Implantation physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Implantation physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Implantation physiology US Medical PG Question 1: Fertilization begins when sperm binds to the corona radiata of the egg. Once the sperm enters the cytoplasm, a cortical reaction occurs which prevents other sperm from entering the oocyte. The oocyte then undergoes an important reaction. What is the next reaction that is necessary for fertilization to continue?
- A. The second meiotic division (Correct Answer)
- B. Degeneration of the sperm tail
- C. Release of a polar body
- D. Formation of the spindle apparatus
- E. Acrosome reaction
Implantation physiology Explanation: ***The second meiotic division***
- Upon **sperm penetration**, the secondary oocyte completes its **meiosis II**, forming a mature ovum and a second polar body.
- This completion of meiosis II is a critical step for the pronuclear fusion and subsequent **zygote formation**.
*Degeneration of the sperm tail*
- While the sperm tail does degenerate within the ooplasm, it occurs **after** the genetic material has been released and is not the immediate next critical reaction for continued fertilization.
- This is a process of degradation and assimilation, not an active cellular reaction of the oocyte vital for fertilization progression.
*Release of a polar body*
- The first polar body is released **before fertilization** (at the completion of meiosis I), and the second polar body is released **concomitantly with the completion of meiosis II**, which is the required reaction.
- Releasing a polar body is a consequence of meiotic division, not an independent reaction that drives fertilization forward.
*Formation of the spindle apparatus*
- The **spindle apparatus** is formed during both meiotic divisions to separate chromosomes, but its formation itself is not the immediate "next reaction" necessary for fertilization to continue after cortical reaction.
- The key event is the progression of meiosis, which the spindle facilitates, not the mere formation of the apparatus.
*Acrosome reaction*
- The **acrosome reaction** occurs **before** the sperm binds to the zona pellucida and penetrates the oocyte, enabling the release of enzymes to digest the egg's outer layers.
- This reaction has already taken place for the sperm to have entered the oocyte and initiated the cortical reaction.
Implantation physiology US Medical PG Question 2: A 22-year-old female presents to her PCP after having unprotected sex with her boyfriend 2 days ago. She has been monogamous with her boyfriend but is very concerned about pregnancy. The patient requests emergency contraception to decrease her likelihood of getting pregnant. A blood hCG test returns negative. The PCP prescribes the patient ethinyl estradiol 100 mcg and levonorgestrel 0.5 mg to be taken 12 hours apart. What is the most likely mechanism of action for this combined prescription?
- A. Inhibition or delayed ovulation (Correct Answer)
- B. Interference of corpus luteum function
- C. Thickening of cervical mucus with sperm trapping
- D. Tubal constriction inhibiting sperm transportation
- E. Alteration of the endometrium impairing implantation of the fertilized egg
Implantation physiology Explanation: ***Inhibition or delayed ovulation***
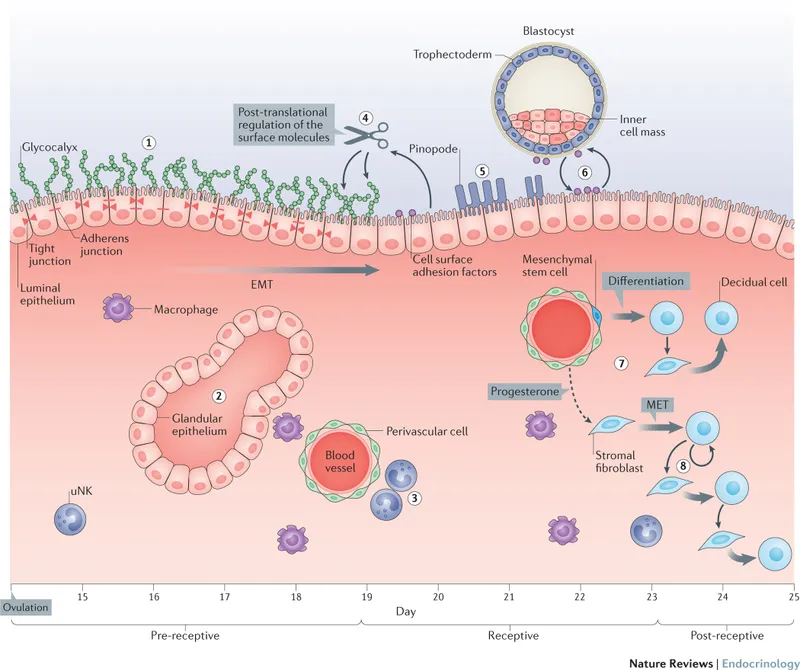
- The high doses of **estrogen** and **progestin** in the combined emergency contraception pill primarily act by suppressing the **luteinizing hormone (LH) surge**, which is essential for ovulation.
- By inhibiting or delaying ovulation, the pill prevents the release of an egg, thus preventing fertilization since sperm cannot meet an egg.
*Interference of corpus luteum function*
- While hormonal contraceptives can affect the **corpus luteum**, high-dose emergency contraception primarily acts *before* the formation of a mature corpus luteum by preventing ovulation itself.
- Once the corpus luteum is formed, its function is usually maintained if pregnancy occurs, and emergency contraception given *after* implantation is generally ineffective at terminating a pregnancy.
*Thickening of cervical mucus with sperm trapping*
- This is a well-known mechanism of action for *continuous* hormonal contraception (e.g., daily birth control pills), where lower, consistent doses of progestin make cervical mucus impenetrable to sperm.
- While it might play a *minor* role, it is not the primary mechanism of action for high-dose emergency contraception administered acutely, which mainly targets ovulation.
*Tubal constriction inhibiting sperm transportation*
- There is no strong evidence to suggest that combined emergency contraception pills cause **tubal constriction** to significantly impair sperm or egg transport.
- The main sites of action are the **hypothalamic-pituitary-ovarian axis** (for ovulation) and possibly the endometrium (for implantation), not direct tubal motility.
*Alteration of the endometrium impairing implantation of the fertilized egg*
- While hormonal contraceptives can alter the **endometrium** making it less receptive to implantation, this is considered a *secondary* or less significant mechanism for combined emergency contraception.
- The primary goal and most effective action of these pills is to prevent fertilization by inhibiting ovulation, especially when taken shortly after unprotected intercourse and before implantation.
Implantation physiology US Medical PG Question 3: A 19-year-old female complains of abnormal facial hair growth. This has been very stressful for her, especially in the setting of not being happy with her weight. Upon further questioning you learn she has a history of type 2 diabetes mellitus. Her height is 61 inches, and weight is 185 pounds (84 kg). Physical examination is notable for facial hair above her superior lip and velvety, greyish thickened hyperpigmented skin in the posterior neck. Patient is started on a hormonal oral contraceptive. Which of the following is a property of the endometrial protective hormone found in this oral contraceptive?
- A. Enhances tubal motility
- B. Thickens cervical mucus (Correct Answer)
- C. Increases bone fractures
- D. Decreases LDL
- E. Decreases thyroid binding globulin
Implantation physiology Explanation: ***Thickens cervical mucus***
- The endometrial protective hormone in this oral contraceptive is **progestin**, which acts by **thickening cervical mucus**, making it impenetrable to sperm and thus preventing fertilization.
- This action is a key mechanism by which combined oral contraceptives prevent pregnancy, along with inhibiting ovulation.
*Enhances tubal motility*
- **Estrogen**, found in combined oral contraceptives, generally enhances tubal motility, but progestin's primary action for contraception is not tubal enhancement but rather making the cervical mucus inhospitable.
- Increased tubal motility could theoretically aid sperm transport or ovum capture, which is counterproductive to contraception.
*Increases bone fractures*
- **Hormonal contraceptives**, particularly combined oral contraceptives, are not typically associated with an **increased risk of bone fractures**; in fact, some studies suggest a protective or neutral effect on bone mineral density.
- **Estrogen** in combined oral contraceptives generally has a protective effect on bone density.
*Decreases LDL*
- While some hormonal therapies can impact lipid profiles, **oral contraceptives**, particularly those with certain progestins, can sometimes lead to a **slight increase in LDL** (low-density lipoprotein) and triglycerides, while estrogen components can elevate HDL.
- The net effect on LDL is not typically a decrease; therefore, this is not a property of the progestin component providing endometrial protection.
*Decreases thyroid binding globulin*
- **Estrogen** in oral contraceptives **increases the synthesis of thyroid-binding globulin (TBG)**, leading to higher total thyroid hormone levels, although free thyroid hormone levels usually remain normal.
- Progestins do not decrease TBG; therefore, this statement is incorrect.
Implantation physiology US Medical PG Question 4: Research is being conducted on embryoblasts. The exact date of fertilization is unknown. There is the presence of a cytotrophoblast and syncytiotrophoblast, marking the time when implantation into the uterus would normally occur. Within the embryoblast, columnar and cuboidal cells are separated by a membrane. Which of these cell layers begins to line the yolk sac cavity?
- A. Hypoblast (Correct Answer)
- B. Epiblast
- C. Syncytiotrophoblast
- D. Inner cell mass
- E. Endoderm
Implantation physiology Explanation: ***Hypoblast***
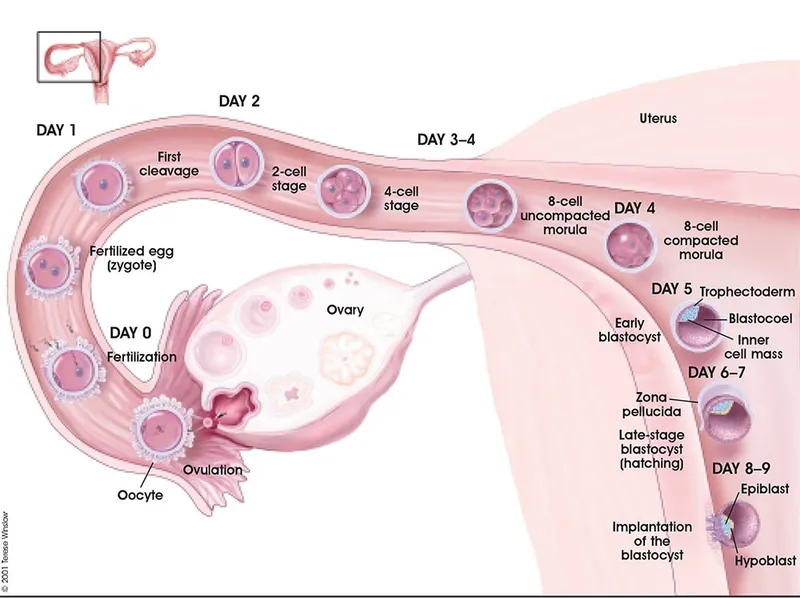
- The **hypoblast** is a layer of cuboidal cells that forms from the inner cell mass around day 8 post-fertilization.
- It plays a crucial role in forming the **primary yolk sac** by migrating to line the exocoelomic cavity.
*Epiblast*
- The **epiblast** is composed of columnar cells located dorsal to the hypoblast and forms the floor of the **amniotic cavity**.
- It is the source of the **three primary germ layers** during gastrulation (ectoderm, mesoderm, and endoderm), not the yolk sac lining itself.
*Syncytiotrophoblast*
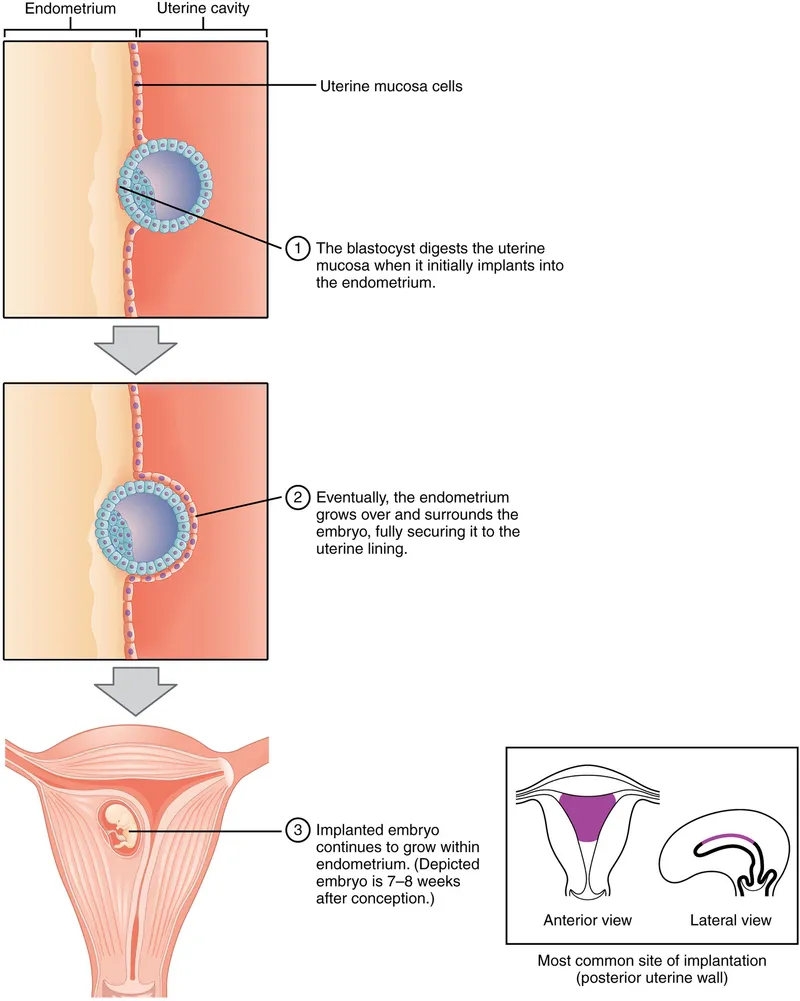
- The **syncytiotrophoblast** is the outer, invasive layer of the trophoblast that facilitates implantation and forms the fetal component of the placenta.
- It is not involved in lining the yolk sac cavity but rather in **invading the uterine endometrium** and producing hCG.
*Inner cell mass*
- The **inner cell mass (ICM)** is the cluster of cells within the blastocyst that gives rise to the embryoblast (which further differentiates into epiblast and hypoblast).
- The ICM itself does not line the yolk sac; rather, its derivative, the hypoblast, does.
*Endoderm*
- The **endoderm** is one of the three primary germ layers that forms during gastrulation from the epiblast derivative.
- It ultimately forms the linings of the **gastrointestinal and respiratory tracts**, not the primary yolk sac lining.
Implantation physiology US Medical PG Question 5: A 26-year-old woman comes to the physician because she has not had a menstrual period for 5 weeks. Menarche was at the age of 14 years and menses occurred at regular 30-day intervals. She reports having unprotected sexual intercourse 3 weeks ago. A urine pregnancy test is positive. Which of the following best describes the stage of development of the embryo at this time?
- A. Fetal heart is beating, but cardiac activity is not yet visible on ultrasound
- B. Limb buds have formed, but fetal movements have not begun
- C. Sexual differentiation has begun, but fetal movement has not started
- D. Neural crest has formed, but limb buds have not yet formed (Correct Answer)
- E. Implantation has occurred, but notochord has not yet formed
Implantation physiology Explanation: ***Neural crest has formed, but limb buds have not yet formed***
- At **5 weeks gestational age (3 weeks post-fertilization)**, neurulation is completing or recently completed
- **Neural crest cells** migrate from the neural folds during weeks 3-4 post-fertilization and are definitely present by this time
- **Limb buds** appear later, around week 4-5 post-fertilization (week 6-7 gestational age), making this the most accurate description for the current developmental stage
*Fetal heart is beating, but cardiac activity is not yet visible on ultrasound*
- The primitive heart tube begins contracting around day 22-23 post-fertilization (early week 4)
- At 3 weeks post-fertilization (5 weeks gestational age), the heart may just be starting to beat, but this timing is less precise
- Cardiac activity becomes visible on transvaginal ultrasound around 5.5-6 weeks gestational age, so this option is close but less precise than the correct answer
*Limb buds have formed, but fetal movements have not begun*
- **Limb buds** typically appear around week 4-5 post-fertilization (week 6-7 gestational age)
- This is **too advanced** for 3 weeks post-fertilization
- While fetal movements aren't perceptible to the mother until 16-20 weeks, they begin much later than the current stage
*Sexual differentiation has begun, but fetal movement has not started*
- **Sexual differentiation** of the gonads begins around week 7 post-fertilization (week 9 gestational age)
- External genitalia differentiation occurs even later (weeks 9-12 post-fertilization)
- This stage is **far too advanced** for the current 3-week post-fertilization timeframe
*Implantation has occurred, but notochord has not yet formed*
- **Implantation** occurs 6-12 days after fertilization, which is approximately 2-3 weeks before a positive pregnancy test
- The **notochord** forms during gastrulation in the **3rd week post-fertilization** (5th week gestational age)
- By the time of this positive pregnancy test (5 weeks gestational age), the notochord has **already formed**, making this statement incorrect
Implantation physiology US Medical PG Question 6: A 27-year-old woman with a past medical history of rheumatoid arthritis and severe anemia of chronic disease presents to the emergency department for nausea, vomiting, and abdominal pain that started this morning. She has been unable to tolerate oral intake during this time. Her blood pressure is 107/58 mmHg, pulse is 127/min, respirations are 15/min, and oxygen saturation is 99% on room air. Physical exam is notable for left lower quadrant abdominal pain upon palpation. A urine pregnancy test is positive, and a serum beta-hCG is 1,110 mIU/mL. A transvaginal ultrasound demonstrates no free fluid and is unable to identify an intrauterine pregnancy. The patient states that she intends to have children in the future. Which of the following is the best next step in management?
- A. Repeat beta-hCG in 2 days (Correct Answer)
- B. CT scan of the abdomen
- C. Methotrexate
- D. Salpingostomy
- E. Salpingectomy
Implantation physiology Explanation: ***Repeat beta-hCG in 2 days***
- With a beta-hCG level of **1,110 mIU/mL** and no intrauterine pregnancy seen on ultrasound, a **repeat beta-hCG in 48 hours** is the most appropriate next step to assess the trend and differentiate between an early, viable intrauterine pregnancy, a non-viable pregnancy (miscarriage), or an ectopic pregnancy.
- The patient is currently **hemodynamically stable**, which allows for expectant management and further diagnostic evaluation rather than immediate intervention.
*CT scan of the abdomen*
- A CT scan of the abdomen exposes the patient to **ionizing radiation**, which is generally avoided in pregnancy unless absolutely necessary.
- It would not provide the specific diagnostic information needed to evaluate for an **ectopic pregnancy** as effectively as serial beta-hCG levels and repeat ultrasound.
*Methotrexate*
- **Methotrexate** is a potential treatment for ectopic pregnancy, but it is not the first step in diagnosis and would only be considered after a definitive diagnosis.
- The patient's **hemodynamic stability** and desire for future fertility make a conservative approach involving more diagnostic steps preferable before initiating medical treatment.
*Salpingostomy*
- **Salpingostomy** is a surgical procedure to remove an ectopic pregnancy while preserving the fallopian tube, but it is a definitive treatment and not a diagnostic step.
- It would be considered for a **confirmed ectopic pregnancy** in a stable patient who desires future fertility, but only after further diagnostic evaluation.
*Salpingectomy*
- **Salpingectomy**, the surgical removal of the fallopian tube, is a treatment for ectopic pregnancy, most often reserved for cases of **rupture**, significant tubal damage, or patients who do not desire future fertility from that tube.
- This patient is **hemodynamically stable** and desires future fertility, making salpingectomy an inappropriate initial choice.
Implantation physiology US Medical PG Question 7: Which of the following cells in the body depends on dynein for its unique functioning?
- A. Small intestinal mucosal cell
- B. Skeletal muscle cell
- C. Adipocyte
- D. Lower esophageal mucosal cell
- E. Fallopian tube mucosal cell (Correct Answer)
Implantation physiology Explanation: ***Fallopian tube mucosal cell***
- Dynein is a **motor protein** that facilitates the movement of **cilia** along microtubules.
- The ciliary action in fallopian tube mucosal cells is crucial for **transporting the ovum** from the ovary to the uterus.
*Small intestinal mucosal cell*
- These cells primarily depend on **microvilli** for absorption, which are actin-based structures and do not directly involve dynein for their primary function of absorption.
- While they have some cilia, their unique and defining function is nutrient absorption, not movement dependent on dynein.
*Skeletal muscle cell*
- Skeletal muscle cells rely on the interaction of **actin and myosin** filaments for **contraction**.
- Dynein is not directly involved in the mechanism of muscle contraction.
*Adipocyte*
- Adipocytes are specialized in **lipid storage** and release, a process that does not involve dynein.
- Their unique function does not depend on intracellular or extracellular movement facilitated by dynein.
*Lower esophageal mucosal cell*
- These cells primarily provide a **protective barrier** against gastric acid reflux.
- Their function involves **stratified squamous epithelium** and mucus production, not ciliary movement dependent on dynein.
Implantation physiology US Medical PG Question 8: A 12-year-old girl is brought to the emergency department 3 hours after the sudden onset of colicky abdominal pain and vomiting. She also has redness and swelling of the face and lips without pruritus. Her symptoms began following a tooth extraction earlier this morning. She had a similar episode of facial swelling after a bicycle accident 1 year ago which resolved within 48 hours without treatment. Vital signs are within normal limits. Examination shows a nontender facial edema, erythema of the oral mucosa, and an enlarged tongue. The abdomen is soft and there is tenderness to palpation over the lower quadrants. An abdominal ultrasound shows segmental thickening of the intestinal wall. Which of the following is the most likely cause of this patient's condition?
- A. T-cell mediated immune reaction
- B. Drug-induced bradykinin excess
- C. Leukotriene overproduction
- D. Immune-complex deposition
- E. Complement inhibitor deficiency (Correct Answer)
Implantation physiology Explanation: ***Complement inhibitor deficiency***
- This patient's presentation with recurrent episodes of **angioedema** (face and lip swelling, enlarged tongue, intestinal wall thickening causing abdominal pain), particularly triggered by **trauma** (tooth extraction, bicycle accident), strongly suggests **hereditary angioedema (HAE)**. HAE is caused by a deficiency or dysfunction of **C1 esterase inhibitor**, a key complement inhibitor.
- A deficiency in C1 esterase inhibitor leads to uncontrolled activation of both the **complement cascade** and the **kallikrein-bradykinin pathway**, resulting in excessive **bradykinin production**, which causes increased vascular permeability and localized edema without urticaria or pruritus.
*T-cell mediated immune reaction*
- **T-cell mediated reactions** are typically associated with **delayed-type hypersensitivity reactions** (e.g., contact dermatitis, graft rejection) and **autoimmune disorders**, which do not fit the acute, recurrent, non-pruritic angioedema seen here.
- These reactions primarily involve cell-mediated cytotoxicity or cytokine release, rather than rapid fluid extravasation due to bradykinin excess.
*Drug-induced bradykinin excess*
- While drug-induced angioedema (e.g., from **ACE inhibitors**) can also cause bradykinin excess, this patient's history of episodes since childhood (after a bicycle accident) and the current exacerbation after a tooth extraction, makes a **hereditary predisposition** much more likely than an isolated drug reaction in a 12-year-old.
- The triggers (trauma, dental procedure) are classic for HAE, which involves an intrinsic defect in bradykinin regulation, not merely an external pharmaceutical cause.
*Leukotriene overproduction*
- **Leukotrienes** are potent mediators involved in **allergic reactions** and **asthma**, contributing to bronchoconstriction, vascular permeability, and inflammation.
- Conditions involving leukotriene overproduction, such as aspirin-exacerbated respiratory disease, typically present with bronchospasm, rhinitis, or urticaria, which are not the primary features here.
*Immune-complex deposition*
- **Immune-complex deposition** is characteristic of conditions like **serum sickness**, **lupus nephritis**, or **vasculitis**, leading to inflammation, fever, rash, and organ damage.
- These conditions do not typically present with isolated, recurrent, non-pruritic angioedema and do not involve the specific mechanism of bradykinin overproduction seen in this patient.
Implantation physiology US Medical PG Question 9: A 27-year-old woman with Kallmann syndrome (congenital GnRH deficiency) desires pregnancy. She has been on estrogen-progesterone replacement for bone health. Her physician plans to switch her to pulsatile GnRH therapy. After 6 weeks of treatment, labs show: LH 4 mIU/mL, FSH 5 mIU/mL, estradiol 120 pg/mL. Ultrasound shows a 16mm dominant follicle. Evaluate and synthesize the physiologic response to determine the appropriate next intervention for ovulation induction.
- A. Continue current GnRH dosing and monitor for spontaneous LH surge
- B. Add clomiphene citrate to augment endogenous gonadotropin release
- C. Increase GnRH pulse frequency to stimulate endogenous LH surge
- D. Administer exogenous hCG to trigger ovulation and time intercourse (Correct Answer)
- E. Switch to gonadotropin therapy with recombinant FSH and LH
Implantation physiology Explanation: ***Administer exogenous hCG to trigger ovulation and time intercourse***
- In **Kallmann syndrome**, the absence of **GnRH neurons** means the patient cannot generate a spontaneous **LH surge** despite follicular maturation; **exogenous hCG** acts as an **LH analog** to trigger ovulation.
- The labs and ultrasound demonstrate successful **follicular development** with a **16mm follicle** and adequate **estradiol**, indicating the patient is ready for the final maturation trigger.
*Continue current GnRH dosing and monitor for spontaneous LH surge*
- A spontaneous surge will not occur because the patient lacks the endogenous **hypothalamic GnRH** release mechanism required to respond to **estrogen positive feedback**.
- Relying on the pump's fixed frequency will not mimic the necessary mid-cycle **GnRH surge** needed for natural ovulation.
*Add clomiphene citrate to augment endogenous gonadotropin release*
- **Clomiphene citrate** works by blocking **estrogen receptors** in the hypothalamus to increase GnRH; it is ineffective in Kallmann syndrome due to the lack of **functional GnRH neurons**.
- Therapeutic success in these patients requires bypassing the hypothalamus using either **pulsatile GnRH** or direct **gonadotropin therapy**.
*Increase GnRH pulse frequency to stimulate endogenous LH surge*
- Increasing pulse frequency does not replicate the complex **positive feedback** kinetics required to generate a massive **LH surge** in GnRH-deficient individuals.
- Fixed-frequency pulsatile pumps are designed for **folliculogenesis** but are generally insufficient to achieve the threshold required for **oocyte release** without additional triggers.
*Switch to gonadotropin therapy with recombinant FSH and LH*
- This switch is unnecessary because the patient is already showing an excellent physiologic response to **pulsatile GnRH therapy**, as evidenced by her **FSH**, **LH**, and **dominant follicle**.
- Pulsatile GnRH is often preferred when available because it maintains the **pituitary-ovarian axis** and carries a lower risk of **ovarian hyperstimulation syndrome (OHSS)** compared to exogenous gonadotropins.
Implantation physiology US Medical PG Question 10: A 30-year-old woman at 28 weeks gestation with gestational diabetes managed with insulin presents with decreased fetal movement. Fetal monitoring shows category II tracing. Umbilical artery Doppler shows absent end-diastolic flow. Her glucose control has been suboptimal (HbA1c 7.8%). Maternal blood pressure is normal. Synthesize the pathophysiologic relationship between her metabolic condition and the Doppler findings to determine the primary mechanism.
- A. Maternal hyperglycemia causing fetal hyperinsulinemia and increased oxygen consumption
- B. Maternal ketoacidosis causing direct fetal myocardial depression
- C. Fetal polycythemia from chronic hypoxia increasing blood viscosity
- D. Uteroplacental insufficiency from diabetes-induced vasculopathy affecting spiral arteries (Correct Answer)
- E. Placental hypertrophy from fetal macrosomia compressing umbilical cord
Implantation physiology Explanation: ***Uteroplacental insufficiency from diabetes-induced vasculopathy affecting spiral arteries***
- **Absent end-diastolic flow (AEDF)** in the umbilical artery signifies high **placental vascular resistance**, often due to maternal **decidual vasculopathy** and endothelial damage.
- Suboptimal glucose control in diabetes leads to **microvascular changes** in the **spiral arteries**, reducing oxygen and nutrient delivery, which results in placental insufficiency and compromised fetal wellbeing.
*Maternal hyperglycemia causing fetal hyperinsulinemia and increased oxygen consumption*
- While **maternal hyperglycemia** leads to **fetal hyperinsulinemia**, this metabolic state primarily drives **fetal macrosomia** and elective oxygen demand rather than structural vascular resistance in the umbilical artery.
- Increased oxygen consumption contributes to **fetal hypoxemia**, but it does not mechanistically explain the **AEDF** seen on Doppler studies.
*Fetal polycythemia from chronic hypoxia increasing blood viscosity*
- **Fetal polycythemia** is a compensatory response to **chronic hypoxia** triggered by erythropoietin release; it is a consequence rather than the primary driver of umbilical artery flow obstruction.
- Although increased **blood viscosity** can affect flow, the primary lesion in **AEDF** is high resistance within the **placental villous bed** due to vascular pathology.
*Maternal ketoacidosis causing direct fetal myocardial depression*
- **Maternal ketoacidosis** is an acute, life-threatening emergency that can cause **fetal distress**, but there is no clinical evidence (such as pH or anion gap) provided to support this diagnosis here.
- **AEDF** is typically a marker of chronic **placental resistance** over time, whereas myocardial depression would more likely reflect as **fetal bradycardia** or loss of variability.
*Placental hypertrophy from fetal macrosomia compressing umbilical cord*
- **Placental hypertrophy** is commonly associated with **gestational diabetes**, but the placenta does not compress the umbilical cord to the point of causing **AEDF**.
- **Umbilical cord compression** usually presents as **variable decelerations** on fetal heart monitoring, not a persistent high-resistance Doppler pattern in the umbilical artery.
More Implantation physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.