concentration*
- **Factor V** is a procoagulant factor that is **consumed** during DIC, leading to **decreased** rather than increased concentrations.
- Increased factor V would promote clotting, which is overridden by the massive consumption of factors and platelets in DIC.
*Increased platelet count*
- **Platelets** are actively consumed in the widespread microthrombi formation characteristic of DIC, leading to **thrombocytopenia** (decreased platelet count), not an increase.
- An increased platelet count would be protective against bleeding, which is not the case here.
*Decreased prothrombin time*
- **Prothrombin time (PT)** measures the extrinsic and common coagulation pathways; in DIC, the consumption of coagulation factors, including **prothrombin**, leads to a **prolonged (increased)** PT, not a decreased one.
- A decreased PT would indicate a hypercoagulable state with enhanced clotting factor activity, which is eventually exhausted in DIC.
Maternal physiological adaptations to pregnancy US Medical PG Question 3: A 26-year-old woman, gravida 2, para 1, at 28 weeks' gestation comes to the physician for a prenatal visit. She feels well. Pregnancy and delivery of her first child were uncomplicated. Her temperature is 37.2°C (99°F) and blood pressure is 163/105 mm Hg. Her blood pressure 10 weeks ago was 128/84 mm Hg. At her last visit two weeks ago, her blood pressure was 142/92 mm Hg. Pelvic examination shows a uterus consistent in size with a 28-week gestation. A complete blood count and serum concentrations of electrolytes, creatinine, and hepatic transaminases are within the reference range. A urinalysis is within normal limits. Which of the following is the most appropriate next step in management?
- A. Oral labetalol therapy (Correct Answer)
- B. Lisinopril therapy
- C. Magnesium sulfate therapy
- D. Complete bed rest
- E. Dietary salt restriction
Maternal physiological adaptations to pregnancy Explanation: **Oral labetalol therapy**
- The patient has developed **gestational hypertension** (blood pressure ≥140/90 mmHg on two occasions at least 4 hours apart after 20 weeks gestation, without proteinuria or other signs of preeclampsia), with her current BP of 163/105 mmHg confirming **severe range hypertension** (systolic ≥160 mmHg or diastolic ≥110 mmHg).
- **Labetalol** is a first-line agent for managing hypertension in pregnancy due to its established safety profile and efficacy in lowering blood pressure.
*Lisinopril therapy*
- **Angiotensin-converting enzyme (ACE) inhibitors** like lisinopril are **contraindicated in pregnancy** as they can cause fetal renal dysfunction, oligohydramnios, and neonatal hypotension.
- This medication choice would be harmful to the fetus.
*Magnesium sulfate therapy*
- **Magnesium sulfate** is indicated for the **prevention and treatment of seizures in preeclampsia/eclampsia**, not for blood pressure control itself.
- While the patient has hypertension, there are no signs of preeclampsia (e.g., proteinuria, signs of end-organ damage), making magnesium sulfate inappropriate at this stage.
*Complete bed rest*
- **Complete bed rest** is no longer recommended for the management of gestational hypertension or preeclampsia, as studies have shown it does not improve maternal or fetal outcomes and can increase the risk of **thromboembolism**.
- It can also negatively impact a patient's quality of life without providing therapeutic benefit.
*Dietary salt restriction*
- While generally recommended for hypertension outside of pregnancy, **severe salt restriction** in pregnancy is **not typically recommended** for gestational hypertension or preeclampsia, as it has not been shown to improve outcomes and could potentially worsen maternal fluid balance.
- The primary management for severe range gestational hypertension involves antihypertensive medications.
Maternal physiological adaptations to pregnancy US Medical PG Question 4: A 32-year-old female presents to her obstetrician 3 weeks postpartum for failure to lactate. Of note, she has been unable to tolerate cold environments since the birth of her child. Review of systems is positive for fatigue, lightheadedness, and a 3-pound weight gain over the last 3 weeks. Her delivery was complicated by placenta accreta with postpartum blood loss. Her newborn infant is doing well on formula. She denies any personal or family history of thyroid disease. Physical exam is overall unremarkable. On a panel of hormone testing, which of the following levels is most likely to be normal in this patient?
- A. Thyroid hormone
- B. Cortisol
- C. Luteinizing hormone
- D. Antidiuretic hormone (Correct Answer)
- E. Aldosterone
Maternal physiological adaptations to pregnancy Explanation: ***Antidiuretic hormone***
- This patient is presenting with symptoms consistent with **Sheehan syndrome**, which is postpartum pituitary necrosis due to severe hemorrhage and hypovolemic shock.
- Sheehan syndrome **primarily affects the anterior pituitary**, where most pituitary hormones are produced.
- **Antidiuretic hormone (ADH)** is synthesized by the **hypothalamus** and stored/released by the **posterior pituitary**, which is typically **spared** in Sheehan syndrome due to its separate blood supply.
- Therefore, **ADH levels would be normal** in this patient, making this the correct answer.
*Aldosterone*
- The **renin-angiotensin-aldosterone system (RAAS)** is regulated independently by the kidneys and is preserved in pituitary disorders.
- Aldosterone levels would also likely be **normal** in this patient.
- However, ADH is the better answer as it specifically demonstrates the anatomical distinction between anterior and posterior pituitary function.
*Thyroid hormone*
- The **anterior pituitary** fails to produce **thyroid-stimulating hormone (TSH)** in Sheehan syndrome, leading to secondary hypothyroidism.
- This results in **low thyroid hormone levels**.
- Her symptoms of **cold intolerance**, **fatigue**, and **weight gain** are classic manifestations of hypothyroidism.
*Cortisol*
- The anterior pituitary produces **adrenocorticotropic hormone (ACTH)**, which stimulates cortisol release from the adrenal glands.
- In Sheehan syndrome, failure of ACTH production leads to **secondary adrenal insufficiency** with **low cortisol levels**.
- This contributes to her **fatigue** and **lightheadedness**.
*Luteinizing hormone*
- The anterior pituitary produces **luteinizing hormone (LH)**, which is crucial for ovarian function and ovulation.
- The patient's **failure to lactate** is due to **prolactin deficiency** (another anterior pituitary hormone), not LH deficiency.
- Lack of LH and other gonadotropins would contribute to amenorrhea and loss of reproductive function that often accompany Sheehan syndrome.
Maternal physiological adaptations to pregnancy US Medical PG Question 5: A 42-year-old G1P0 woman presents to an obstetrician for her first prenatal visit. She has been pregnant for about 10 weeks and is concerned about how pregnancy will affect her health. Specifically, she is afraid that her complicated medical history will be adversely affected by her pregnancy. Her past medical history is significant for mild polycythemia, obesity hypoventilation syndrome, easy bleeding, multiple sclerosis, and aortic regurgitation. Which of these disorders is most likely to increase in severity during the course of the pregnancy?
- A. Easy bleeding
- B. Hypoventilation (Correct Answer)
- C. Multiple sclerosis
- D. Polycythemia
- E. Heart murmur
Maternal physiological adaptations to pregnancy Explanation: ***Hypoventilation***
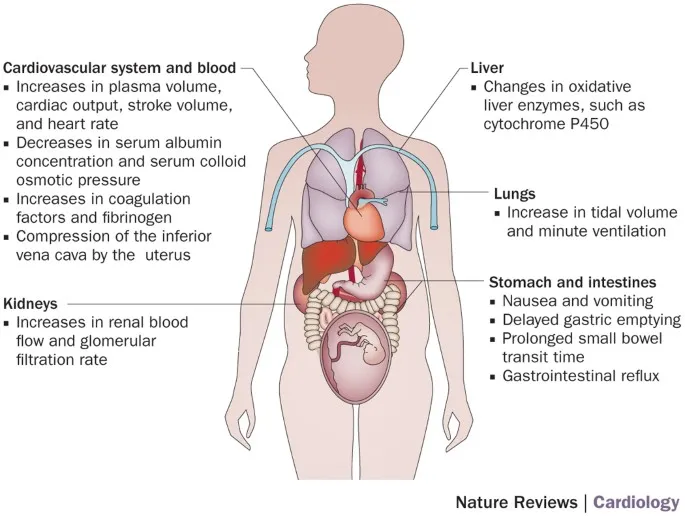
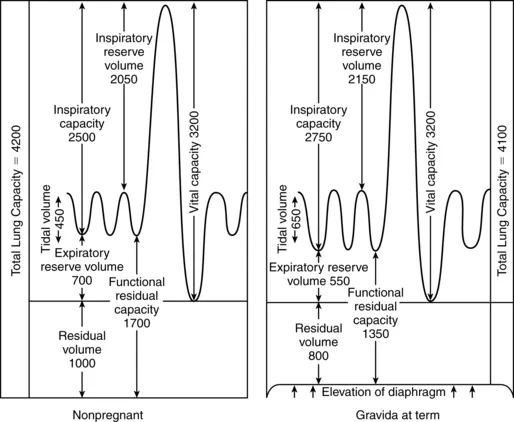
- Pregnancy leads to increased **oxygen consumption** and **carbon dioxide production**, requiring increased ventilation.
- In a patient with **obesity hypoventilation syndrome**, the already compromised respiratory drive and mechanics can worsen, leading to increased **hypercapnia** and **hypoxia**.
*Easy bleeding*
- Pregnancy is a **hypercoagulable state**, which typically reduces the risk of bleeding.
- While certain pregnancy complications (e.g., placental abruption) can cause bleeding, the overall physiological changes tend to **decrease primary bleeding tendencies**.
*Multiple sclerosis*
- Pregnancy typically has an **immunomodulatory effect** that can lead to a decrease in the frequency of MS relapses, especially in the third trimester.
- Relapses may increase postpartum, but during pregnancy itself, the condition often **stabilizes or improves**.
*Polycythemia*
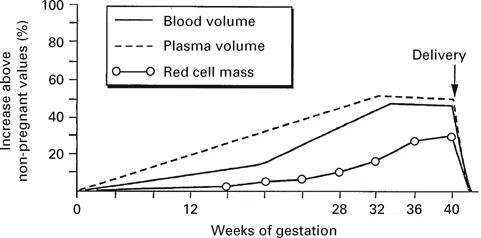
- Pregnancy increases **plasma volume** significantly, which can lead to a relative **hemodilution**.
- This physiological change would likely **ameliorate mild polycythemia** rather than worsen it.
*Heart murmur*
- The murmur is due to **aortic regurgitation**, and while pregnancy increases **cardiac output** and **blood volume**, severe aortic regurgitation can worsen.
- However, the overall physiological changes of pregnancy result in **increased minute ventilation**, making hypoventilation a more direct and universally worsened problem with existing **obesity hypoventilation syndrome**.
Maternal physiological adaptations to pregnancy US Medical PG Question 6: A 36-year-old woman, gravida 2, para 1, at 30 weeks' gestation comes to the physician for evaluation of increased urinary frequency. She has no history of major medical illness. Physical examination shows no abnormalities. Laboratory studies show an increased serum C-peptide concentration. Ultrasonography shows polyhydramnios and a large for gestational age fetus. Which of the following hormones is predominantly responsible for the observed laboratory changes in this patient?
- A. Human placental lactogen (Correct Answer)
- B. Adrenocorticotropic hormone
- C. Human chorionic gonadotropin
- D. Progesterone
- E. Estrogen
Maternal physiological adaptations to pregnancy Explanation: ***Human placental lactogen***
- **Human placental lactogen (hPL)**, also known as **chorionic somatomammotropin**, is produced by the placenta and has **anti-insulin effects**, increasing maternal blood glucose to prioritize fetal nutrient supply.
- This **insulin resistance** leads to increased maternal insulin production (reflected by **elevated C-peptide**) to compensate, and if inadequate, results in **gestational diabetes mellitus (GDM)**, which explains the **polyhydramnios** and **large for gestational age fetus**.
*Adrenocorticotropic hormone*
- **ACTH** stimulates the **adrenal cortex** to produce **cortisol**, which also has diabetogenic effects.
- However, **hPL** is the primary hormone responsible for the **insulin resistance** of pregnancy and the associated elevated C-peptide and GDM features (polyhydramnios and large for gestational age fetus) in this context.
*Human chorionic gonadotropin*
- **hCG** is crucial for maintaining the **corpus luteum** in early pregnancy, stimulating **progesterone** production, and is used as a marker for pregnancy.
- It does not directly cause the **insulin resistance** or significantly elevate C-peptide that leads to the observed findings of **polyhydramnios** and a **large for gestational age fetus**.
*Progesterone*
- **Progesterone** is essential for maintaining pregnancy by promoting **endometrial growth** and suppressing uterine contractions.
- While it plays a role in some metabolic changes during pregnancy, it is not the primary hormone responsible for the **insulin-antagonistic effects** that lead to the elevated C-peptide and signs of GDM described.
*Estrogen*
- **Estrogen** promotes uterine growth, maintains the **endometrium**, and plays a role in fetal development and the development of maternal secondary sexual characteristics.
- While it contributes to metabolic changes in pregnancy, it is not the main hormone responsible for the **insulin resistance** and related features like elevated C-peptide, polyhydramnios, and a large for gestational age fetus seen in this patient.
Maternal physiological adaptations to pregnancy US Medical PG Question 7: A 38-year-old woman, gravida 2, para 1, at 32 weeks' gestation comes to the physician because of a 1-day history of dyspnea and left-sided chest pain that is worse when she breathes deeply. One week ago, she returned from a trip to Chile, where she had a 3-day episode of flu-like symptoms that resolved without treatment. Pregnancy and delivery of her first child were uncomplicated. She has no history of serious illness. Her temperature is 37.2°C (99°F), pulse is 118/min, respirations are 28/min and slightly labored, and blood pressure is 110/76 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 91%. Examination shows jugular venous distention and bilateral pitting edema below the knees that is worse on the left-side. There is decreased breath sounds over the left lung base. The uterus is consistent in size with a 32-week gestation. The remainder of the examination shows no abnormalities. Further evaluation of this patient is most likely to show which of the following findings?
- A. Protein dipstick test of 2+ on urinalysis
- B. Depression of the PR segment on electrocardiography
- C. Decreased fibrinogen levels on serum analysis
- D. Decreased myocardial perfusion on a cardiac PET scan
- E. Noncompressible femoral vein on ultrasonography (Correct Answer)
Maternal physiological adaptations to pregnancy Explanation: **Noncompressible femoral vein on ultrasonography**
- The patient's symptoms (dyspnea, pleuritic chest pain, tachypnea, tachycardia, hypoxemia, JVD, and unilateral leg edema) are highly suggestive of **pulmonary embolism (PE)**, especially given her recent travel and pregnancy. A noncompressible femoral vein on ultrasonography indicates a **deep vein thrombosis (DVT)**, which is the most common cause of PE.
- Pregnancy is a **hypercoagulable state**, increasing the risk of venous thromboembolism. The unilateral leg edema further supports the presence of a DVT.
*Protein dipstick test of 2+ on urinalysis*
- While preeclampsia can manifest with dyspnea due to pulmonary edema, her **blood pressure of 110/76 mm Hg is normal**, and she has no other signs of preeclampsia.
- **Proteinuria** would be a key finding in preeclampsia, but it is not directly linked to the acute pleuritic chest pain and hypoxemia seen here.
*Depression of the PR segment on electrocardiography*
- **PR segment depression** can be seen in **pericarditis**, which typically causes sharp, pleuritic chest pain that improves when leaning forward and is associated with a pericardial friction rub.
- The patient's presentation, particularly the unilateral leg edema and hypoxemia, is not typical for pericarditis.
*Decreased fibrinogen levels on serum analysis*
- **Decreased fibrinogen levels** are characteristic of **disseminated intravascular coagulation (DIC)**, which is a severe complication and would present with widespread bleeding or thrombotic events.
- While DIC can occur in pregnancy complications, it does not typically cause isolated acute PE symptoms and would not be the most likely initial finding in this scenario.
*Decreased myocardial perfusion on a cardiac PET scan*
- **Decreased myocardial perfusion** indicates **myocardial ischemia or infarction**, which usually presents with substernal chest pain, often radiating, and characteristic ECG changes.
- Although PE can cause right ventricular strain, the primary pathology is in the pulmonary vasculature, not directly in myocardial perfusion as the leading cause of her acute symptoms.
Maternal physiological adaptations to pregnancy US Medical PG Question 8: A 60-year-old male engineer who complains of shortness of breath when walking a few blocks undergoes a cardiac stress test because of concern for coronary artery disease. During the test he asks his cardiologist about what variables are usually used to quantify the functioning of the heart. He learns that one of these variables is stroke volume. Which of the following scenarios would be most likely to lead to a decrease in stroke volume?
- A. Anxiety
- B. Heart failure (Correct Answer)
- C. Exercise
- D. Pregnancy
- E. Digitalis
Maternal physiological adaptations to pregnancy Explanation: ***Heart failure***
- In **heart failure**, the heart's pumping ability is impaired, leading to a reduced **ejection fraction** and thus a decreased **stroke volume**.
- The weakened myocardium cannot effectively contract to expel the normal volume of blood, resulting in lower blood output per beat.
*Anxiety*
- **Anxiety** typically causes an increase in **sympathetic nervous system** activity, leading to increased heart rate and myocardial contractility.
- This often results in a temporary **increase in stroke volume** due to enhanced cardiac performance, not a decrease.
*Exercise*
- During **exercise**, there is a significant **increase in venous return** and sympathetic stimulation, leading to increased **end-diastolic volume** and contractility.
- This physiological response causes a substantial **increase in stroke volume** to meet the body's higher oxygen demands.
*Pregnancy*
- **Pregnancy** leads to significant **physiological adaptations** to accommodate the growing fetus, including a substantial increase in **blood volume**.
- This increased blood volume and cardiac output result in an **increase in stroke volume** to maintain adequate perfusion for both mother and fetus.
*Digitalis*
- **Digitalis** is a cardiac glycoside that **increases intracellular calcium** in myocardial cells, enhancing the **force of contraction**.
- This positive inotropic effect leads to an **increased stroke volume** by improving the heart's pumping efficiency.
Maternal physiological adaptations to pregnancy US Medical PG Question 9: Activation of the renin-angiotensin-aldosterone system yields a significant physiological effect on renal blood flow and filtration. Which of the following is most likely to occur in response to increased levels of Angiotensin-II?
- A. Decreased renal plasma flow, decreased filtration fraction
- B. Decreased renal plasma flow, increased glomerular capillary oncotic pressure
- C. Increased renal plasma flow, decreased filtration fraction
- D. Increased renal plasma flow, increased filtration fraction
- E. Decreased renal plasma flow, increased filtration fraction (Correct Answer)
Maternal physiological adaptations to pregnancy Explanation: ***Decreased renal plasma flow, increased filtration fraction***
- **Angiotensin II** causes **efferent arteriolar constriction**, which reduces blood flow leaving the glomerulus, thereby **decreasing renal plasma flow**.
- This efferent constriction also increases **glomerular hydrostatic pressure** and reduces plasma flow distal to the glomerulus, leading to a **higher filtration fraction** (GFR/RPF).
*Decreased renal plasma flow, decreased filtration fraction*
- While **renal plasma flow decreases**, a **decreased filtration fraction** would imply that either GFR decreases disproportionately more than RPF or GFR does not increase despite the RPF reduction, which is not the typical response to **angiotensin II** due to its predominant effect on the **efferent arteriole**.
*Decreased renal plasma flow, increased glomerular capillary oncotic pressure*
- **Increased glomerular capillary oncotic pressure** is a consequence of increased filtration fraction, as more fluid is filtered out, leaving behind a more concentrated plasma. This option includes a correct element (decreased RPF) but pairs it with a less direct and defining outcome of acute Angiotensin II action as the primary physiological effect.
*Increased renal plasma flow, decreased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, predominantly of the efferent arteriole, which by definition would **decrease renal plasma flow**, not increase it.
- A **decreased filtration fraction** would be inconsistent with efferent arteriolar constriction which typically raises GFR relative to RPF.
*Increased renal plasma flow, increased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, leading to a **decrease in renal plasma flow**, not an increase.
- While **filtration fraction is increased**, the initial premise of increased renal plasma flow is incorrect.
Maternal physiological adaptations to pregnancy US Medical PG Question 10: A newborn whose mother had uncontrolled diabetes mellitus during pregnancy is likely to have which of the following findings?
- A. Amyloid deposits in pancreatic islets
- B. Atrophy of pancreatic islets cells
- C. Hyperglycemia
- D. Ketoacidosis
- E. Hypoglycemia (Correct Answer)
Maternal physiological adaptations to pregnancy Explanation: ***Hypoglycemia***
- Uncontrolled maternal diabetes leads to **fetal hyperglycemia**, causing the fetal pancreas to produce **excessive insulin** (fetal hyperinsulinism) to compensate.
- After birth, the maternal glucose supply is cut off, but the newborn's pancreas continues to overproduce insulin, leading to **rapid drops in blood glucose** and severe hypoglycemia.
*Amyloid deposits in pancreatic islets*
- **Amyloid deposits** in pancreatic islets are characteristic of **Type 2 Diabetes Mellitus** in adults, typically not seen in newborns or as a direct consequence of maternal diabetes.
- This condition involves the accumulation of **islet amyloid polypeptide (IAPP)**, which is different from the physiological responses seen in infants of diabetic mothers.
*Atrophy of pancreatic islets cells*
- **Atrophy of pancreatic islet cells** is seen in late-stage **Type 1 Diabetes Mellitus** due to autoimmune destruction, not in infants of diabetic mothers, who typically have hypertrophied islets.
- In newborns of diabetic mothers, the pancreatic beta cells are usually **hypertrophic and hyperplastic** due to chronic glucose stimulation.
*Hyperglycemia*
- While the fetus experiences **hyperglycemia** in utero due to maternal diabetes, the newborn after birth typically develops **hypoglycemia** once the continuous maternal glucose supply is removed.
- The newborn's elevated insulin levels, in response to chronic fetal hyperglycemia, quickly deplete available glucose post-delivery, leading to low blood sugar.
*Ketoacidosis*
- **Ketoacidosis** occurs when the body produces high levels of **ketones** due to severe insulin deficiency and high glucose, which is primarily seen in **Type 1 Diabetes Mellitus** or severe stress states.
- Newborns of diabetic mothers are more prone to hypoglycemia due to **hyperinsulinism**, which inhibits ketogenesis, rather than ketoacidosis.
More Maternal physiological adaptations to pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.