Water balance and osmoregulation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Water balance and osmoregulation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Water balance and osmoregulation US Medical PG Question 1: A 28-year-old woman presents to her primary care physician complaining of intense thirst and frequent urination for the past 2 weeks. She says that she constantly feels the urge to drink water and is also going to the bathroom to urinate frequently throughout the day and multiple times at night. She was most recently hospitalized 1 month prior to presentation following a motor vehicle accident in which she suffered severe impact to her head. The physician obtains laboratory tests, with the results shown below:
Serum:
Na+: 149 mEq/L
Cl-: 103 mEq/L
K+: 3.5 mEq/L
HCO3-: 24 mEq/L
BUN: 20 mg/dL
Glucose: 105 mg/dL
Urine Osm: 250 mOsm/kg
The patient’s condition is most likely caused by inadequate hormone secretion from which of the following locations?
- A. Adrenal cortex
- B. Anterior pituitary
- C. Preoptic nucleus of the hypothalamus
- D. Suprachiasmatic nucleus of the hypothalamus
- E. Posterior pituitary (Correct Answer)
Water balance and osmoregulation Explanation: ***Posterior pituitary***
- The patient's symptoms of **polydipsia** and **polyuria**, coupled with **hypernatremia** and **low urine osmolality**, are classic signs of **diabetes insipidus (DI)**.
- The **posterior pituitary gland** is responsible for releasing **antidiuretic hormone (ADH)**, which, when inadequately secreted (neurogenic DI), leads to these findings. The prior **head trauma** is a common cause of damage to this region.
*Adrenal cortex*
- The adrenal cortex produces **mineralocorticoids** (e.g., **aldosterone**), **glucocorticoids** (e.g., **cortisol**), and **androgens**.
- Deficiencies or excesses of these hormones lead to conditions like **Addison's disease** (adrenal insufficiency) or **Cushing's syndrome**, which have different clinical presentations than those described.
*Anterior pituitary*
- The anterior pituitary produces hormones such as **GH, TSH, ACTH, FSH, LH**, and **prolactin**.
- Dysfunction of the anterior pituitary would lead to a range of hormonal imbalances impacting growth, metabolism, and reproduction, but not directly cause diabetes insipidus.
*Preoptic nucleus of the hypothalamus*
- The **preoptic nucleus** is involved in **thermoregulation**, **sleep**, and **hypothalamic control** of reproduction.
- While part of the hypothalamus, its primary functions do not directly involve ADH synthesis or release, thereby not causing diabetes insipidus.
*Suprachiasmatic nucleus of the hypothalamus*
- The **suprachiasmatic nucleus (SCN)** is the body's primary **circadian rhythm** pacemaker.
- Damage to the SCN would disrupt the sleep-wake cycle and other circadian functions, but would not directly lead to symptoms of diabetes insipidus.
Water balance and osmoregulation US Medical PG Question 2: A 56-year-old man is seen in the hospital for a chief complaint of intense thirst and polyuria. His history is significant for recent transsphenoidal resection of a pituitary adenoma. With regard to the man's fluid balance, which of the following would be expected?
- A. Hyponatremia
- B. Increased extracellular fluid osmolarity (Correct Answer)
- C. Serum osmolarity <290 mOsm/L
- D. Elevated serum ADH
- E. Elevated blood glucose
Water balance and osmoregulation Explanation: ***Increased extracellular fluid osmolarity***
- The symptoms of intense thirst and polyuria after pituitary surgery are classic for **diabetes insipidus (DI)**, which results from insufficient **antidiuretic hormone (ADH)**.
- Lack of ADH leads to the kidneys' inability to reabsorb water, causing excessive water loss and a consequent **increase in plasma osmolality** and extracellular fluid osmolarity as water is lost disproportionately to solutes.
*Hyponatremia*
- **Hyponatremia** (low sodium) typically occurs from over-hydration or conditions causing excess ADH, such as **syndrome of inappropriate ADH (SIADH)**.
- In DI, the primary problem is water loss leading to **hypernatremia** (high sodium) and increased osmolarity.
*Serum osmolarity <290 mOsm/L*
- Normal serum osmolarity is approximately **275-295 mOsm/L**. A value less than 290 mOsm/L suggests **hypo-osmolarity**.
- In DI, the significant water loss due to lack of ADH leads to **increased serum osmolarity**, usually above 295 mOsm/L.
*Elevated serum ADH*
- **Elevated serum ADH** would lead to increased water reabsorption in the kidneys, resulting in concentrated urine and potentially hyponatremia.
- In central diabetes insipidus, the problem is a **deficiency of ADH** secretion or action, leading to low or undetectable ADH levels.
*Elevated blood glucose*
- **Elevated blood glucose** is characteristic of **diabetes mellitus**, where polyuria and polydipsia occur due to osmotic diuresis from high glucose levels.
- This patient's history of pituitary surgery and the specific presentation points to DI, which is a disorder of **water balance** not directly related to glucose metabolism.
Water balance and osmoregulation US Medical PG Question 3: A 30-year-old man presents to your clinic complaining of excessive thirst and frequent urination for the past few months. Urine testing reveals a low urine osmolarity, which fails to increase after subjecting the patient to a water deprivation test and injection of desmopressin. Further into the encounter, the patient reveals that he has been on a mood stabilizer for bipolar disorder for several years. Which of the following is the most likely cause of his polyuria?
- A. Nephrogenic diabetes insipidus (Correct Answer)
- B. Syndrome of inappropriate ADH secretion
- C. Primary polydipsia
- D. Central diabetes insipidus
- E. Urinary tract infection
Water balance and osmoregulation Explanation: ***Nephrogenic diabetes insipidus***
- The patient's history of **excessive thirst and frequent urination** with **low urine osmolarity** indicates a problem with water reabsorption.
- The failure of urine osmolarity to increase after both **water deprivation and desmopressin administration** strongly suggests **nephrogenic diabetes insipidus**, where the kidneys do not respond to ADH. His long-term use of a mood stabilizer (likely **lithium** for bipolar disorder) is a common cause of acquired nephrogenic DI.
*Syndrome of inappropriate ADH secretion*
- **SIADH** typically presents with **hyponatremia** and **concentrated urine** (high urine osmolarity) despite plasma hypo-osmolality, which is the opposite of this patient's findings.
- This condition leads to **fluid retention** and *not* polyuria or excessive thirst.
*Primary polydipsia*
- In primary polydipsia, excessive fluid intake leads to polyuria, but the kidneys are still able to **concentrate urine** in response to water deprivation.
- The patient's urine osmolarity would **increase** after water deprivation, unlike what is observed here.
*Central diabetes insipidus*
- While central DI also causes polyuria and low urine osmolarity, the urine osmolarity **would increase** significantly after the administration of **desmopressin** (synthetic ADH) because the kidneys are still responsive.
- The lack of response to desmopressin rules out a central cause.
*Urinary tract infection*
- A UTI would typically present with symptoms such as **dysuria, urgency, frequency** (though polyuria can occur), and often **hematuria or pyuria**.
- It would not explain the specific findings of **low urine osmolarity** and the **failure to respond to water deprivation and desmopressin** in this manner.
Water balance and osmoregulation US Medical PG Question 4: A 45-year-old woman is brought to the Emergency Department by her husband due to increasing confusion. He reports that she has been urinating a lot for the past month or so, especially at night, and has also been constantly drinking water and tea. Lately, she has been more tired than usual as well. Her past medical history is significant for bipolar disorder. She takes lithium and a multivitamin. She has a levonorgestrel IUD. Her blood pressure is 140/90 mmHg, pulse rate is 95/min, respiratory rate is 16/min, and temperature is 36°C (96.8°F). At physical examination, she is drowsy and disoriented. Her capillary refill is delayed and her mucous membranes appear dry. The rest of the exam is nondiagnostic. Laboratory studies show:
Na+: 148 mEq/L
K+: 4.2 mEq/L
Serum calcium: 11.0 mg/dL
Creatinine: 1.0 mg/dL
Urine osmolality: 190 mOsm/kg
Serum osmolality: 280 mOsm/kg
Finger-stick glucose: 120 mg/dL
Fluid resuscitation is initiated. Which of the following is the most likely diagnosis?
- A. Nephrogenic diabetes insipidus (Correct Answer)
- B. Psychogenic polydipsia
- C. Central diabetes insipidus
- D. SIADH
- E. Diabetes Mellitus
Water balance and osmoregulation Explanation: ***Nephrogenic diabetes insipidus***
- The patient's history of **lithium use**, combined with **polyuria, polydipsia**, and laboratory findings of **hypernatremia (148 mEq/L)** with **inappropriately low urine osmolality (190 mOsm/kg)** in the setting of elevated serum osmolality, is highly consistent with nephrogenic diabetes insipidus.
- In a normal kidney, hypernatremia and elevated serum osmolality should trigger ADH release and result in concentrated urine (>800 mOsm/kg), but this patient's urine remains dilute, indicating **renal resistance to ADH**.
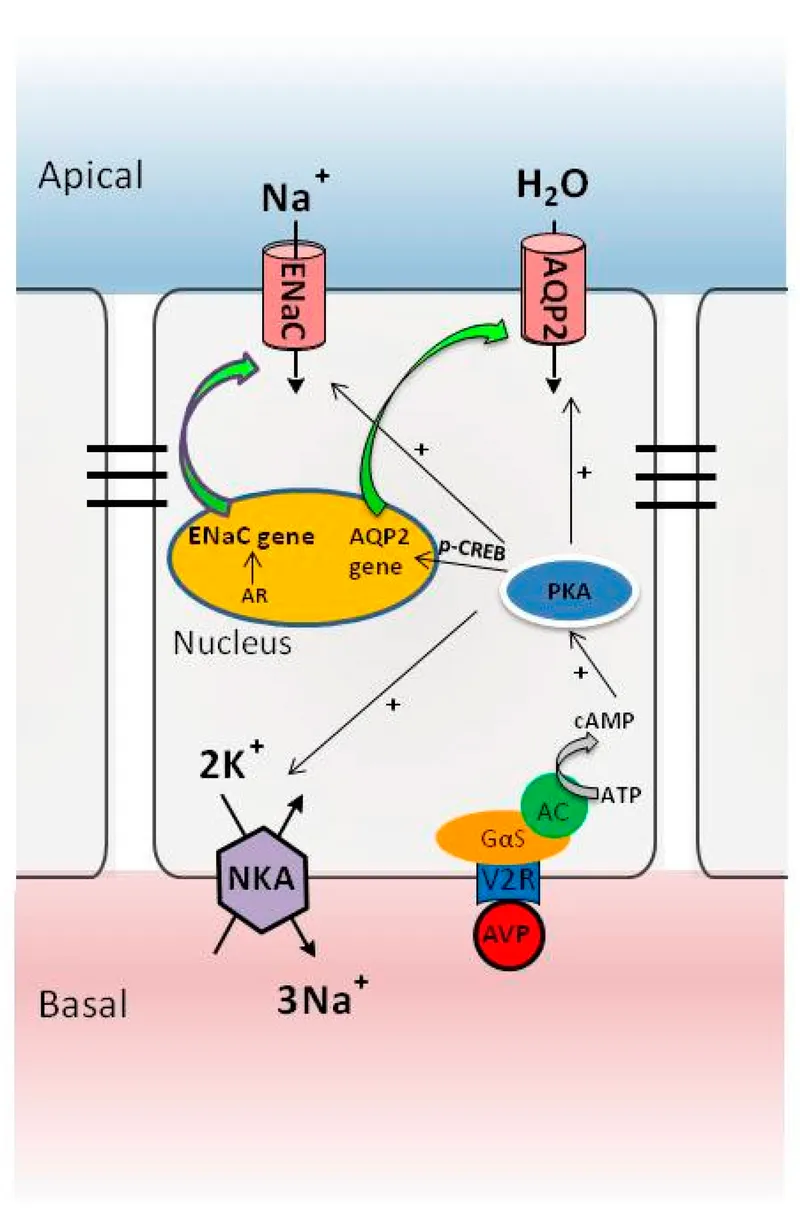
- Lithium is a well-known cause of acquired nephrogenic diabetes insipidus, as it interferes with aquaporin-2 channels and the kidney's response to **ADH (vasopressin)**.
*Psychogenic polydipsia*
- This condition involves excessive water intake, leading to **hyponatremia** due to hemodilution, which contradicts the patient's **hypernatremia**.
- In psychogenic polydipsia, urine osmolality would be appropriately low due to water overload, not due to renal resistance to ADH.
*Central diabetes insipidus*
- Central DI is caused by a deficiency in **ADH production or release**, leading to polyuria and polydipsia with high serum osmolality and low urine osmolality.
- While the laboratory pattern is similar, the patient's history of **lithium use** makes nephrogenic DI far more likely.
- Central DI would respond to desmopressin (ADH analog), whereas nephrogenic DI would not.
*SIADH*
- SIADH is characterized by **excessive ADH activity**, leading to **hyponatremia** and inappropriately concentrated urine, which is the opposite of this patient's presentation of hypernatremia and dilute urine.
- The patient's symptoms are completely inconsistent with SIADH.
*Diabetes Mellitus*
- Diabetes mellitus causes polyuria and polydipsia due to **glucosuria and osmotic diuresis**, but the patient's **finger-stick glucose (120 mg/dL)** is within the normal range.
- The elevated serum sodium and low urine osmolality are not typical features of uncontrolled diabetes mellitus, which would present with glucosuria and elevated serum glucose.
Water balance and osmoregulation US Medical PG Question 5: Activation of the renin-angiotensin-aldosterone system yields a significant physiological effect on renal blood flow and filtration. Which of the following is most likely to occur in response to increased levels of Angiotensin-II?
- A. Decreased renal plasma flow, decreased filtration fraction
- B. Decreased renal plasma flow, increased glomerular capillary oncotic pressure
- C. Increased renal plasma flow, decreased filtration fraction
- D. Increased renal plasma flow, increased filtration fraction
- E. Decreased renal plasma flow, increased filtration fraction (Correct Answer)
Water balance and osmoregulation Explanation: ***Decreased renal plasma flow, increased filtration fraction***
- **Angiotensin II** causes **efferent arteriolar constriction**, which reduces blood flow leaving the glomerulus, thereby **decreasing renal plasma flow**.
- This efferent constriction also increases **glomerular hydrostatic pressure** and reduces plasma flow distal to the glomerulus, leading to a **higher filtration fraction** (GFR/RPF).
*Decreased renal plasma flow, decreased filtration fraction*
- While **renal plasma flow decreases**, a **decreased filtration fraction** would imply that either GFR decreases disproportionately more than RPF or GFR does not increase despite the RPF reduction, which is not the typical response to **angiotensin II** due to its predominant effect on the **efferent arteriole**.
*Decreased renal plasma flow, increased glomerular capillary oncotic pressure*
- **Increased glomerular capillary oncotic pressure** is a consequence of increased filtration fraction, as more fluid is filtered out, leaving behind a more concentrated plasma. This option includes a correct element (decreased RPF) but pairs it with a less direct and defining outcome of acute Angiotensin II action as the primary physiological effect.
*Increased renal plasma flow, decreased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, predominantly of the efferent arteriole, which by definition would **decrease renal plasma flow**, not increase it.
- A **decreased filtration fraction** would be inconsistent with efferent arteriolar constriction which typically raises GFR relative to RPF.
*Increased renal plasma flow, increased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, leading to a **decrease in renal plasma flow**, not an increase.
- While **filtration fraction is increased**, the initial premise of increased renal plasma flow is incorrect.
Water balance and osmoregulation US Medical PG Question 6: A physician is choosing whether to prescribe losartan or lisinopril to treat hypertension in a 56-year-old male. Relative to losartan, one would expect treatment with lisinopril to produce which of the following changes in the circulating levels of these peptides?
- A. Aldosterone increase; bradykinin decrease
- B. Angiotensin II increase; bradykinin decrease
- C. Renin decrease; angiotensin I increase
- D. Bradykinin increase; angiotensin II decrease (Correct Answer)
- E. Renin decrease; angiotensin II increase
Water balance and osmoregulation Explanation: ***Bradykinin increase; angiotensin II decrease***
- **Lisinopril** is an **ACE inhibitor**, which directly blocks the conversion of **angiotensin I** to **angiotensin II**, leading to a decrease in circulating **angiotensin II** levels.
- ACE is also responsible for the breakdown of **bradykinin**, so inhibiting ACE with lisinopril will lead to an **increase in bradykinin** levels, contributing to vasodilation but also the characteristic cough.
*Aldosterone increase; bradykinin decrease*
- **Lisinopril** (an ACE inhibitor) decreases **angiotensin II**, which in turn leads to a **decrease in aldosterone** synthesis and release, not an increase.
- **Bradykinin** levels would increase due to ACE inhibition, as ACE is involved in its degradation.
*Angiotensin II increase; bradykinin decrease*
- **Lisinopril** directly inhibits the enzyme responsible for producing **angiotensin II**, thus leading to its **decrease**, not an increase.
- **Bradykinin** levels would increase because its degradation pathway (via ACE) is blocked, not decrease.
*Renin decrease; angiotensin I increase*
- **Lisinopril** reduces the negative feedback on **renin** release, leading to an **increase in renin** levels, not a decrease.
- While ACE is inhibited by lisinopril, this leads to an accumulation of its substrate, **angiotensin I**, resulting in an increase of angiotensin I.
*Renin decrease; angiotensin II increase*
- As an ACE inhibitor, lisinopril would lead to an **increase in renin** due to reduced negative feedback from angiotensin II, not a decrease.
- **Angiotensin II** levels would **decrease** because its production from angiotensin I is directly inhibited by lisinopril.
Water balance and osmoregulation US Medical PG Question 7: A 75-year-old gentleman is brought to the ED with confusion that started earlier this morning. His family notes that he was complaining of feeling weak last night and also had a slight tremor at the time. He is afebrile and he has no known chronic medical conditions. Physical exam reveals a cooperative but confused gentleman. His mucous membranes are moist, he has no focal neurological deficits, and his skin turgor is within normal limits. His lab results are notable for:
Serum Na+: 123 mEq/L
Plasma osmolality: 268 mOsm/kg
Urine osmolality: 349 mOsm/kg
Urine Na+: 47 mEq/L
Which of the following malignancies is most likely to be responsible for this patient's presentation?
- A. Gastric adenocarcinoma
- B. Small cell lung cancer (Correct Answer)
- C. Esophageal squamous cell carcinoma
- D. Non-seminomatous germ cell tumor
- E. Rib osteosarcoma
Water balance and osmoregulation Explanation: ***Small cell lung cancer***
- This patient's laboratory values (hyponatremia, low plasma osmolality, and inappropriately high urine osmolality with elevated urine sodium) are classic for the **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- **Small cell lung cancer** is the most common malignancy associated with paraneoplastic SIADH due to its ability to ectopically produce ADH.
*Gastric adenocarcinoma*
- While gastric adenocarcinomas can cause paraneoplastic syndromes, SIADH is an **uncommon** paraneoplastic manifestation of this type of cancer.
- Other paraneoplastic syndromes, such as **Trousseau's syndrome** (migratory thrombophlebitis), are more classically associated with gastric adenocarcinoma.
*Esophageal squamous cell carcinoma*
- Esophageal cancer, including squamous cell carcinoma, is **rarely associated** with SIADH.
- Its paraneoplastic manifestations are less defined and not prominent for ADH production.
*Non-seminomatous germ cell tumor*
- Germ cell tumors, particularly non-seminomatous types, are more commonly associated with paraneoplastic syndromes involving **human chorionic gonadotropin (hCG)** or **alpha-fetoprotein (AFP)** production.
- While some germ cell tumors *can* release ADH, it is **not a primary cause** of SIADH compared to small cell lung cancer.
*Rib osteosarcoma*
- Osteosarcoma is a primary bone tumor and is **not typically associated** with paraneoplastic syndromes like SIADH.
- Its primary clinical manifestations are related to local bone destruction and metastasis.
Water balance and osmoregulation US Medical PG Question 8: A 43-year-old woman is found in the hospital to have a plasma sodium concentration of 126 mg/dL. She was hospitalized after she expressed suicidal ideations and was started on a medication for major depressive disorder. Her past medical history is significant for diabetes for which she is currently taking metformin. Her blood pressure while in the hospital has been around 130/85 mmHg and she is not taking any other medications. Laboratory studies show a serum osmolality of 265 mOsm/kg. Which of the following best describes the cell bodies of the cells that are behaving abnormally in this patient?
- A. Basophils in the anterior pituitary
- B. Chromophobes in the anterior pituitary
- C. Acidophils in the anterior pituitary
- D. Located in the hypothalamus (Correct Answer)
- E. Located in the posterior pituitary
Water balance and osmoregulation Explanation: ***Located in the hypothalamus***
- The patient's **hyponatremia** (126 mg/dL) with a **low serum osmolality** (265 mOsm/kg) in the presence of depression and medication suggests **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- **ADH (vasopressin)** is synthesized in the magnocellular neurosecretory cells of the **hypothalamus** (specifically the supraoptic and paraventricular nuclei) and then transported to the posterior pituitary for release. Since the patient's condition is due to inappropriate ADH secretion, the abnormality originates in the hypothalamus where these cells are located.
*Basophils in the anterior pituitary*
- **Basophils** in the anterior pituitary produce hormones like **TSH, FSH, and LH**, which are not directly involved in the regulation of water balance and sodium levels in the context of SIADH.
- An abnormality in these cells would lead to endocrine dysfunction related to thyroid or gonadal axes, not hyponatremia.
*Chromophobes in the anterior pituitary*
- **Chromophobes** are cells in the anterior pituitary that are typically undifferentiated or degranulated, often representing cells that have released their stored hormones.
- They are not primarily responsible for the production or release of hormones involved in water balance, so an abnormality here is unlikely to cause SIADH.
*Acidophils in the anterior pituitary*
- **Acidophils** in the anterior pituitary produce **growth hormone (GH)** and **prolactin**.
- Abnormalities in these cells would lead to conditions like acromegaly or hyperprolactinemia, neither of which explains the patient's hyponatremia and low serum osmolality.
*Located in the posterior pituitary*
- While the **posterior pituitary** stores and releases **ADH**, it does not synthesize it; the cell bodies responsible for ADH production are in the hypothalamus.
- Therefore, the primary abnormal cells in SIADH are the ones synthesizing ADH in the hypothalamus, not merely storing it in the posterior pituitary.
Water balance and osmoregulation US Medical PG Question 9: A 48-year-old female presents to the emergency room with mental status changes.
Laboratory analysis of the patient's serum shows:
Na 122 mEq/L
K 3.9 mEq/L
HCO3 24 mEq/L
BUN 21 mg/dL
Cr 0.9 mg/dL
Ca 8.5 mg/dL
Glu 105 mg/dL
Urinalysis shows:
Osmolality 334 mOsm/kg
Na 45 mEq/L
Glu 0 mg/dL
Which of the following is the most likely diagnosis?
- A. Diabetes insipidus
- B. Aspirin overdose
- C. Primary polydipsia
- D. Diarrhea
- E. Lung cancer (Correct Answer)
Water balance and osmoregulation Explanation: ***Lung cancer***
- The patient presents with **hyponatremia** (Na 122 mEq/L) and **mental status changes**, along with a **euvolemic state** (normal BUN, creatinine, and potassium), which are characteristic of **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- **Small cell lung cancer** is a common cause of **ectopic ADH production**, leading to SIADH.
*Diabetes insipidus*
- Characterized by **hypernatremia** and the excretion of **large volumes of dilute urine** (low urine osmolality), which contradicts the patient's hyponatremia and relatively concentrated urine (334 mOsm/kg).
- This condition involves insufficient ADH or renal unresponsiveness to ADH, leading to free water loss, not retention.
*Aspirin overdose*
- Typically causes an **acid-base disturbance**, often a mixed respiratory alkalosis and metabolic acidosis, and may lead to **tinnitus** and **hyperthermia**.
- While it can affect mental status, it does not directly explain the specific pattern of **hyponatremia** and urine osmolality observed.
*Primary polydipsia*
- Usually results in **hyponatremia** due to excessive water intake, but the urine would be **maximally dilute** (urine osmolality < 100 mOsm/kg) as the kidneys try to excrete the excess water.
- The patient's urine osmolality of 334 mOsm/kg indicates that the kidneys are still able to concentrate urine somewhat, making primary polydipsia less likely.
*Diarrhea*
- Causes **volume depletion** and can lead to various electrolyte abnormalities, but typically results in **hypernatremia** or isotonic hyponatremia with signs of dehydration.
- The patient's lab values do not show signs of dehydration or a primary gastrointestinal disturbance.
Water balance and osmoregulation US Medical PG Question 10: A 52-year-old woman presents to her primary care physician complaining of 3 weeks of persistent thirst despite consumption of increased quantities of water. She also admits that she has had increased frequency of urination during the same time period. A basic metabolic panel is performed which reveals mild hypernatremia and a normal glucose level. Urine electrolytes are then obtained which shows a very low urine osmolality that does not correct when a water deprivation test is performed. Blood tests reveal an undetectable level of antidiuretic hormone (ADH). Based on this information, what is the most likely cause of this patient's symptoms?
- A. Diabetes mellitus
- B. Central diabetes insipidus (Correct Answer)
- C. Primary polydipsia
- D. Surreptitious diuretic use
- E. Nephrogenic diabetes insipidus
Water balance and osmoregulation Explanation: ***Central diabetes insipidus***
- The patient presents with **polyuria**, **polydipsia**, **hypernatremia**, and a **low urine osmolality** that does not correct with a **water deprivation test**.
- An **undetectable ADH level** confirms a defect in ADH production or release from the pituitary, which is characteristic of central diabetes insipidus.
*Diabetes mellitus*
- This condition is characterized by **hyperglycemia**, which is ruled out by the **normal glucose level** in the basic metabolic panel.
- While it causes polyuria and polydipsia, the underlying mechanism is **osmotic diuresis due to glucose**, not a defect in ADH or renal response to ADH.
*Primary polydipsia*
- In primary polydipsia, patients consume excessive amounts of water, leading to **dilutional hyponatremia** rather than hypernatremia.
- The **ADH levels would be appropriately suppressed** in a patient with primary polydipsia, not undetectable.
*Surreptitious diuretic use*
- Diuretic use would typically lead to **low blood pressure**, **electrolyte imbalances** (e.g., hypokalemia), and a **high urine sodium concentration**, none of which are explicitly mentioned here.
- It would also not result in an **undetectable ADH level** in the absence of an underlying ADH deficiency.
*Nephrogenic diabetes insipidus*
- This condition involves the **kidneys' inability to respond to ADH**, leading to similar symptoms of polyuria and polydipsia with low urine osmolality.
- However, in nephrogenic diabetes insipidus, the **ADH levels would be high or normal** as the pituitary is producing ADH, but the kidneys are not responding.
More Water balance and osmoregulation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.