Countercurrent multiplication system US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Countercurrent multiplication system. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Countercurrent multiplication system US Medical PG Question 1: A researcher is studying the effects of a new antihypertensive medication on urine osmolality. She first measures urine osmolality in different parts of the nephron of a healthy human control. The findings are shown below:
Portion of nephron Urine osmolality (mOsmol/kg)
Proximal convoluted tubule 300
Loop of Henle, descending limb 1200
Loop of Henle, ascending limb 200
Distal convoluted tubule 100
Collecting duct 600
Which of the following is the most likely explanation for the urine osmolality in the ascending limb of the loop of Henle?
- A. Increased urea excretion
- B. Increased transcription of water channels
- C. Impermeability to water (Correct Answer)
- D. Increased bicarbonate reabsorption
- E. Impermeability to sodium
Countercurrent multiplication system Explanation: ***Impermeability to water***
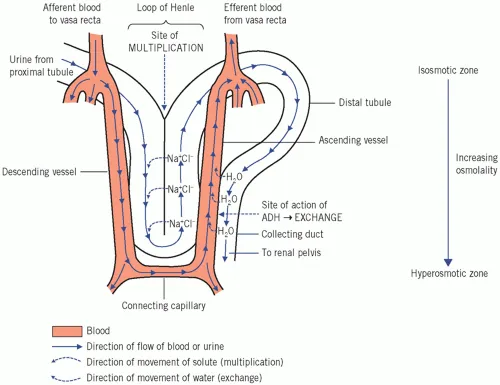
- The **ascending limb of the loop of Henle** is notable for its **water impermeability** due to the absence of aquaporins.
- This impermeability, coupled with active reabsorption of solutes, leads to the production of **hypoosmotic fluid** (200 mOsmol/kg) in this segment.
*Increased urea excretion*
- While urea is a major contributor to medullary osmolality and is excreted, it is primarily reabsorbed in the **collecting duct** and secreted into the loop of Henle, not directly explaining the low osmolality in the ascending limb.
- Increased urea excretion on its own would likely lead to a higher, not lower, osmolality of the urine exiting the kidney.
*Increased transcription of water channels*
- Increased transcription of water channels (**aquaporins**) would make the tubule more permeable to water, leading to water reabsorption and an **increase in osmolality**, which contradicts the observed hypoosmotic fluid.
- The ascending limb is primarily involved in **solute reabsorption** without water, making it dilute.
*Increased bicarbonate reabsorption*
- **Bicarbonate reabsorption** primarily occurs in the **proximal tubule** and is crucial for acid-base balance, not directly impacting the dramatic osmolality changes in the ascending limb.
- While some bicarbonate is reabsorbed in the ascending limb, it does not explain the significant decrease in fluid osmolality.
*Impermeability to sodium*
- The ascending limb is **highly permeable to sodium** and actively reabsorbs it via the **Na-K-2Cl cotransporter**, which is crucial for diluting the tubular fluid.
- If it were impermeable to sodium, the reabsorption of solutes would cease, and the osmolality would not decrease as observed.
Countercurrent multiplication system US Medical PG Question 2: A 42-year-old man is brought to the emergency room because of confusion. His wife says he has been urinating more frequently than usual for the past 3 days. He has not had fever or dysuria. He has bipolar disorder, for which he takes lithium. His pulse is 105/min, and respirations are 14/min. He is lethargic and oriented only to person. Physical examination shows dry mucous membranes and increased capillary refill time. Laboratory studies show a serum sodium concentration of 158 mEq/L and an antidiuretic hormone (ADH) concentration of 8 pg/mL (N = 1–5). Which of the following is the most likely site of dysfunction in this patient?
- A. Hypothalamic supraoptic nucleus
- B. Descending loop of Henle
- C. Juxtaglomerular apparatus
- D. Collecting duct (Correct Answer)
- E. Posterior pituitary gland
Countercurrent multiplication system Explanation: ***Collecting duct***
- The patient presents with **hypernatremia** (Na 158 mEq/L), **polyuria**, and **dehydration** (dry mucous membranes, increased capillary refill time, confusion), indicative of **nephrogenic diabetes insipidus**.
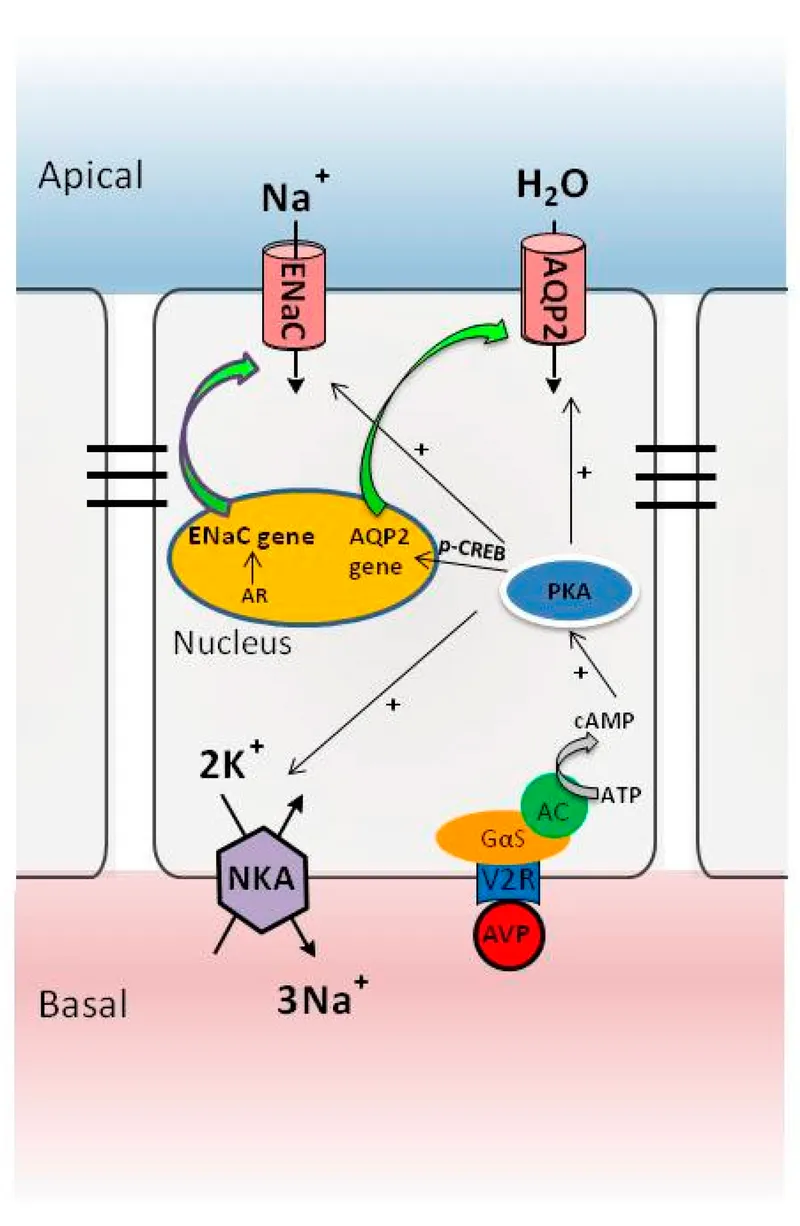
- His ADH level is **elevated** (8 pg/mL), suggesting that the kidneys are not responding to ADH; the **collecting ducts** are the primary site where ADH exerts its effect via aquaporin-2 channels to reabsorb water.
- **Lithium**, which this patient is taking for bipolar disorder, is a well-known cause of nephrogenic diabetes insipidus by interfering with ADH action at the collecting duct level.
*Hypothalamic supraoptic nucleus*
- This nucleus is responsible for synthesizing **ADH**. Dysfunction here would lead to **decreased ADH production** (central diabetes insipidus), but the patient's ADH level is elevated.
- A lack of ADH from this area would not explain the kidney's unresponsiveness to the high ADH levels observed.
*Descending loop of Henle*
- The descending loop of Henle is permeable to water but not directly responsible for ADH-mediated water reabsorption that is impaired in diabetes insipidus.
- Its primary role is to concentrate the filtrate as it descends into the hypertonic medulla.
*Juxtaglomerular apparatus*
- The juxtaglomerular apparatus regulates **blood pressure** and **glomerular filtration rate** through the **renin-angiotensin-aldosterone system**.
- While important for kidney function, it's not directly involved in the ADH-mediated water reabsorption whose impairment leads to nephrogenic diabetes insipidus.
*Posterior pituitary gland*
- This gland stores and releases ADH, which is synthesized in the hypothalamus.
- If the posterior pituitary were dysfunctional, it would lead to **decreased ADH release** (central diabetes insipidus), contradicting the patient's **elevated ADH level**.
Countercurrent multiplication system US Medical PG Question 3: A 66-year-old man with congestive heart failure presents to the emergency department complaining of worsening shortness of breath. These symptoms have worsened over the last 3 days. He has a blood pressure of 126/85 mm Hg and heart rate of 82/min. Physical examination is notable for bibasilar crackles. A chest X-ray reveals bilateral pulmonary edema. His current medications include metoprolol succinate and captopril. You wish to add an additional medication targeted towards his symptoms. Of the following, which statement is correct regarding loop diuretics?
- A. Loop diuretics can cause metabolic acidosis
- B. Loop diuretics can cause ammonia toxicity
- C. Loop diuretics can cause hyperlipidemia
- D. Loop diuretics decrease sodium, magnesium, and chloride but increase calcium
- E. Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter (Correct Answer)
Countercurrent multiplication system Explanation: ***Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter***
- Loop diuretics, like furosemide, directly block the **Na+/K+/2Cl- cotransporter** in the **thick ascending limb of the loop of Henle**, preventing the reabsorption of these ions.
- This inhibition leads to increased excretion of water, sodium, potassium, and chloride, which is beneficial in conditions like **pulmonary edema** due to **congestive heart failure**.
*Loop diuretics can cause metabolic acidosis*
- Loop diuretics typically cause **metabolic alkalosis**, not acidosis, because they increase the excretion of hydrogen ions and potassium, leading to a compensatory increase in bicarbonate.
- The increased delivery of sodium to the collecting duct can also stimulate potassium and hydrogen secretion, contributing to alkalosis.
*Loop diuretics can cause ammonia toxicity*
- Loop diuretics do not directly cause **ammonia toxicity**; this is more commonly associated with conditions like **hepatic encephalopathy** or certain other medications.
- Their primary mechanism of action is on renal ion transport, not ammonia metabolism.
*Loop diuretics can cause hyperlipidemia*
- While some diuretics like **thiazide diuretics** can cause mild increases in **lipid levels**, loop diuretics are not typically associated with significant **hyperlipidemia**.
- The most common metabolic side effects of loop diuretics include electrolyte imbalances.
*Loop diuretics decrease sodium, magnesium, and chloride but increase calcium*
- Loop diuretics decrease the reabsorption of **sodium**, **magnesium**, and **chloride**, leading to their increased excretion.
- They also increase **calcium excretion** (cause hypocalcemia), rather than increasing serum calcium levels, by inhibiting its reabsorption in the thick ascending limb of the loop of Henle.
Countercurrent multiplication system US Medical PG Question 4: Which transport mechanism is primarily responsible for calcium reabsorption in the proximal tubule?
- A. Paracellular transport (Correct Answer)
- B. Facilitated diffusion
- C. Active transport
- D. Antiport with sodium
Countercurrent multiplication system Explanation: ***Paracellular transport***
- In the **proximal tubule**, approximately 60-70% of filtered calcium is reabsorbed primarily through the **paracellular pathway**, driven by the electrochemical gradient and solvent drag.
- This transport occurs between cells, moving through the **tight junctions**, and is passive, following the reabsorption of water.
*Facilitated diffusion*
- While a type of passive transport, **facilitated diffusion** typically involves membrane proteins and occurs across the cell membrane, not primarily between cells in the proximal tubule for calcium.
- This mechanism is prominent for calcium reabsorption in other nephron segments like the **distal convoluted tubule** via **TRPV5/6 channels**, but not the main route in the proximal tubule.
*Active transport*
- **Active transport** of calcium, mainly via **calcium ATPase** and the **Na+/Ca2+ exchanger**, occurs across the luminal and basolateral membranes, respectively, in specific nephron segments.
- However, in the **proximal tubule**, the bulk of calcium reabsorption is passive and paracellular, not ATP-dependent active transport across cell membranes.
*Antiport with sodium*
- The **Na+/Ca2+ exchanger (NCX)** is an antiport mechanism that plays a crucial role in extruding calcium from the cell into the interstitium, particularly in the basolateral membrane of the distal tubule.
- However, it is not the primary mechanism for overall tubular reabsorption of calcium in the **proximal tubule**, where paracellular movement dominates.
Countercurrent multiplication system US Medical PG Question 5: A 32-year-old woman presents with a 3-month history of intermittent blurred vision and problems walking. The patient states that she often feels “pins and needles” in her legs that cause her problems when she’s walking. The patient is afebrile, and her vital signs are within normal limits. An autoimmune disorder is suspected. Which of the following findings would most likely be present in this patient?
- A. Damaged myelin sheath and myelin-producing cells (Correct Answer)
- B. Absence of interneurons
- C. Destruction of blood-brain barrier
- D. Degeneration of anterior horn cells
- E. Decreased cerebrospinal fluid due to destruction of cells
Countercurrent multiplication system Explanation: ***Damaged myelin sheath and myelin-producing cells***
- The patient's symptoms of intermittent **blurred vision** (optic neuritis), **problems walking** (ataxia, spasticity), and **paresthesias** ("pins and needles") are classical presentations of Multiple Sclerosis (MS).
- MS is characterized by multifocal areas of inflammation and **demyelination** in the central nervous system, where the **myelin sheath** surrounding axons is damaged, and the **oligodendrocytes** (myelin-producing cells) are attacked.
- This demyelination disrupts saltatory conduction, leading to the varied and intermittent neurological symptoms.
*Absence of interneurons*
- The absence of **interneurons** is typically associated with conditions like **spinal muscular atrophy** or certain **neuropathies**, which present with different clinical features (e.g., muscle weakness, atrophy) than those described.
- While interneurons are crucial for neuronal communication, their absence doesn't explain the *intermittent* and multifocal symptoms seen in this case.
*Destruction of blood-brain barrier*
- While **blood-brain barrier (BBB) breakdown** does occur in MS, it is a *consequence* of the inflammatory process rather than the primary *pathological finding* that directly explains the neurological symptoms.
- BBB destruction allows inflammatory cells to enter the CNS, contributing to demyelination, but the core issue remains the myelin damage itself.
*Degeneration of anterior horn cells*
- **Anterior horn cell degeneration** is the hallmark of **amyotrophic lateral sclerosis (ALS)** and **spinal muscular atrophy**, presenting with progressive muscle weakness, atrophy, and fasciculations.
- These conditions lack the sensory symptoms (paresthesias) and visual disturbances seen in this patient, and typically show a progressive rather than intermittent course.
*Decreased cerebrospinal fluid due to destruction of cells*
- **Decreased CSF volume** is not a characteristic feature of MS; in fact, CSF analysis often shows increased protein and **oligoclonal bands**.
- The destruction of cells in MS primarily affects myelin and oligodendrocytes, not cells responsible for CSF production or volume regulation.
Countercurrent multiplication system US Medical PG Question 6: An investigator studying hormone synthesis and transport uses immunocytochemical techniques to localize a carrier protein in the central nervous system of an experimental animal. The investigator finds that this protein is synthesized together with a specific hormone from a composite precursor. The protein is involved in the transport of the hormone from the supraoptic and paraventricular nuclei to its destination. The hormone transported by these carrier proteins is most likely responsible for which of the following functions?
- A. Stimulation of thyroglobulin cleavage
- B. Upregulation of renal aquaporin-2 channels (Correct Answer)
- C. Hyperplasia of the adrenal zona fasciculata
- D. Increased insulin-like growth factor 1 production
- E. Maturation of primordial germ cells
Countercurrent multiplication system Explanation: ***Upregulation of renal aquaporin-2 channels***
- The description of a hormone synthesized in the **supraoptic** and **paraventricular nuclei** and transported by a carrier protein refers to **antidiuretic hormone (ADH)**, also known as vasopressin.
- ADH's primary function in the kidney is to **increase water reabsorption** by upregulating **aquaporin-2 channels** in the principal cells of the collecting ducts.
*Stimulation of thyroglobulin cleavage*
- **Thyroglobulin cleavage** and subsequent release of thyroid hormones (T3, T4) are stimulated by **thyroid-stimulating hormone (TSH)**, which is produced by the anterior pituitary, not the hypothalamus.
- The described origin in the supraoptic and paraventricular nuclei is inconsistent with TSH.
*Hyperplasia of the adrenal zona fasciculata*
- **Adrenocorticotropic hormone (ACTH)** from the anterior pituitary stimulates the adrenal cortex, including the zona fasciculata, to produce cortisol.
- The hormone described here originates in the hypothalamus and is transported to the posterior pituitary, not stimulating adrenal hyperplasia.
*Increased insulin-like growth factor 1 production*
- **Insulin-like growth factor 1 (IGF-1)** production is stimulated primarily by **growth hormone (GH)**, which is secreted by the anterior pituitary.
- This function is not associated with hormones produced in the supraoptic and paraventricular nuclei.
*Maturation of primordial germ cells*
- The maturation of **primordial germ cells** is regulated by **gonadotropins (FSH and LH)**, which are secreted by the anterior pituitary, and sex steroids.
- This process is not directly controlled by hormones originating from the supraoptic and paraventricular nuclei.
Countercurrent multiplication system US Medical PG Question 7: An investigator is studying physiologic renal responses to common medical conditions. She measures urine osmolalities in different parts of the nephron of a human subject in the emergency department. The following values are obtained:
Portion of nephron Osmolality (mOsmol/kg)
Proximal convoluted tubule 300
Loop of Henle, descending limb 1200
Loop of Henle, ascending limb 250
Distal convoluted tubule 100
Collecting duct 1200
These values were most likely obtained from an individual with which of the following condition?
- A. Gitelman syndrome
- B. Psychogenic polydipsia
- C. Furosemide overdose
- D. Dehydration (Correct Answer)
- E. Diabetes insipidus
Countercurrent multiplication system Explanation: ***Dehydration***
- The high osmolality in the **collecting duct (1200 mOsmol/kg)** indicates the kidney is actively conserving water, a normal physiological response to **dehydration**.
- In dehydration, **antidiuretic hormone (ADH)** levels are high, leading to increased water reabsorption in the collecting ducts and thus a concentrated urine.
*Gitelman syndrome*
- This condition involves a defect in the **NaCl cotransporter** in the **distal convoluted tubule**, leading to impaired sodium reabsorption.
- Patients typically present with significant **hypokalemia**, metabolic alkalosis, and a relatively dilute urine, which is not consistent with the given osmolality values.
*Psychogenic polydipsia*
- Individuals with psychogenic polydipsia consume excessive amounts of water, leading to **dilute urine** (low urine osmolality) as a compensatory mechanism to excrete the excess water.
- This would result in much lower osmolality values throughout the nephron, particularly in the collecting duct, compared to the values provided.
*Furosemide overdose*
- Furosemide is a **loop diuretic** that inhibits the reabsorption of sodium and chloride in the **thick ascending limb of the loop of Henle**.
- This would impair the kidney's ability to concentrate urine, leading to a much **lower osmolality in the collecting duct** than observed in this scenario.
*Diabetes insipidus*
- Diabetes insipidus (DI) is characterized by either a deficiency in ADH (central DI) or unresponsiveness to ADH (nephrogenic DI).
- In both types, the kidney cannot concentrate urine effectively, resulting in the production of a **large volume of very dilute urine** (low urine osmolality, typically <300 mOsmol/kg), which contradicts the high collecting duct osmolality.
Countercurrent multiplication system US Medical PG Question 8: Renal clearance of substance Y is experimentally studied. At a constant glomerular filtration rate, it is found that the amount of substance Y excreted is greater than the amount filtered. This holds true across all physiologic values on the titration curve. Substance Y is most similar to which of the following?
- A. Para-amino hippuric acid (Correct Answer)
- B. Albumin
- C. Bicarbonate
- D. Magnesium
- E. Glucose
Countercurrent multiplication system Explanation: ***Para-amino hippuric acid***
- If the amount of a substance excreted is **greater than the amount filtered**, it indicates that the substance undergoes both **glomerular filtration** and **tubular secretion**.
- **Para-amino hippuric acid (PAH)** is a classic example of a substance that is extensively filtered and actively secreted by the renal tubules, making its clearance rate very high and a good estimate of **renal plasma flow**.
*Albumin*
- **Albumin** is a large protein that is normally **not filtered** by the glomerulus due to its size and negative charge.
- Its presence in the urine, indicating a greater amount excreted than filtered (which is normally zero), would suggest **glomerular damage**, but it does not undergo active tubular secretion.
*Bicarbonate*
- **Bicarbonate** is freely filtered at the glomerulus and is primarily **reabsorbed** in the renal tubules, particularly in the proximal tubule.
- Therefore, the amount of bicarbonate excreted is typically **much less than** the amount filtered, not greater.
*Magnesium*
- **Magnesium** is filtered by the glomeruli and undergoes complex regulation involving both **reabsorption and secretion** in various parts of the renal tubule, though reabsorption predominates.
- While magnesium balance is maintained by the kidneys, its excretion does not typically exceed filtration to the extent described for substances primarily handled by secretion.
*Glucose*
- **Glucose** is freely filtered at the glomerulus and is almost **completely reabsorbed** in the proximal tubule under normal physiological conditions.
- The amount of glucose excreted is typically zero, and only exceeds filtration when the **tubular reabsorptive capacity is saturated**, as in uncontrolled diabetes, but it is reabsorbed, not secreted.
Countercurrent multiplication system US Medical PG Question 9: A 30-year-old man presents to his physician for a follow-up appointment for a blood pressure of 140/90 mm Hg during his last visit. He was advised to record his blood pressure at home with an automated device twice every day. He recorded a wide range of blood pressure values in the past week, ranging from 110/70 mm Hg to 135/84 mm Hg. The medical history is unremarkable and he takes no medications. He occasionally drinks alcohol after work, but denies smoking and illicit drug use. Which of the following factors is responsible for maintaining a near-normal renal blood flow over a wide range of systemic blood pressures?
- A. Glomerular filtration
- B. Afferent arteriole (Correct Answer)
- C. Aldosterone
- D. Sympathetic nervous system
- E. Efferent arteriole
Countercurrent multiplication system Explanation: ***Afferent arteriole***
- The **afferent arteriole** is the **primary site** of **renal autoregulation**, which maintains constant renal blood flow over a wide range of systemic blood pressures (80-180 mm Hg).
- Two key mechanisms operate here: (1) **Myogenic mechanism** - smooth muscle in the afferent arteriole constricts in response to increased stretch from elevated blood pressure, and dilates when pressure decreases; (2) **Tubuloglomerular feedback** - involves juxtaglomerular apparatus sensing changes in distal tubule NaCl delivery and adjusting afferent arteriolar tone.
- The afferent arteriole is the **initial and dominant** site where resistance changes occur to buffer pressure fluctuations before they affect glomerular capillaries.
*Glomerular filtration*
- **Glomerular filtration** is the process by which blood is filtered in the glomerulus, forming an ultrafiltrate.
- This is the **outcome** that autoregulation protects, not the mechanism itself.
- Autoregulation maintains stable GFR despite blood pressure changes.
*Aldosterone*
- **Aldosterone** is a mineralocorticoid hormone that regulates **sodium and water reabsorption** in the distal tubule and collecting duct.
- It acts over hours to days and regulates **volume status** and **chronic blood pressure control**, not acute autoregulation.
- Does not directly regulate renal blood flow in response to acute systemic blood pressure changes.
*Sympathetic nervous system*
- The **sympathetic nervous system** releases **norepinephrine**, causing **vasoconstriction** of both afferent and efferent arterioles.
- This is an **extrinsic** control mechanism that overrides autoregulation during severe stress, hemorrhage, or extreme hypotension.
- Within the **normal autoregulatory range** (80-180 mm Hg), intrinsic mechanisms (myogenic and tubuloglomerular feedback) predominate, not sympathetic control.
*Efferent arteriole*
- The **efferent arteriole** does contribute to GFR regulation, primarily through **angiotensin II-mediated constriction** which helps maintain GFR when renal perfusion pressure drops.
- However, the **primary autoregulatory adjustments** to maintain constant renal blood flow occur at the **afferent arteriole** level through the myogenic mechanism.
- The efferent arteriole plays a more significant role in maintaining GFR during hypotension rather than buffering blood flow changes across the full autoregulatory range.
Countercurrent multiplication system US Medical PG Question 10: An investigator is studying bone metabolism and compares the serum studies and bone biopsy findings of a cohort of women 25–35 years of age with those from a cohort of women 55–65 years of age. Which of the following processes is most likely to be increased in the cohort of older women?
- A. Urinary excretion of cyclic AMP
- B. Expression of RANK ligand (Correct Answer)
- C. Demineralization of bone with normal osteoid matrix
- D. Activation of fibroblast growth factor receptor 3
- E. Urinary excretion of osteocalcin
Countercurrent multiplication system Explanation: ***Expression of RANK ligand***
- As women age, especially after **menopause**, estrogen levels decline, leading to an **increase in pro-resorptive cytokines**.
- This imbalance promotes increased **RANK ligand (RANKL)** expression, which stimulates **osteoclast differentiation and activity**, resulting in increased bone resorption.
*Urinary excretion of cyclic AMP*
- **Urinary cyclic AMP (cAMP)** is primarily regulated by **parathyroid hormone (PTH)**, which stimulates its excretion.
- While PTH levels can change with age, a direct and significant increase in urinary cAMP excretion is not the most consistent or specific finding representing increased **bone resorption** in older women compared to other options.
*Demineralization of bone with normal osteoid matrix*
- This finding, specifically **normal osteoid matrix** but decreased mineralization, is characteristic of **osteomalacia** (in adults) or rickets (in children).
- This condition is primarily due to **vitamin D deficiency** or impaired phosphate metabolism, not directly due to age-related bone loss in the absence of other underlying pathology.
*Activation of fibroblast growth factor receptor 3*
- **Fibroblast growth factor receptor 3 (FGFR3)** plays a significant role in **endochondral ossification** and is primarily associated with conditions like **achondroplasia** when hyperactivated.
- It does not significantly increase in activity as a normal physiological change in older women contributing to age-related bone loss.
*Urinary excretion of osteocalcin*
- **Osteocalcin** is a marker of **bone formation**, produced by **osteoblasts**.
- While bone turnover increases with age, net bone loss in older women is due to resorption exceeding formation, meaning markers of formation would not typically be *increased* compared to earlier adulthood, or at least not reflect the primary pathology of bone loss.
More Countercurrent multiplication system US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.