Hypothalamic-pituitary-gonadal axis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypothalamic-pituitary-gonadal axis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 1: A 16-year-old girl is brought to the physician because she has not yet had her 1st period. She was born at 39 weeks gestation via spontaneous vaginal delivery. She is up to date on all vaccines and meeting all developmental milestones. She has no history of a serious illness and takes no medications. Physical examination shows underdeveloped breasts with scant pubic and axillary hair. Speculum examination shows a short vagina and no cervix. The remainder of the physical examination shows no abnormalities. Pelvic ultrasound shows no uterus. Which of the following is the most likely karyotype in this patient?
- A. 47,XXY
- B. 45,X
- C. 46,XY (Correct Answer)
- D. 46,XX/46,XY
- E. 46,XX
Hypothalamic-pituitary-gonadal axis Explanation: ***46,XY***
- This karyotype describes an individual who is genetically male but presents phenotypically as female, often seen in **androgen insensitivity syndrome (AIS)**.
- The patient's underdeveloped breasts, scant pubic/axillary hair, short vagina with no cervix, and absent uterus (on ultrasound) are classic signs of AIS, where **testosterone is produced but tissues are unresponsive** due to receptor defects, leading to female external genitalia development and lack of Müllerian structures.
*47,XXY*
- This karyotype is associated with **Klinefelter syndrome**, which affects males and typically presents with tall stature, small testes, gynecomastia, and infertility.
- It does not explain the absence of a uterus or Mullerian structures, nor the specific presentation of underdeveloped secondary sexual characteristics in a phenotypic female.
*45,X*
- This karyotype describes **Turner syndrome**, which presents with primary amenorrhea, short stature, webbed neck, and **streak gonads** (absent or non-functional ovaries).
- While it causes primary amenorrhea and underdeveloped secondary sexual characteristics, Turner syndrome patients typically have a **uterus** (though small) and do not have an absent cervix or a short vagina in the way described.
*46,XX/46,XY*
- This represents **gonadal mosaicism**, where an individual has cell lines with both male and female karyotypes.
- The clinical presentation can be highly variable, ranging from ambiguous genitalia to female or male phenotypes, but it does not specifically account for the precise combination of primary amenorrhea, absent uterus, and underdeveloped secondary sexual characteristics as seen in AIS.
*46,XX*
- This is the normal female karyotype. While it can be associated with primary amenorrhea in conditions such as **Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome** (agenesis of the uterus and upper vagina), it would be accompanied by normal breast and pubic/axillary hair development due to functional ovaries.
- The patient's underdeveloped breasts and scant pubic/axillary hair suggest a problem with androgen action, not simply Müllerian agenesis in an otherwise hormonally normal female.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 2: A 47-year-old woman comes to the physician because of fatigue, difficulty falling asleep, and night sweats for the past 6 months. Over the past year, her menstrual cycle has become irregular and her last menstrual period was 2 months ago. She quit smoking 2 years ago. Pelvic exam shows vulvovaginal atrophy. A pregnancy test is negative. Which of the following changes is most likely to occur in this patient's condition?
- A. Decreased gonadotropin-releasing hormone
- B. Increased inhibin B
- C. Decreased luteinizing hormone
- D. Increased estrogen
- E. Increased follicle-stimulating hormone (Correct Answer)
Hypothalamic-pituitary-gonadal axis Explanation: ***Increased follicle-stimulating hormone***
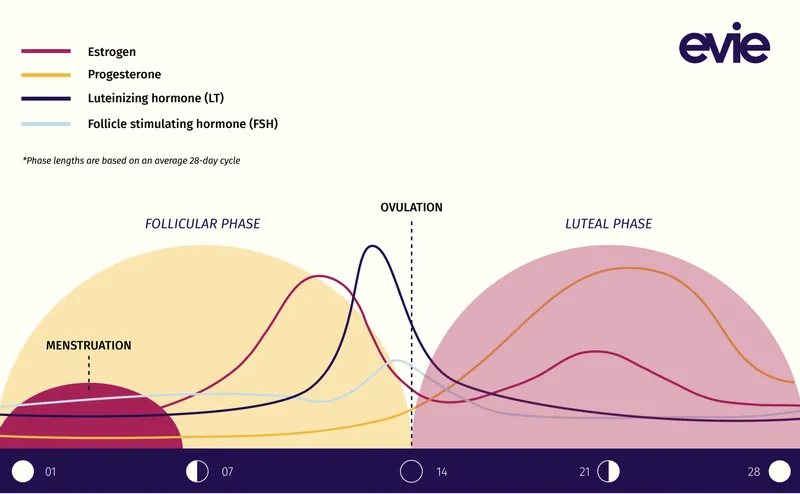
- The patient's symptoms (fatigue, insomnia, night sweats, irregular menses, 2 months amenorrhea, vulvovaginal atrophy) at age 47 are classic for **menopause**.
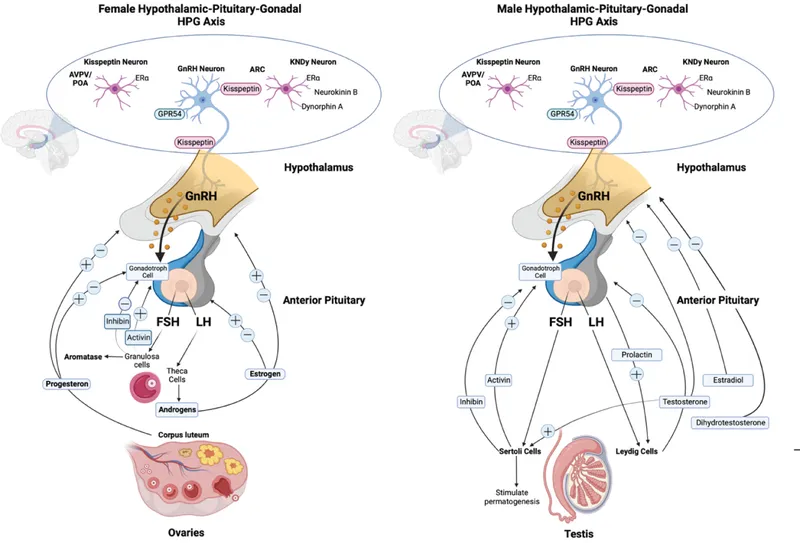
- During menopause, declining **ovarian function** leads to decreased estrogen and inhibin, which in turn causes the pituitary to release more **FSH** and LH via a feedback loop.
*Decreased gonadotropin-releasing hormone*
- **GnRH** levels are typically increased in menopause due to the lack of negative feedback from ovarian hormones, stimulating the pituitary.
- A decrease in GnRH would reduce pituitary gonadotropin secretion, which is contrary to what is observed in menopause.
*Increased inhibin B*
- **Inhibin B** is produced by ovarian granulosa cells and typically **decreases** significantly during the menopausal transition due to the reduced number of ovarian follicles.
- Decreased inhibin B contributes to the rise in FSH levels during menopause.
*Decreased luteinizing hormone*
- In menopause, both **LH** and FSH levels are **elevated** due to the loss of negative feedback from declining ovarian hormones like estrogen and inhibin.
- While FSH rises earlier and more dramatically, LH also increases.
*Increased estrogen*
- In menopause, the ovaries produce **significantly less estrogen**, leading to the classic symptoms like hot flashes and vaginal atrophy.
- The decline in estrogen is a primary hormonal change driving the menopausal transition.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 3: A 15-year-old boy is brought to the physician for a well-child visit. His parents are concerned that he has not had his growth spurt yet. As a child, he was consistently in the 60th percentile for height; now he is in the 25th percentile. His classmates make fun of his height and high-pitched voice. His parents are also concerned that he does not maintain good hygiene. He frequently forgets to shower and does not seem aware of his body odor. As an infant, he had bilateral orchidopexy for cryptorchidism and a cleft palate repair. He is otherwise healthy. Vital signs are within normal limits. On physical exam, axillary and pubic hair is sparse. Genitals are Tanner stage 1 and the testicles are 2 mL bilaterally. Which of the following is the most likely diagnosis?
- A. Constitutional delay of puberty
- B. Hyperprolactinemia
- C. Hypothyroidism
- D. Primary hypogonadism
- E. Kallmann syndrome (Correct Answer)
Hypothalamic-pituitary-gonadal axis Explanation: ***Kallmann syndrome***
- This patient's presentation with **anosmia/hyposmia** (implied by poor hygiene and lack of awareness of body odor), **delayed puberty** (Tanner stage 1 at 15 years old, small testicular volume), and a history of **cryptorchidism** and **cleft palate** is highly suggestive of Kallmann syndrome.
- Kallmann syndrome is a form of **congenital hypogonadotropic hypogonadism** characterized by a deficiency in **GnRH** migration and function, leading to impaired sexual development and a lack of olfactory bulb development.
*Constitutional delay of puberty*
- While constitutional delay also presents with delayed puberty, it typically does **not include associated congenital anomalies** like cryptorchidism or cleft palate, nor does it present with features suggestive of anosmia.
- Children with constitutional delay often have a family history of delayed puberty, and their **growth deceleration** is usually less pronounced and still follows a growth curve.
*Hyperprolactinemia*
- **Hyperprolactinemia** causes hypogonadism by inhibiting GnRH, leading to delayed puberty, but it is not associated with **anosmia**, **cryptorchidism**, or **cleft palate**.
- It would typically be investigated if central nervous system symptoms like **headaches** or **visual field defects** were present, or in the context of certain medications.
*Hypothyroidism*
- **Hypothyroidism** can cause delayed puberty and growth deceleration, but it is not associated with **anosmia**, **cryptorchidism**, or **cleft palate**.
- Other classic symptoms of hypothyroidism, such as **fatigue, weight gain, cold intolerance, and constipation**, are not mentioned.
*Primary hypogonadism*
- **Primary hypogonadism** (e.g., Klinefelter syndrome) would present with elevated gonadotropins (LH and FSH) due to testicular failure, unlike the hypogonadotropic hypogonadism seen in Kallmann syndrome.
- While cryptorchidism can lead to primary hypogonadism, the additional features of **anosmia/hyposmia** and **cleft palate** point specifically to Kallmann syndrome.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 4: A 52-year-old G3P3 presents to her gynecologist complaining of painful intercourse. She reports a 6-month history of intermittent dryness, itching, and burning during intercourse. Upon further questioning, she also reports poor sleep and occasional periods during which she feels very warm and sweats profusely. Her past medical history is significant for poorly controlled hypertension and a 10 pack-year smoking history. She takes hydrochlorothiazide and enalapril. Her temperature is 99.3°F (37.4°C), blood pressure is 135/85 mmHg, pulse is 90/min, and respirations are 18/min. On examination, she is a healthy female in no distress. Pelvic examination reveals no adnexal or cervical motion tenderness. Which of the following sets of hormone levels are most likely to be found in this patient?
- A. Increased estrogen, decreased FSH, decreased LH, decreased GnRH
- B. Decreased estrogen, decreased FSH, decreased LH, increased GnRH
- C. Normal estrogen, normal FSH, normal LH, normal GnRH
- D. Decreased estrogen, increased FSH, increased LH, increased GnRH (Correct Answer)
- E. Increased estrogen, increased FSH, increased LH, increased GnRH
Hypothalamic-pituitary-gonadal axis Explanation: ***Decreased estrogen, increased FSH, increased LH, increased GnRH***
- The patient's symptoms of **vaginal dryness**, **dyspareunia**, **hot flashes**, and **night sweats** are classic for **menopause**. These symptoms are caused by a significant decline in **estrogen production** by the ovaries.
- In response to low estrogen, the **hypothalamus** increases **GnRH** (gonadotropin-releasing hormone) secretion, which in turn leads to increased production of **FSH** (follicle-stimulating hormone) and **LH** (luteinizing hormone) from the **anterior pituitary** in an attempt to stimulate ovarian function.
*Increased estrogen, decreased FSH, decreased LH, decreased GnRH*
- This hormonal profile is characteristic of conditions like **ovarian tumors** that produce estrogen or **pregnancy**, neither of which fits the clinical picture of menopause.
- High estrogen levels would typically **inhibit GnRH, FSH, and LH** secretion through negative feedback mechanisms.
*Decreased estrogen, decreased FSH, decreased LH, increased GnRH*
- This pattern suggests a **primary ovarian failure** (low estrogen) coupled with a **pituitary or hypothalamic dysfunction** resulting in inappropriately low FSH and LH. This is not typical for natural menopause.
- In natural menopause, the pituitary and hypothalamus respond to low estrogen by **increasing** FSH and LH.
*Normal estrogen, normal FSH, normal LH, normal GnRH*
- This hormonal profile would be consistent with a **pre-menopausal** or **reproductive-aged woman**, not someone experiencing menopausal symptoms like this patient.
- The patient's symptoms clearly indicate a significant shift in her hormonal status.
*Increased estrogen, increased FSH, increased LH, increased GnRH*
- It is physiologically unlikely to have **increased estrogen** simultaneously with **increased FSH, LH, and GnRH**, as estrogen exerts negative feedback on these hormones.
- This pattern does not align with any known normal or common pathological hormonal state.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 5: A 24-year-old woman comes to her primary care physician because she has not had a menstrual period for 6 months. She is a competitive runner and has been training heavily for the past year in preparation for upcoming races. She has no family or personal history of serious illness. She has not been sexually active for the past 9 months. Her temperature is 36.9°C (98.4° F), pulse is 51/min, respirations are 12/min, and blood pressure is 106/67 mm Hg. Her BMI is 18.1 kg/m2. Which of the following is the most likely cause of her amenorrhea?
- A. Decreased frequency of GnRH release from the hypothalamus (Correct Answer)
- B. Poor synthetic response of ovarian cells to circulating LH and FSH
- C. Increased prolactin secretion
- D. Intrauterine adhesions
- E. Increased LH release and increased ovarian androgen production
Hypothalamic-pituitary-gonadal axis Explanation: ***Decreased frequency of GnRH release from the hypothalamus***
- This patient's profile (competitive runner, regular intense training, low **BMI** of 18.1 kg/m2, amenorrhea, and mild bradycardia) is classic for **hypothalamic amenorrhea**.
- **Intense physical activity** and **low body fat** can disrupt the pulsatile release of **gonadotropin-releasing hormone (GnRH)** from the hypothalamus, leading to reduced LH and FSH secretion and subsequent ovarian dysfunction.
*Poor synthetic response of ovarian cells to circulating LH and FSH*
- This scenario would suggest **primary ovarian insufficiency** or **premature ovarian failure**, which is less likely in a young, otherwise healthy athlete with no family history.
- While LH and FSH levels might be low in this patient due to hypothalamic suppression, the *ovaries themselves* are typically capable of responding if stimulated appropriately.
*Increased prolactin secretion*
- **Hyperprolactinemia** causes amenorrhea, but it would typically present with **galactorrhea** and is not directly linked to strenuous exercise or low BMI in this manner.
- While prolactin can suppress GnRH, the primary etiology in this athletic patient is more directly related to energy balance.
*Intrauterine adhesions*
- **Intrauterine adhesions (Asherman's syndrome)** typically occur after uterine trauma, such as D&C procedures, infection, or surgery.
- This patient has no history to suggest such an event, and her amenorrhea is more consistent with a hormonal imbalance.
*Increased LH release and increased ovarian androgen production*
- This describes **polycystic ovary syndrome (PCOS)**, which is characterized by obesity, hirsutism, and insulin resistance, none of which are present in this patient.
- In PCOS, there is often an increased LH:FSH ratio, leading to increased ovarian androgen production, which is the opposite of what would be expected with hypothalamic amenorrhea.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 6: A 23-year-old woman comes to the emergency department because of a 5-day history of nausea and vomiting. There is no associated fever, abdominal pain, constipation, diarrhea, or dysuria. She is sexually active and uses condoms inconsistently. Her last menstrual period was 10 weeks ago. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 18/min, and blood pressure is 110/70 mm Hg. There is no rebound tenderness or guarding. A urine pregnancy test is positive. Ultrasonography shows an intrauterine pregnancy consistent in size with an 8-week gestation. The hormone that was measured in this patient's urine to detect the pregnancy is also directly responsible for which of the following processes?
- A. Hypertrophy of the uterine myometrium
- B. Fetal angiogenesis
- C. Maintenance of the corpus luteum (Correct Answer)
- D. Inhibition of ovulation
- E. Stimulation of uterine contractions at term
Hypothalamic-pituitary-gonadal axis Explanation: ***Maintenance of the corpus luteum***
- The hormone measured in the urine pregnancy test is **human chorionic gonadotropin (hCG)**. hCG's primary role early in pregnancy is to **maintain the corpus luteum**, which in turn produces progesterone to support the uterine lining.
- The **corpus luteum** is essential for progesterone production until the placenta is sufficiently developed to take over this function, typically around 8-10 weeks gestation.
*Hypertrophy of the uterine myometrium*
- **Estrogen** and **progesterone** are primarily responsible for the hypertrophy and hyperplasia of the uterine myometrium during pregnancy.
- While hCG indirectly supports this by maintaining the corpus luteum (which produces estrogen and progesterone), it does not directly cause myometrial hypertrophy itself.
*Fetal angiogenesis*
- **Vascular endothelial growth factor (VEGF)** and **fibroblast growth factor (FGF)** are key factors directly involved in fetal angiogenesis (the formation of new blood vessels in the fetus).
- While proper placental function, supported by hCG, is critical for fetal growth, hCG itself is not the direct mediator of fetal angiogenesis.
*Inhibition of ovulation*
- High levels of **estrogen** and **progesterone** (produced by the corpus luteum, maintained by hCG) provide **negative feedback** to the hypothalamus and pituitary, thus inhibiting the release of GnRH, FSH, and LH, which prevents further ovulation.
- hCG itself does not directly inhibit ovulation; rather, it sets in motion the hormonal cascade that leads to its inhibition.
*Stimulation of uterine contractions at term*
- **Oxytocin** is the primary hormone responsible for stimulating uterine contractions, particularly at term, often in conjunction with prostaglandins.
- hCG levels peak early in pregnancy and then decline, and it plays no direct role in stimulating labor contractions.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 7: A 27-year-old woman comes to the physician for the evaluation of infertility. She has been unable to conceive for the past 2 years. Menses occur at 45 to 80-day intervals. She is 168 cm (5 ft 6 in) tall and weighs 77 kg (170 lb); BMI is 27.4 kg/m2. Physical examination shows facial acne and pigmented hair on the upper lip. Serum studies show elevated levels of testosterone and an LH:FSH ratio of 4:1. Treatment with the appropriate drug for this patient's infertility is begun. Which of the following is the primary mechanism of action of this drug?
- A. Activation of pituitary dopamine receptors
- B. Activation of granulosa cell aromatase
- C. Activation of ovarian luteinizing hormone receptors
- D. Inhibition of hypothalamic estrogen receptors (Correct Answer)
- E. Inhibition of endometrial progesterone receptors
Hypothalamic-pituitary-gonadal axis Explanation: ***Inhibition of hypothalamic estrogen receptors***
- The patient presents with classic symptoms of **polycystic ovarian syndrome (PCOS)**, including **oligomenorrhea** (menses every 45-80 days), **hirsutism**, **acne**, **elevated BMI**, **elevated testosterone**, and an **elevated LH:FSH ratio (4:1)**.
- **Clomiphene citrate** is the first-line drug for ovulation induction in PCOS patients with infertility.
- Clomiphene is a **selective estrogen receptor modulator (SERM)** that acts as a **competitive antagonist at estrogen receptors in the hypothalamus**.
- By blocking estrogen receptors, clomiphene prevents normal **negative feedback inhibition** of GnRH release.
- This results in increased **GnRH pulsatility**, leading to increased **FSH and LH secretion** from the anterior pituitary, which promotes **follicular development and ovulation**.
*Activation of pituitary dopamine receptors*
- This mechanism is characteristic of **dopamine agonists** (e.g., **bromocriptine**, **cabergoline**), which are used to treat infertility due to **hyperprolactinemia**.
- These agents activate D2 receptors in lactotroph cells, inhibiting prolactin secretion.
- The patient shows no signs of hyperprolactinemia (e.g., galactorrhea, amenorrhea from elevated prolactin).
*Activation of granulosa cell aromatase*
- Aromatase converts androgens to estrogens in granulosa cells.
- While aromatase activity is important in follicular development, **activating aromatase is not a mechanism of any standard ovulation-inducing drug**.
- In PCOS, there is often relative aromatase insufficiency, but drugs do not directly activate this enzyme for fertility treatment.
*Activation of ovarian luteinizing hormone receptors*
- While **exogenous LH or hCG** (which acts on LH receptors) may be used in assisted reproductive technology, this is not the mechanism of **first-line ovulation induction** in PCOS.
- Clomiphene works by increasing endogenous LH/FSH release, not by directly activating ovarian receptors.
*Inhibition of endometrial progesterone receptors*
- This is the mechanism of **mifepristone** (RU-486), an antiprogestin used for medical abortion and occasionally for **endometriosis** or **uterine fibroids**.
- Inhibiting progesterone receptors would **prevent implantation** or disrupt pregnancy, which is opposite to the goal of fertility treatment.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 8: An 8-year-old boy is brought to the hospital because of blurred vision and headache for 3 months. During this period, the father has noticed that the child has been tilting his head back to look straight ahead. The patient has also had difficulty falling asleep for 2 months. He has had a 3.5 kg (7.7 lb) weight loss over the past 6 months. His temperature is 37.7°C (99.8°F), pulse is 105/min, and blood pressure is 104/62 mm Hg. Examination shows equal pupils that are not reactive to light. The pupils constrict when an object is brought near the eye. His upward gaze is impaired; there is nystagmus and eyelid retraction while attempting to look upwards. Neurologic examination shows no other focal findings. Which of the following is the most likely sequela of this patient's condition?
- A. Diabetes insipidus
- B. Blindness
- C. Subarachnoid hemorrhage
- D. Diabetic ketoacidosis
- E. Precocious puberty (Correct Answer)
Hypothalamic-pituitary-gonadal axis Explanation: ***Precocious puberty***
- The constellation of **Parinaud syndrome** (impaired upward gaze, nystagmus, eyelid retraction, and pupillary abnormalities) combined with symptoms of **increased intracranial pressure** (headache, blurred vision, weight loss, difficulty sleeping) in a child points to a **pineal tumor**, specifically a **germinoma**.
- Pineal germinomas are known to secrete **human chorionic gonadotropin (hCG)**, which can cross-react with LH receptors, leading to stimulation of **testosterone production** and subsequent **precocious puberty** in boys.
*Diabetes insipidus*
- While diabetes insipidus can be associated with suprasellar tumors, it's less commonly a direct sequela of a **pineal germinoma** itself compared to precocious puberty, although mass effect on the hypothalamus could potentially lead to it.
- The primary symptoms described are classic for **Parinaud syndrome** and increased intracranial pressure, not specific signs of diabetes insipidus (e.g., polyuria, polydipsia).
*Blindness*
- **Vision loss or blindness** can occur due to long-standing **papilledema** from increased intracranial pressure, or direct compression of the **optic chiasm** or **optic nerves** by a large tumor.
- While a possible serious complication, **precocious puberty** is a more specific and direct endocrinological sequela linked to the hormonal activity of a pineal germinoma in boys.
*Subarachnoid hemorrhage*
- Although any intracranial tumor can potentially bleed, a **subarachnoid hemorrhage** typically presents with a sudden onset of **"thunderclap" headache**, stiff neck, and altered consciousness.
- The patient's symptoms have been evolving over 3 months, which is inconsistent with the acute presentation of a subarachnoid hemorrhage.
*Diabetic ketoacidosis*
- **Diabetic ketoacidosis (DKA)** is a severe complication of **type 1 diabetes mellitus**, characterized by hyperglycemia, metabolic acidosis, and ketonemia.
- There are no clinical signs or symptoms in this presentation (e.g., polyuria, polydipsia, Kussmaul respirations, fruity breath) to suggest uncontrolled diabetes or DKA, and it is not a direct sequela of a pineal tumor.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 9: A 33-year-old man comes to the physician with his wife for evaluation of infertility. They have been unable to conceive for 2 years. The man reports normal libido and erectile function. He has smoked one pack of cigarettes daily for 13 years. He does not take any medications. He has a history of right-sided cryptorchidism that was surgically corrected when he was 7 years of age. Physical examination shows no abnormalities. Analysis of his semen shows a low sperm count. Laboratory studies are most likely to show which of the following?
- A. Decreased inhibin B concentration (Correct Answer)
- B. Increased prolactin concentration
- C. Increased placental ALP concentration
- D. Decreased testosterone concentration
- E. Decreased FSH concentration
Hypothalamic-pituitary-gonadal axis Explanation: ***Decreased inhibin B concentration***
- The patient's history of **corrected cryptorchidism** and current **low sperm count** suggest primary testicular failure affecting spermatogenesis.
- **Inhibin B** is produced by Sertoli cells in response to FSH and is a marker of Sertoli cell function and spermatogenesis; its decrease indicates impaired spermatogenesis.
*Increased prolactin concentration*
- **Hyperprolactinemia** can cause hypogonadism and infertility by suppressing GnRH, leading to decreased LH, FSH, and testosterone.
- However, the patient has normal libido and erectile function, which would likely be affected by hyperprolactinemia.
*Increased placental ALP concentration*
- **Placental alkaline phosphatase (ALP)** is a marker for germ cell tumors, particularly seminomas.
- While cryptorchidism increases the risk of testicular cancer, the primary issue described is infertility due to low sperm count, not a presentation suggestive of a mass.
*Decreased testosterone concentration*
- Although **primary testicular failure** (Sertoli cell dysfunction) can lead to secondary Leydig cell dysfunction over time, the patient's normal libido and erectile function make an isolated or significant decrease in testosterone less likely as the primary finding.
- Leydig cells, which produce testosterone, are often less affected than Sertoli cells in cases of isolated spermatogenic failure following cryptorchidism.
*Decreased FSH concentration*
- **Decreased FSH** would suggest a central (hypothalamic or pituitary) cause of hypogonadism, leading to secondary testicular failure.
- In primary testicular failure (as suggested by cryptorchidism history), the pituitary compensates by **increasing FSH levels** due to the loss of negative feedback from inhibin B; therefore, FSH would be elevated, not decreased, in this patient.
Hypothalamic-pituitary-gonadal axis US Medical PG Question 10: A 32-year-old female presents to her obstetrician 3 weeks postpartum for failure to lactate. Of note, she has been unable to tolerate cold environments since the birth of her child. Review of systems is positive for fatigue, lightheadedness, and a 3-pound weight gain over the last 3 weeks. Her delivery was complicated by placenta accreta with postpartum blood loss. Her newborn infant is doing well on formula. She denies any personal or family history of thyroid disease. Physical exam is overall unremarkable. On a panel of hormone testing, which of the following levels is most likely to be normal in this patient?
- A. Thyroid hormone
- B. Cortisol
- C. Luteinizing hormone
- D. Antidiuretic hormone (Correct Answer)
- E. Aldosterone
Hypothalamic-pituitary-gonadal axis Explanation: ***Antidiuretic hormone***
- This patient is presenting with symptoms consistent with **Sheehan syndrome**, which is postpartum pituitary necrosis due to severe hemorrhage and hypovolemic shock.
- Sheehan syndrome **primarily affects the anterior pituitary**, where most pituitary hormones are produced.
- **Antidiuretic hormone (ADH)** is synthesized by the **hypothalamus** and stored/released by the **posterior pituitary**, which is typically **spared** in Sheehan syndrome due to its separate blood supply.
- Therefore, **ADH levels would be normal** in this patient, making this the correct answer.
*Aldosterone*
- The **renin-angiotensin-aldosterone system (RAAS)** is regulated independently by the kidneys and is preserved in pituitary disorders.
- Aldosterone levels would also likely be **normal** in this patient.
- However, ADH is the better answer as it specifically demonstrates the anatomical distinction between anterior and posterior pituitary function.
*Thyroid hormone*
- The **anterior pituitary** fails to produce **thyroid-stimulating hormone (TSH)** in Sheehan syndrome, leading to secondary hypothyroidism.
- This results in **low thyroid hormone levels**.
- Her symptoms of **cold intolerance**, **fatigue**, and **weight gain** are classic manifestations of hypothyroidism.
*Cortisol*
- The anterior pituitary produces **adrenocorticotropic hormone (ACTH)**, which stimulates cortisol release from the adrenal glands.
- In Sheehan syndrome, failure of ACTH production leads to **secondary adrenal insufficiency** with **low cortisol levels**.
- This contributes to her **fatigue** and **lightheadedness**.
*Luteinizing hormone*
- The anterior pituitary produces **luteinizing hormone (LH)**, which is crucial for ovarian function and ovulation.
- The patient's **failure to lactate** is due to **prolactin deficiency** (another anterior pituitary hormone), not LH deficiency.
- Lack of LH and other gonadotropins would contribute to amenorrhea and loss of reproductive function that often accompany Sheehan syndrome.
More Hypothalamic-pituitary-gonadal axis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.