Integrated nephron function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Integrated nephron function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Integrated nephron function US Medical PG Question 1: Which region of the nephron reabsorbs the highest percentage of filtered bicarbonate?
- A. Collecting duct
- B. Thick ascending limb
- C. Distal tubule
- D. Proximal tubule (Correct Answer)
Integrated nephron function Explanation: ***Proximal tubule***
- The **proximal convoluted tubule (PCT)** reabsorbs approximately 80-90% of the **filtered bicarbonate** through a process involving **carbonic anhydrase** and the **Na+/H+ exchanger**.
- This vital function ensures that the majority of bicarbonate, a key buffer, is returned to the blood to maintain **acid-base balance**.
*Collecting duct*
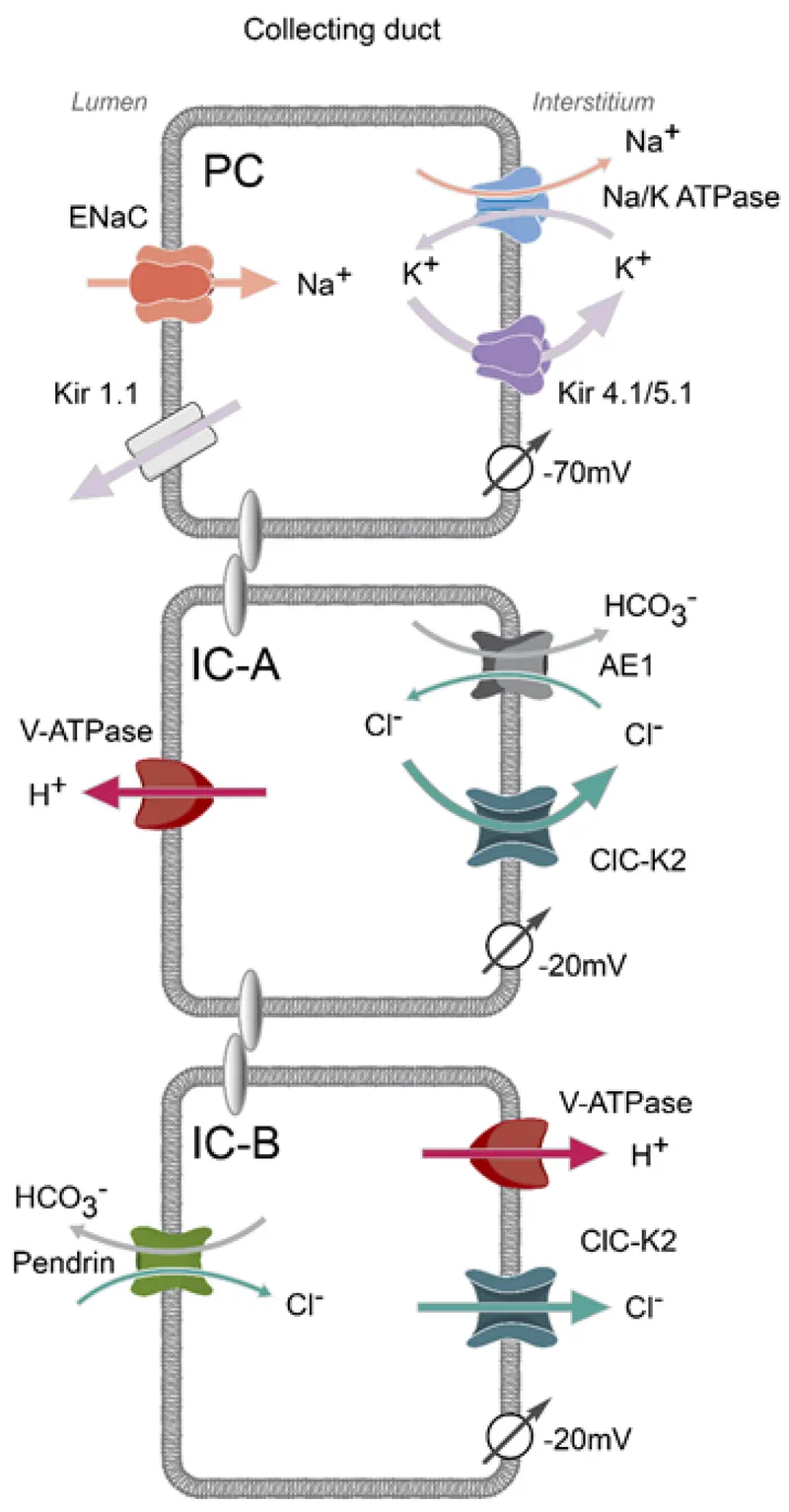
- While the collecting duct does have the ability to reabsorb and secrete bicarbonate, its contribution is minor compared to the PCT, primarily for fine-tuning acid-base balance.
- Cells in the collecting duct, particularly **Type A intercalated cells**, are important for secreting acid (H+) in acidosis and therefore reabsorbing bicarbonate, but not the bulk of it.
*Thick ascending limb*
- The primary role of the **thick ascending limb** is the reabsorption of **sodium**, **potassium**, and **chloride** to create a concentrated interstitium, not significant bicarbonate reabsorption.
- It is largely impermeable to water and is relatively impermeable to bicarbonate.
*Distal tubule*
- The **distal convoluted tubule (DCT)** reabsorbs a small percentage of filtered bicarbonate, but its main role is regulated reabsorption of **sodium** and **calcium**, and secretion of **potassium** and **hydrogen ions**.
- Its contribution to bicarbonate reabsorption is much less significant than that of the proximal tubule.
Integrated nephron function US Medical PG Question 2: Which factor most strongly influences protein filtration at the glomerulus?
- A. Electrical charge
- B. Molecular size (Correct Answer)
- C. Shape
- D. Temperature
Integrated nephron function Explanation: ***Molecular size***
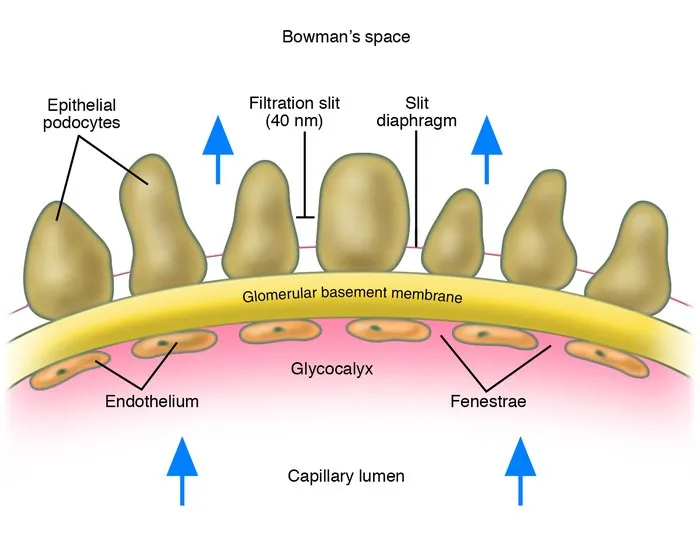
- The glomerular filtration barrier, particularly the **slit diaphragms** between podocytes, acts as a size-selective filter, restricting the passage of larger molecules.
- Proteins like **albumin** (molecular radius ~36 Å, molecular weight ~69 kDa) are significantly large, making them difficult to pass through the filtration barrier.
- Size selectivity is the **primary and most important** factor in protein filtration.
*Electrical charge*
- The glomerular basement membrane contains **negatively charged proteoglycans** (heparan sulfate), which repel negatively charged proteins like albumin, contributing to their retention.
- While important, the role of electrical charge is **secondary** to molecular size in preventing the bulk passage of most proteins.
*Shape*
- While abnormal protein shapes (e.g., **amyloid fibrils**) can impact filtration in specific disease states, the typical physiological filtration of most proteins is primarily governed by size and charge.
- The inherent shape of normal globular proteins plays a less direct role compared to their overall size.
*Temperature*
- **Physiological temperature** is relatively constant in the body and does not directly influence the molecular interactions and physical properties of the glomerular filtration barrier in a way that significantly alters protein filtration.
- Temperature changes would lead to denaturation or aggregation, which are not the primary determinants of normal protein filtration.
Integrated nephron function US Medical PG Question 3: An investigator studying hormone synthesis and transport uses immunocytochemical techniques to localize a carrier protein in the central nervous system of an experimental animal. The investigator finds that this protein is synthesized together with a specific hormone from a composite precursor. The protein is involved in the transport of the hormone from the supraoptic and paraventricular nuclei to its destination. The hormone transported by these carrier proteins is most likely responsible for which of the following functions?
- A. Stimulation of thyroglobulin cleavage
- B. Upregulation of renal aquaporin-2 channels (Correct Answer)
- C. Hyperplasia of the adrenal zona fasciculata
- D. Increased insulin-like growth factor 1 production
- E. Maturation of primordial germ cells
Integrated nephron function Explanation: ***Upregulation of renal aquaporin-2 channels***
- The description of a hormone synthesized in the **supraoptic** and **paraventricular nuclei** and transported by a carrier protein refers to **antidiuretic hormone (ADH)**, also known as vasopressin.
- ADH's primary function in the kidney is to **increase water reabsorption** by upregulating **aquaporin-2 channels** in the principal cells of the collecting ducts.
*Stimulation of thyroglobulin cleavage*
- **Thyroglobulin cleavage** and subsequent release of thyroid hormones (T3, T4) are stimulated by **thyroid-stimulating hormone (TSH)**, which is produced by the anterior pituitary, not the hypothalamus.
- The described origin in the supraoptic and paraventricular nuclei is inconsistent with TSH.
*Hyperplasia of the adrenal zona fasciculata*
- **Adrenocorticotropic hormone (ACTH)** from the anterior pituitary stimulates the adrenal cortex, including the zona fasciculata, to produce cortisol.
- The hormone described here originates in the hypothalamus and is transported to the posterior pituitary, not stimulating adrenal hyperplasia.
*Increased insulin-like growth factor 1 production*
- **Insulin-like growth factor 1 (IGF-1)** production is stimulated primarily by **growth hormone (GH)**, which is secreted by the anterior pituitary.
- This function is not associated with hormones produced in the supraoptic and paraventricular nuclei.
*Maturation of primordial germ cells*
- The maturation of **primordial germ cells** is regulated by **gonadotropins (FSH and LH)**, which are secreted by the anterior pituitary, and sex steroids.
- This process is not directly controlled by hormones originating from the supraoptic and paraventricular nuclei.
Integrated nephron function US Medical PG Question 4: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Integrated nephron function Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
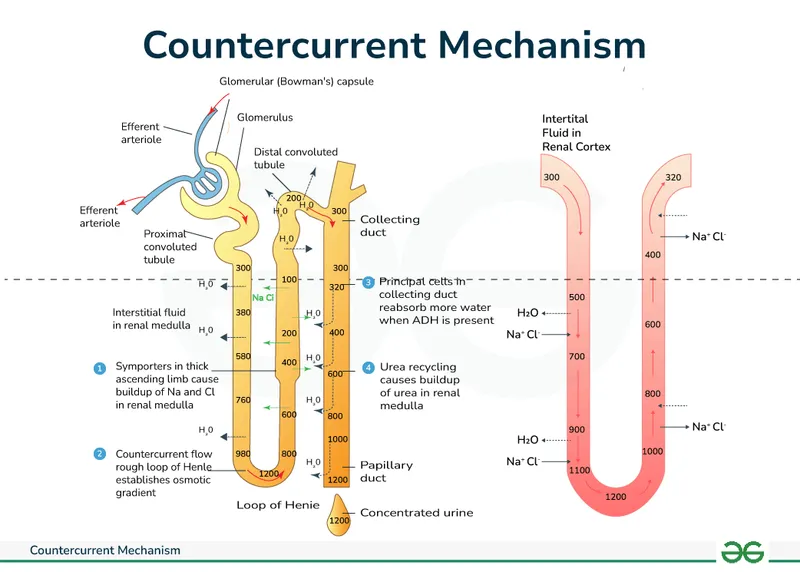
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
Integrated nephron function US Medical PG Question 5: A 66-year-old man with congestive heart failure presents to the emergency department complaining of worsening shortness of breath. These symptoms have worsened over the last 3 days. He has a blood pressure of 126/85 mm Hg and heart rate of 82/min. Physical examination is notable for bibasilar crackles. A chest X-ray reveals bilateral pulmonary edema. His current medications include metoprolol succinate and captopril. You wish to add an additional medication targeted towards his symptoms. Of the following, which statement is correct regarding loop diuretics?
- A. Loop diuretics can cause metabolic acidosis
- B. Loop diuretics can cause ammonia toxicity
- C. Loop diuretics can cause hyperlipidemia
- D. Loop diuretics decrease sodium, magnesium, and chloride but increase calcium
- E. Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter (Correct Answer)
Integrated nephron function Explanation: ***Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter***
- Loop diuretics, like furosemide, directly block the **Na+/K+/2Cl- cotransporter** in the **thick ascending limb of the loop of Henle**, preventing the reabsorption of these ions.
- This inhibition leads to increased excretion of water, sodium, potassium, and chloride, which is beneficial in conditions like **pulmonary edema** due to **congestive heart failure**.
*Loop diuretics can cause metabolic acidosis*
- Loop diuretics typically cause **metabolic alkalosis**, not acidosis, because they increase the excretion of hydrogen ions and potassium, leading to a compensatory increase in bicarbonate.
- The increased delivery of sodium to the collecting duct can also stimulate potassium and hydrogen secretion, contributing to alkalosis.
*Loop diuretics can cause ammonia toxicity*
- Loop diuretics do not directly cause **ammonia toxicity**; this is more commonly associated with conditions like **hepatic encephalopathy** or certain other medications.
- Their primary mechanism of action is on renal ion transport, not ammonia metabolism.
*Loop diuretics can cause hyperlipidemia*
- While some diuretics like **thiazide diuretics** can cause mild increases in **lipid levels**, loop diuretics are not typically associated with significant **hyperlipidemia**.
- The most common metabolic side effects of loop diuretics include electrolyte imbalances.
*Loop diuretics decrease sodium, magnesium, and chloride but increase calcium*
- Loop diuretics decrease the reabsorption of **sodium**, **magnesium**, and **chloride**, leading to their increased excretion.
- They also increase **calcium excretion** (cause hypocalcemia), rather than increasing serum calcium levels, by inhibiting its reabsorption in the thick ascending limb of the loop of Henle.
Integrated nephron function US Medical PG Question 6: A new drug X is being tested for its effect on renal function. During the experiments, the researchers found that in patients taking substance X, the urinary concentration of sodium decreases while urine potassium concentration increase. Which of the following affects the kidneys in the same way as does substance X?
- A. Aldosterone (Correct Answer)
- B. Furosemide
- C. Spironolactone
- D. Atrial natriuretic peptide
- E. Hydrochlorothiazide
Integrated nephron function Explanation: ***Aldosterone***
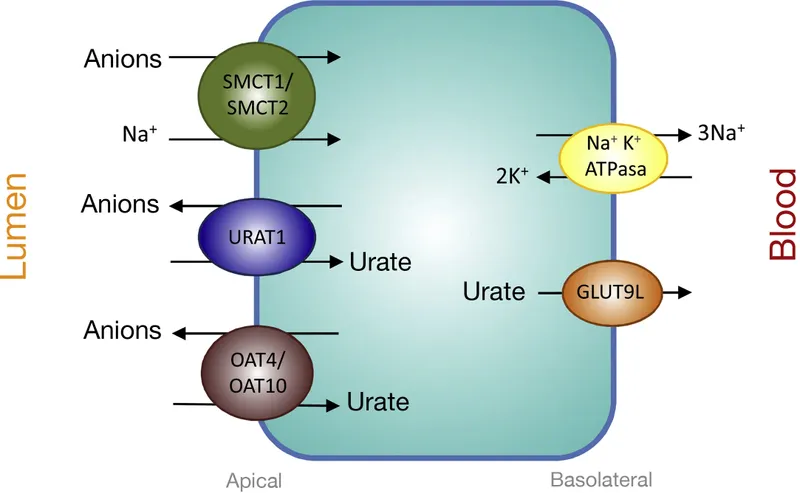
- **Aldosterone** acts on the **principal cells** of the **collecting duct** to increase sodium reabsorption and potassium secretion.
- This action leads to a decrease in urinary sodium concentration and an increase in urinary potassium concentration, matching the effects of drug X.
*Furosemide*
- **Furosemide** is a **loop diuretic** that inhibits the **Na-K-2Cl cotransporter** in the **thick ascending limb** of the loop of Henle.
- This inhibition leads to increased excretion of sodium, potassium, and water, resulting in higher urinary sodium concentration.
*Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that blocks aldosterone's effects on the collecting duct.
- This leads to increased sodium excretion and decreased potassium excretion (potassium-sparing effect), which is the opposite of drug X.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** is released in response to atrial stretch and causes **natriuresis** (increased sodium excretion) and **diuresis**.
- It works by dilating afferent arterioles and constricting efferent arterioles, increasing GFR, and inhibiting sodium reabsorption, thus increasing urinary sodium concentration.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that inhibits the **Na-Cl cotransporter** in the **distal convoluted tubule**.
- This leads to increased sodium and chloride excretion but typically causes potassium wasting (hypokalemia), which differs from the increased urinary potassium concentration seen with drug X.
Integrated nephron function US Medical PG Question 7: A 17-year-old boy is brought to the physician by his father because of a 7-month history of fatigue, recurrent leg cramps, and increased urinary frequency. His pulse is 94/min and blood pressure is 118/85 mm Hg. Physical examination shows dry mucous membranes. Laboratory studies show:
Serum
Na+ 130 mEq/L
K+ 2.8 mEq/L
Cl- 92 mEq/L
Mg2+ 1.1 mEq/L
Ca2+ 10.6 mg/dL
Albumin 5.2 g/dL
Urine
Ca2+ 70 mg/24 h
Cl- 375 mEq/24h (N = 110–250)
Arterial blood gas analysis on room air shows a pH of 7.55 and an HCO3- concentration of 45 mEq/L. Impaired function of which of the following structures is the most likely cause of this patient's condition?
- A. Ascending loop of Henle
- B. Collecting duct
- C. Distal convoluted tubule (Correct Answer)
- D. Descending loop of Henle
- E. Proximal convoluted tubule
Integrated nephron function Explanation: ***Distal convoluted tubule***
- The patient presents with **hypokalemia**, **metabolic alkalosis**, **hypomagnesemia**, and **hypocalciuria** (24-hour urine Ca2+ 70 mg, normal up to 250 mg), which are characteristic findings of **Gitelman syndrome**.
- **Gitelman syndrome** is caused by a loss-of-function mutation in the **thiazide-sensitive Na-Cl cotransporter (NCC)**, located in the **distal convoluted tubule**, leading to impaired reabsorption of Na+ and Cl- at this segment.
*Ascending loop of Henle*
- Impaired function of the **Na-K-2Cl cotransporter (NKCC2)** in the **thick ascending limb of the loop of Henle** causes **Bartter syndrome**.
- Bartter syndrome typically presents with **hypercalciuria**, in contrast to the hypocalciuria seen in this patient.
*Collecting duct*
- Dysfunction of the **collecting duct** can lead to various conditions, such as **renal tubular acidosis** or **diabetes insipidus**, depending on which channels or receptors are affected.
- However, the specific combination of **hypokalemia**, **metabolic alkalosis**, **hypomagnesemia**, and **hypocalciuria** points away from primary collecting duct dysfunction.
*Descending loop of Henle*
- The **descending loop of Henle** is primarily permeable to **water** and has a limited role in electrolyte reabsorption.
- Impairment here would primarily affect **urine concentration** and dilution but would not account for the specific electrolyte imbalances observed.
*Proximal convoluted tubule*
- The **proximal convoluted tubule** is responsible for reabsorbing a large fraction of filtered electrolytes, glucose, and amino acids.
- Dysfunction here (e.g., **Fanconi syndrome**) would typically present with **generalized aminoaciduria**, **glycosuria**, **phosphaturia**, and **proximal renal tubular acidosis**, which are not seen in this patient.
Integrated nephron function US Medical PG Question 8: A 57-year-old male is found to have an elevated prostate specific antigen (PSA) level on screening labwork. PSA may be elevated in prostate cancer, benign prostatic hypertrophy (BPH), or prostatitis. Which of the following best describes the physiologic function of PSA?
- A. Regulation of transcription factors and phosphorylation of proteins
- B. Maintains corpus luteum
- C. Response to peritoneal irritation
- D. Sperm production
- E. Liquefaction of semen (Correct Answer)
Integrated nephron function Explanation: ***Liquefaction of semen***
- Prostate-specific antigen (PSA) is a **serine protease** produced by the epithelial cells of the prostate gland.
- Its primary physiological role is to **liquefy the seminal coagulum** formed after ejaculation, allowing sperm to become motile and navigate the female reproductive tract.
*Regulation of transcription factors and phosphorylation of proteins*
- This function is characteristic of **kinases** and **phosphatases**, which are involved in intracellular signaling pathways.
- While essential for cellular function, it does not describe the specific role of PSA.
*Maintains corpus luteum*
- The maintenance of the corpus luteum is primarily the role of **luteinizing hormone (LH)** and, in pregnancy, **human chorionic gonadotropin (hCG)**.
- These hormones are involved in the female reproductive cycle, unrelated to PSA.
*Response to peritoneal irritation*
- Peritoneal irritation triggers an inflammatory response involving various immune cells and mediators, but not specifically PSA.
- PSA itself is not directly involved in the systemic or local response to peritoneal inflammation.
*Sperm production*
- **Sperm production (spermatogenesis)** occurs in the seminiferous tubules of the testes under the influence of hormones like FSH and testosterone.
- While semen is the vehicle for sperm, PSA's role is in the post-ejaculatory processing of semen, not in the initial production of sperm.
Integrated nephron function US Medical PG Question 9: An 81-year-old man presents to his primary care physician for his yearly exam. His past medical history is significant for osteopenia, nephrolithiasis, and hypertension. His family history is significant for relatives who had early onset kidney failure. He takes occasional acetaminophen and supplemental calcium/vitamin D. He is physically active with a normal body mass index (BMI) and has no current concerns. Review of his laboratory results today were compared with those from 15 years ago with the following findings:
Results today:
Serum creatinine concentration: 1.1 mg/dL
Urine creatinine concentration: 100 mg/dL
Urine volume: 1000 mL/day
Results 15 years ago:
Serum creatinine concentration: 1.1 mg/dL
Urine creatinine concentration: 120 mg/dL
Urine volume: 1000 mL/day
Which is the most likely cause of these changes in his creatinine clearance?
- A. Renovascular disease
- B. Nephrolithiasis
- C. Normal aging (Correct Answer)
- D. Polycystic kidney disease
- E. Benign prostatic hyperplasia
Integrated nephron function Explanation: ***Normal aging***
- As individuals **age**, there is a natural decline in **glomerular filtration rate (GFR)** due to nephron loss and sclerotic changes, even with a stable serum creatinine.
- The drop in **urine creatinine concentration** over 15 years, combined with a stable serum creatinine and urine volume, indicates a reduction in muscle mass and creatinine production, which is typical for an 81-year-old, thereby masking a decline in GFR.
*Renovascular disease*
- This typically causes a **drop in GFR** or **acute kidney injury**, often with a **rise in serum creatinine**.
- There is no increase in serum creatinine in this patient, and the presentation does not suggest **flash pulmonary edema** or **uncontrolled hypertension**.
*Nephrolithiasis*
- While the patient has a history of nephrolithiasis, it typically causes **acute, severe flank pain** or **obstructive kidney injury** when significant.
- There are no symptoms of acute obstruction, nor is there a significant increase in serum creatinine that would suggest a new stone causing obstruction.
*Polycystic kidney disease*
- This is a **genetic disorder** causing multiple cysts in the kidneys, leading to progressive kidney failure, often with a **family history of early-onset kidney failure**.
- While the family history is relevant, there are **no symptoms or physical exam findings** suggestive of PKD, such as kidney enlargement or hematuria.
*Benign prostatic hyperplasia*
- BPH can cause **obstructive uropathy** and a **rise in serum creatinine**, particularly if it leads to urinary retention.
- The patient has a normal urine volume and no symptoms of urinary obstruction such as **hesitancy, weak stream, or nocturia**.
Integrated nephron function US Medical PG Question 10: A 28-year-old research assistant is brought to the emergency department for severe chemical burns 30 minutes after accidentally spilling hydrochloric acid on himself. The burns cover both hands and forearms. His temperature is 37°C (98.6°F), pulse is 112/min, respirations are 20/min, and blood pressure is 108/82 mm Hg. Initial stabilization and resuscitation is begun, including respiratory support, fluid resuscitation, and cardiovascular stabilization. The burned skin is irrigated with saline water to remove the chemical agent. Which of the following is the most appropriate method to verify adequate fluid infusion in this patient?
- A. The Parkland formula
- B. Blood pressure
- C. Pulmonary capillary wedge pressure
- D. Heart rate
- E. Urinary output (Correct Answer)
Integrated nephron function Explanation: ***Urinary output***
- Maintaining a specific **urinary output** (e.g., adult with major burns: 0.5-1.0 mL/kg/hr or 30-50 mL/hr) is the most reliable clinical indicator of adequate fluid resuscitation in burn patients.
- This ensures sufficient end-organ perfusion and avoids both under-resuscitation (leading to shock and organ damage) and over-resuscitation (risk of compartment syndrome and pulmonary edema).
*The Parkland formula*
- The **Parkland formula** is used to *calculate* the initial fluid volume needed, but it does not *verify* the adequacy of the infusion once started.
- This formula provides a starting point for fluid administration, which then needs to be adjusted based on the patient's response.
*Blood pressure*
- **Blood pressure** can be misleading in burn patients; it may remain deceptively normal due to compensatory mechanisms even with significant fluid deficits.
- It is a late indicator of hypovolemic shock, and relying solely on it can lead to under-resuscitation.
*Pulmonary capillary wedge pressure*
- **Pulmonary capillary wedge pressure (PCWP)** requires invasive monitoring via a pulmonary artery catheter, which is rarely indicated for routine fluid management in burn patients due to its invasiveness and associated risks.
- Less invasive and equally effective methods, like urinary output, are preferred for monitoring resuscitation.
*Heart rate*
- **Heart rate** is a sensitive but non-specific indicator of fluid status; it can be elevated due to pain, anxiety, or infection, not solely hypovolemia.
- While a decreasing heart rate can indicate improved fluid status, it is not as reliable or direct an indicator of end-organ perfusion as urinary output.
More Integrated nephron function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.