Concentration and dilution of urine US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Concentration and dilution of urine. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Concentration and dilution of urine US Medical PG Question 1: A 28-year-old woman presents to her primary care physician complaining of intense thirst and frequent urination for the past 2 weeks. She says that she constantly feels the urge to drink water and is also going to the bathroom to urinate frequently throughout the day and multiple times at night. She was most recently hospitalized 1 month prior to presentation following a motor vehicle accident in which she suffered severe impact to her head. The physician obtains laboratory tests, with the results shown below:
Serum:
Na+: 149 mEq/L
Cl-: 103 mEq/L
K+: 3.5 mEq/L
HCO3-: 24 mEq/L
BUN: 20 mg/dL
Glucose: 105 mg/dL
Urine Osm: 250 mOsm/kg
The patient’s condition is most likely caused by inadequate hormone secretion from which of the following locations?
- A. Adrenal cortex
- B. Anterior pituitary
- C. Preoptic nucleus of the hypothalamus
- D. Suprachiasmatic nucleus of the hypothalamus
- E. Posterior pituitary (Correct Answer)
Concentration and dilution of urine Explanation: ***Posterior pituitary***
- The patient's symptoms of **polydipsia** and **polyuria**, coupled with **hypernatremia** and **low urine osmolality**, are classic signs of **diabetes insipidus (DI)**.
- The **posterior pituitary gland** is responsible for releasing **antidiuretic hormone (ADH)**, which, when inadequately secreted (neurogenic DI), leads to these findings. The prior **head trauma** is a common cause of damage to this region.
*Adrenal cortex*
- The adrenal cortex produces **mineralocorticoids** (e.g., **aldosterone**), **glucocorticoids** (e.g., **cortisol**), and **androgens**.
- Deficiencies or excesses of these hormones lead to conditions like **Addison's disease** (adrenal insufficiency) or **Cushing's syndrome**, which have different clinical presentations than those described.
*Anterior pituitary*
- The anterior pituitary produces hormones such as **GH, TSH, ACTH, FSH, LH**, and **prolactin**.
- Dysfunction of the anterior pituitary would lead to a range of hormonal imbalances impacting growth, metabolism, and reproduction, but not directly cause diabetes insipidus.
*Preoptic nucleus of the hypothalamus*
- The **preoptic nucleus** is involved in **thermoregulation**, **sleep**, and **hypothalamic control** of reproduction.
- While part of the hypothalamus, its primary functions do not directly involve ADH synthesis or release, thereby not causing diabetes insipidus.
*Suprachiasmatic nucleus of the hypothalamus*
- The **suprachiasmatic nucleus (SCN)** is the body's primary **circadian rhythm** pacemaker.
- Damage to the SCN would disrupt the sleep-wake cycle and other circadian functions, but would not directly lead to symptoms of diabetes insipidus.
Concentration and dilution of urine US Medical PG Question 2: A 56-year-old man is seen in the hospital for a chief complaint of intense thirst and polyuria. His history is significant for recent transsphenoidal resection of a pituitary adenoma. With regard to the man's fluid balance, which of the following would be expected?
- A. Hyponatremia
- B. Increased extracellular fluid osmolarity (Correct Answer)
- C. Serum osmolarity <290 mOsm/L
- D. Elevated serum ADH
- E. Elevated blood glucose
Concentration and dilution of urine Explanation: ***Increased extracellular fluid osmolarity***
- The symptoms of intense thirst and polyuria after pituitary surgery are classic for **diabetes insipidus (DI)**, which results from insufficient **antidiuretic hormone (ADH)**.
- Lack of ADH leads to the kidneys' inability to reabsorb water, causing excessive water loss and a consequent **increase in plasma osmolality** and extracellular fluid osmolarity as water is lost disproportionately to solutes.
*Hyponatremia*
- **Hyponatremia** (low sodium) typically occurs from over-hydration or conditions causing excess ADH, such as **syndrome of inappropriate ADH (SIADH)**.
- In DI, the primary problem is water loss leading to **hypernatremia** (high sodium) and increased osmolarity.
*Serum osmolarity <290 mOsm/L*
- Normal serum osmolarity is approximately **275-295 mOsm/L**. A value less than 290 mOsm/L suggests **hypo-osmolarity**.
- In DI, the significant water loss due to lack of ADH leads to **increased serum osmolarity**, usually above 295 mOsm/L.
*Elevated serum ADH*
- **Elevated serum ADH** would lead to increased water reabsorption in the kidneys, resulting in concentrated urine and potentially hyponatremia.
- In central diabetes insipidus, the problem is a **deficiency of ADH** secretion or action, leading to low or undetectable ADH levels.
*Elevated blood glucose*
- **Elevated blood glucose** is characteristic of **diabetes mellitus**, where polyuria and polydipsia occur due to osmotic diuresis from high glucose levels.
- This patient's history of pituitary surgery and the specific presentation points to DI, which is a disorder of **water balance** not directly related to glucose metabolism.
Concentration and dilution of urine US Medical PG Question 3: A 66-year-old man with congestive heart failure presents to the emergency department complaining of worsening shortness of breath. These symptoms have worsened over the last 3 days. He has a blood pressure of 126/85 mm Hg and heart rate of 82/min. Physical examination is notable for bibasilar crackles. A chest X-ray reveals bilateral pulmonary edema. His current medications include metoprolol succinate and captopril. You wish to add an additional medication targeted towards his symptoms. Of the following, which statement is correct regarding loop diuretics?
- A. Loop diuretics can cause metabolic acidosis
- B. Loop diuretics can cause ammonia toxicity
- C. Loop diuretics can cause hyperlipidemia
- D. Loop diuretics decrease sodium, magnesium, and chloride but increase calcium
- E. Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter (Correct Answer)
Concentration and dilution of urine Explanation: ***Loop diuretics inhibit the action of the Na+/K+/Cl- cotransporter***
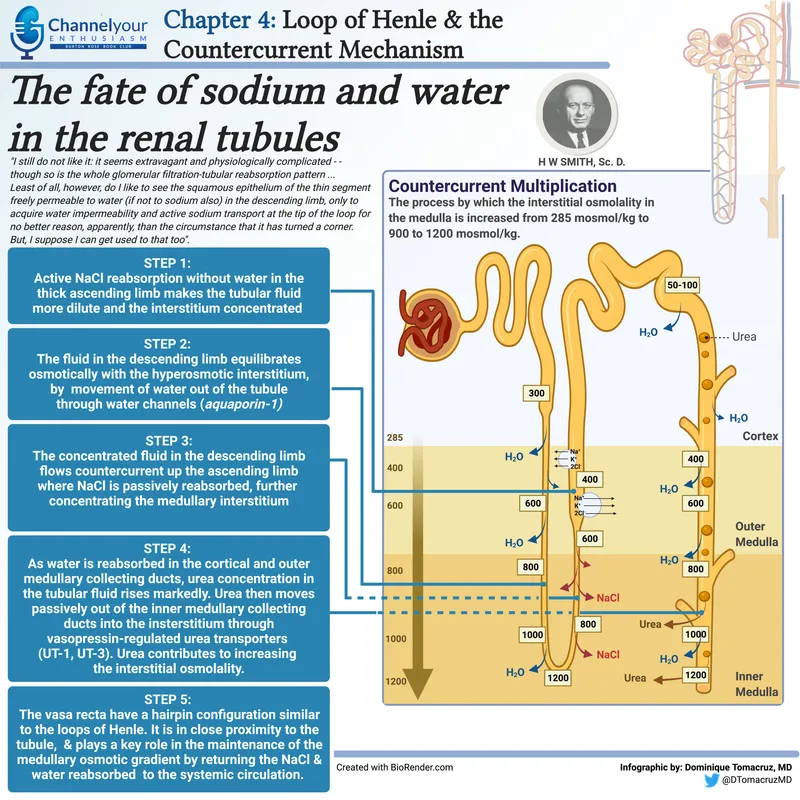
- Loop diuretics, like furosemide, directly block the **Na+/K+/2Cl- cotransporter** in the **thick ascending limb of the loop of Henle**, preventing the reabsorption of these ions.
- This inhibition leads to increased excretion of water, sodium, potassium, and chloride, which is beneficial in conditions like **pulmonary edema** due to **congestive heart failure**.
*Loop diuretics can cause metabolic acidosis*
- Loop diuretics typically cause **metabolic alkalosis**, not acidosis, because they increase the excretion of hydrogen ions and potassium, leading to a compensatory increase in bicarbonate.
- The increased delivery of sodium to the collecting duct can also stimulate potassium and hydrogen secretion, contributing to alkalosis.
*Loop diuretics can cause ammonia toxicity*
- Loop diuretics do not directly cause **ammonia toxicity**; this is more commonly associated with conditions like **hepatic encephalopathy** or certain other medications.
- Their primary mechanism of action is on renal ion transport, not ammonia metabolism.
*Loop diuretics can cause hyperlipidemia*
- While some diuretics like **thiazide diuretics** can cause mild increases in **lipid levels**, loop diuretics are not typically associated with significant **hyperlipidemia**.
- The most common metabolic side effects of loop diuretics include electrolyte imbalances.
*Loop diuretics decrease sodium, magnesium, and chloride but increase calcium*
- Loop diuretics decrease the reabsorption of **sodium**, **magnesium**, and **chloride**, leading to their increased excretion.
- They also increase **calcium excretion** (cause hypocalcemia), rather than increasing serum calcium levels, by inhibiting its reabsorption in the thick ascending limb of the loop of Henle.
Concentration and dilution of urine US Medical PG Question 4: A 39-year-old female presents with confusion. Her husband reports that she doesn't know where she is and cannot remember the date. She was recently diagnosed with small cell lung cancer. Vital signs are T 37C, HR 80, BP 120/80 mmHg, RR 14, and O2 sat 99% on room air. She is not orthostatic. Physical examination reveals moist mucous membranes and normal capillary refill. A basic metabolic profile reveals that serum sodium is 129. Regarding this patient's illness, which of the following is true?
- A. Urinary osmolarity will be < 100, and another potential cause of this disorder is excessive water drinking
- B. Urinary sodium will be > 20 and another potential cause of this disorder is renal failure
- C. Urinary sodium will be > 20 and fractional excretion of sodium will be >1%
- D. Urinary osmolarity will be > 100, and this illness will not correct with normal saline infusion (Correct Answer)
- E. Urinary sodium will be < 10, and fractional excretion of sodium will be <1%
Concentration and dilution of urine Explanation: ***Urinary osmolarity will be > 100, and this illness will not correct with normal saline infusion***
- The patient's **hyponatremia** in the context of **small cell lung cancer** (a known cause of SIADH), euvolemia (normal vital signs, moist mucous membranes, normal capillary refill), suggests **SIADH**. In SIADH, **ADH** is inappropriately elevated, leading to water retention, dilute serum, and concentrated urine, so **urinary osmolarity will be > 100 mOsm/kg** (typically > 300 mOsm/kg).
- Since SIADH involves excess free water retention due to inappropriate ADH secretion and not volume depletion, administering **normal saline (0.9%)** can actually worsen the hyponatremia by providing additional free water without addressing the underlying ADH excess. The appropriate treatment for symptomatic SIADH is **hypertonic saline (3%)**, fluid restriction, and addressing the underlying cause.
*Urinary osmolarity will be < 100, and another potential cause of this disorder is excessive water drinking*
- In SIADH, the presence of inappropriately high ADH leads to increased water reabsorption in the collecting ducts, resulting in **concentrated urine**; therefore, **urinary osmolarity will be > 100 mOsm/kg**, not < 100.
- **Urinary osmolarity < 100 mOsm/kg** with hyponatremia suggests **primary polydipsia** (excessive water drinking), where ADH is appropriately suppressed and the kidneys produce maximally dilute urine. While polydipsia can cause hyponatremia, it is not consistent with the clinical picture of SIADH, where ADH is elevated and urine is concentrated.
*Urinary sodium will be > 20 and another potential cause of this disorder is renal failure*
- In SIADH, the kidneys continue to excrete sodium due to the expanded extracellular fluid volume even in the setting of hyponatremia, leading to a **urinary sodium concentration > 20 mEq/L** ✓.
- While **renal failure** can cause hyponatremia due to impaired free water excretion, it typically presents with volume overload, elevated BUN/creatinine, and other findings not seen in this euvolemic patient with SIADH. Renal failure is not a typical "other cause" when discussing SIADH specifically.
*Urinary sodium will be > 20 and fractional excretion of sodium will be >1%*
- In SIADH, the body experiences perceived volume expansion, causing natriuresis despite low serum sodium, resulting in **urinary sodium > 20 mEq/L** ✓.
- The **fractional excretion of sodium (FENa)** is typically **>1%** (usually 1-2%) in SIADH because the kidneys appropriately excrete sodium in response to the perceived volume expansion ✓. While this option is medically accurate for SIADH, it doesn't address the critical clinical point about treatment (that normal saline is contraindicated) and the urinary osmolarity, which are more defining diagnostic and therapeutic characteristics.
*Urinary sodium will be < 10, and fractional excretion of sodium will be <1%*
- **Urinary sodium < 10 mEq/L** and **FENa < 1%** typically indicate **hypovolemic hyponatremia** with effective arterial blood volume depletion (e.g., dehydration, heart failure, cirrhosis), where the kidneys are avidly conserving sodium and water.
- This is **not consistent with SIADH**, which presents as **euvolemic hyponatremia** where the urine is concentrated (not maximally dilute) and sodium continues to be excreted, making these values incompatible with the diagnosis.
Concentration and dilution of urine US Medical PG Question 5: A 43-year-old woman is found in the hospital to have a plasma sodium concentration of 126 mg/dL. She was hospitalized after she expressed suicidal ideations and was started on a medication for major depressive disorder. Her past medical history is significant for diabetes for which she is currently taking metformin. Her blood pressure while in the hospital has been around 130/85 mmHg and she is not taking any other medications. Laboratory studies show a serum osmolality of 265 mOsm/kg. Which of the following best describes the cell bodies of the cells that are behaving abnormally in this patient?
- A. Basophils in the anterior pituitary
- B. Chromophobes in the anterior pituitary
- C. Acidophils in the anterior pituitary
- D. Located in the hypothalamus (Correct Answer)
- E. Located in the posterior pituitary
Concentration and dilution of urine Explanation: ***Located in the hypothalamus***
- The patient's **hyponatremia** (126 mg/dL) with a **low serum osmolality** (265 mOsm/kg) in the presence of depression and medication suggests **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- **ADH (vasopressin)** is synthesized in the magnocellular neurosecretory cells of the **hypothalamus** (specifically the supraoptic and paraventricular nuclei) and then transported to the posterior pituitary for release. Since the patient's condition is due to inappropriate ADH secretion, the abnormality originates in the hypothalamus where these cells are located.
*Basophils in the anterior pituitary*
- **Basophils** in the anterior pituitary produce hormones like **TSH, FSH, and LH**, which are not directly involved in the regulation of water balance and sodium levels in the context of SIADH.
- An abnormality in these cells would lead to endocrine dysfunction related to thyroid or gonadal axes, not hyponatremia.
*Chromophobes in the anterior pituitary*
- **Chromophobes** are cells in the anterior pituitary that are typically undifferentiated or degranulated, often representing cells that have released their stored hormones.
- They are not primarily responsible for the production or release of hormones involved in water balance, so an abnormality here is unlikely to cause SIADH.
*Acidophils in the anterior pituitary*
- **Acidophils** in the anterior pituitary produce **growth hormone (GH)** and **prolactin**.
- Abnormalities in these cells would lead to conditions like acromegaly or hyperprolactinemia, neither of which explains the patient's hyponatremia and low serum osmolality.
*Located in the posterior pituitary*
- While the **posterior pituitary** stores and releases **ADH**, it does not synthesize it; the cell bodies responsible for ADH production are in the hypothalamus.
- Therefore, the primary abnormal cells in SIADH are the ones synthesizing ADH in the hypothalamus, not merely storing it in the posterior pituitary.
Concentration and dilution of urine US Medical PG Question 6: A 52-year-old woman presents to her primary care physician complaining of 3 weeks of persistent thirst despite consumption of increased quantities of water. She also admits that she has had increased frequency of urination during the same time period. A basic metabolic panel is performed which reveals mild hypernatremia and a normal glucose level. Urine electrolytes are then obtained which shows a very low urine osmolality that does not correct when a water deprivation test is performed. Blood tests reveal an undetectable level of antidiuretic hormone (ADH). Based on this information, what is the most likely cause of this patient's symptoms?
- A. Diabetes mellitus
- B. Central diabetes insipidus (Correct Answer)
- C. Primary polydipsia
- D. Surreptitious diuretic use
- E. Nephrogenic diabetes insipidus
Concentration and dilution of urine Explanation: ***Central diabetes insipidus***
- The patient presents with **polyuria**, **polydipsia**, **hypernatremia**, and a **low urine osmolality** that does not correct with a **water deprivation test**.
- An **undetectable ADH level** confirms a defect in ADH production or release from the pituitary, which is characteristic of central diabetes insipidus.
*Diabetes mellitus*
- This condition is characterized by **hyperglycemia**, which is ruled out by the **normal glucose level** in the basic metabolic panel.
- While it causes polyuria and polydipsia, the underlying mechanism is **osmotic diuresis due to glucose**, not a defect in ADH or renal response to ADH.
*Primary polydipsia*
- In primary polydipsia, patients consume excessive amounts of water, leading to **dilutional hyponatremia** rather than hypernatremia.
- The **ADH levels would be appropriately suppressed** in a patient with primary polydipsia, not undetectable.
*Surreptitious diuretic use*
- Diuretic use would typically lead to **low blood pressure**, **electrolyte imbalances** (e.g., hypokalemia), and a **high urine sodium concentration**, none of which are explicitly mentioned here.
- It would also not result in an **undetectable ADH level** in the absence of an underlying ADH deficiency.
*Nephrogenic diabetes insipidus*
- This condition involves the **kidneys' inability to respond to ADH**, leading to similar symptoms of polyuria and polydipsia with low urine osmolality.
- However, in nephrogenic diabetes insipidus, the **ADH levels would be high or normal** as the pituitary is producing ADH, but the kidneys are not responding.
Concentration and dilution of urine US Medical PG Question 7: A 78-year-old male with history of coronary artery disease, status post coronary stent placement currently on aspirin and clopidogrel was found down in his bathroom by his wife. His GCS score was 3 and an accurate physical exam is limited. A stat non-contrast CT scan of his brain demonstrated a large right parietal intracranial hemorrhage with surrounding edema. He was promptly transferred to the intensive care unit (ICU) for monitoring. Over the next day, his mental status continues to worsen but repeat CT scan shows no new bleeding. In addition, the patient’s urinary output has been >200 cc/hr over the last several hours and increasing. His temperature is 99.0 deg F (37.2 deg C), blood pressure is 125/72 mmHg, pulse is 87/min, and respirations are 13/min. Which of the following values would most likely correspond to the patient’s urine specific gravity, urine osmolality, plasma osmolality, and serum sodium?
- A. Low, High, High, High
- B. Low, Low, High, High (Correct Answer)
- C. High, High, Low, Low
- D. Low, Low, High, Low
- E. High, Low, Low, High
Concentration and dilution of urine Explanation: ***Low, Low, High, High***
- This patient's presentation, particularly the **large intracranial hemorrhage**, worsening mental status despite no new bleeding, and especially the **high urinary output (>200 cc/hr)**, is classic for **diabetes insipidus (DI)**, often neurogenic DI, due to damage to the posterior pituitary or hypothalamus.
- In DI, there is a deficiency of **ADH (vasopressin)**, leading to the kidneys' inability to reabsorb water. This results in the excretion of large volumes of **dilute urine** (low urine specific gravity, low urine osmolality) and concentration of the plasma (high plasma osmolality and hypernatremia, which means high serum sodium).
*Low, High, High, High*
- This pattern would indicate concentrated urine alongside concentrated plasma and high sodium, which contradicts the presence of **polyuria** and the underlying pathology of **diabetes insipidus (DI)**.
- High urine osmolality and specific gravity would suggest intact ADH function and water reabsorption in the kidneys, which is not what occurs in DI.
*High, High, Low, Low*
- This profile describes a state of **concentrated urine** but **dilute plasma** and **hyponatremia**, which is characteristic of the **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- SIADH is the opposite of diabetes insipidus, involving excessive ADH leading to water retention, not excessive water excretion.
*Low, Low, High, Low*
- While **low urine specific gravity** and **low urine osmolality** are consistent with diabetes insipidus, a **low serum sodium** (hyponatremia) is not.
- In diabetes insipidus, the loss of free water typically leads to **hypernatremia** as the body becomes dehydrated.
*High, Low, Low, High*
- This combination is inconsistent with any common clinical scenario. A **high urine specific gravity** with a **low urine osmolality** is contradictory, as specific gravity is a measure of urine concentration, which correlates with osmolality.
- Furthermore, a **low plasma osmolality** with a **high serum sodium** is physiologically improbable.
Concentration and dilution of urine US Medical PG Question 8: An 81-year-old man presents to his primary care physician for his yearly exam. His past medical history is significant for osteopenia, nephrolithiasis, and hypertension. His family history is significant for relatives who had early onset kidney failure. He takes occasional acetaminophen and supplemental calcium/vitamin D. He is physically active with a normal body mass index (BMI) and has no current concerns. Review of his laboratory results today were compared with those from 15 years ago with the following findings:
Results today:
Serum creatinine concentration: 1.1 mg/dL
Urine creatinine concentration: 100 mg/dL
Urine volume: 1000 mL/day
Results 15 years ago:
Serum creatinine concentration: 1.1 mg/dL
Urine creatinine concentration: 120 mg/dL
Urine volume: 1000 mL/day
Which is the most likely cause of these changes in his creatinine clearance?
- A. Renovascular disease
- B. Nephrolithiasis
- C. Normal aging (Correct Answer)
- D. Polycystic kidney disease
- E. Benign prostatic hyperplasia
Concentration and dilution of urine Explanation: ***Normal aging***
- As individuals **age**, there is a natural decline in **glomerular filtration rate (GFR)** due to nephron loss and sclerotic changes, even with a stable serum creatinine.
- The drop in **urine creatinine concentration** over 15 years, combined with a stable serum creatinine and urine volume, indicates a reduction in muscle mass and creatinine production, which is typical for an 81-year-old, thereby masking a decline in GFR.
*Renovascular disease*
- This typically causes a **drop in GFR** or **acute kidney injury**, often with a **rise in serum creatinine**.
- There is no increase in serum creatinine in this patient, and the presentation does not suggest **flash pulmonary edema** or **uncontrolled hypertension**.
*Nephrolithiasis*
- While the patient has a history of nephrolithiasis, it typically causes **acute, severe flank pain** or **obstructive kidney injury** when significant.
- There are no symptoms of acute obstruction, nor is there a significant increase in serum creatinine that would suggest a new stone causing obstruction.
*Polycystic kidney disease*
- This is a **genetic disorder** causing multiple cysts in the kidneys, leading to progressive kidney failure, often with a **family history of early-onset kidney failure**.
- While the family history is relevant, there are **no symptoms or physical exam findings** suggestive of PKD, such as kidney enlargement or hematuria.
*Benign prostatic hyperplasia*
- BPH can cause **obstructive uropathy** and a **rise in serum creatinine**, particularly if it leads to urinary retention.
- The patient has a normal urine volume and no symptoms of urinary obstruction such as **hesitancy, weak stream, or nocturia**.
Concentration and dilution of urine US Medical PG Question 9: A 23-year-old male presents with complaints of polydipsia and frequent, large-volume urination. Laboratory testing does not demonstrate any evidence of diabetes; however, a reduced urine osmolality of 120 mOsm/L is measured. Which of the following findings on a desmopressin test would be most consistent with a diagnosis of central diabetes insipidus?
- A. Reduction in urine osmolality to 60 mOsm/L following desmopressin administration
- B. No detectable change in urine osmolality following desmopressin administration
- C. Increase in urine osmolality to 400 mOsm/L following desmopressin administration (Correct Answer)
- D. Increase in urine osmolality to 130 mOsm/L following desmopressin administration
- E. Reduction in urine osmolality to 110 mOsm/L following desmopressin administration
Concentration and dilution of urine Explanation: ***Increase in urine osmolality to 400 mOsm/L following desmopressin administration***
- In **central diabetes insipidus**, the kidneys are still able to respond to **vasopressin** (ADH), but the body doesn't produce enough of it. Therefore, administering **desmopressin** (a synthetic ADH analog) will significantly increase **urine osmolality** as the kidneys resorb more water.
- A significant increase, such as from 120 mOsm/L to 400 mOsm/L, indicates that the underlying problem is a lack of ADH production, characteristic of **central diabetes insipidus**.
*Increase in urine osmolality to 130 mOsm/L following desmopressin administration*
- A minor increase from 120 mOsm/L to 130 mOsm/L following desmopressin administration would suggest that the kidneys are largely **unresponsive** to ADH, which is characteristic of **nephrogenic diabetes insipidus**.
- In central diabetes insipidus, a more substantial increase in **urine osmolality** is expected, as the kidney's ability to respond to ADH is intact.
*Reduction in urine osmolality to 60 mOsm/L following desmopressin administration*
- A reduction in **urine osmolality** after desmopressin administration would be an unexpected and contradictory finding.
- Desmopressin is meant to increase water reabsorption, leading to concentrated urine, not more dilute urine.
*Reduction in urine osmolality to 110 mOsm/L following desmopressin administration*
- Similar to the previous option, a reduction in **urine osmolality** following desmopressin administration is clinically inconsistent with the expected action of ADH.
- This result would not align with either central nor nephrogenic diabetes insipidus scenarios, where an increase or no change, respectively, would be anticipated.
*No detectable change in urine osmolality following desmopressin administration*
- If there is no detectable change or only a very small change in **urine osmolality** after desmopressin administration, it suggests that the kidneys are not responding to ADH.
- This would be consistent with **nephrogenic diabetes insipidus**, where the kidneys themselves are resistant to ADH, rather than central DI, where the problem is ADH deficiency.
Concentration and dilution of urine US Medical PG Question 10: An investigator studying hormone synthesis and transport uses immunocytochemical techniques to localize a carrier protein in the central nervous system of an experimental animal. The investigator finds that this protein is synthesized together with a specific hormone from a composite precursor. The protein is involved in the transport of the hormone from the supraoptic and paraventricular nuclei to its destination. The hormone transported by these carrier proteins is most likely responsible for which of the following functions?
- A. Stimulation of thyroglobulin cleavage
- B. Upregulation of renal aquaporin-2 channels (Correct Answer)
- C. Hyperplasia of the adrenal zona fasciculata
- D. Increased insulin-like growth factor 1 production
- E. Maturation of primordial germ cells
Concentration and dilution of urine Explanation: ***Upregulation of renal aquaporin-2 channels***
- The description of a hormone synthesized in the **supraoptic** and **paraventricular nuclei** and transported by a carrier protein refers to **antidiuretic hormone (ADH)**, also known as vasopressin.
- ADH's primary function in the kidney is to **increase water reabsorption** by upregulating **aquaporin-2 channels** in the principal cells of the collecting ducts.
*Stimulation of thyroglobulin cleavage*
- **Thyroglobulin cleavage** and subsequent release of thyroid hormones (T3, T4) are stimulated by **thyroid-stimulating hormone (TSH)**, which is produced by the anterior pituitary, not the hypothalamus.
- The described origin in the supraoptic and paraventricular nuclei is inconsistent with TSH.
*Hyperplasia of the adrenal zona fasciculata*
- **Adrenocorticotropic hormone (ACTH)** from the anterior pituitary stimulates the adrenal cortex, including the zona fasciculata, to produce cortisol.
- The hormone described here originates in the hypothalamus and is transported to the posterior pituitary, not stimulating adrenal hyperplasia.
*Increased insulin-like growth factor 1 production*
- **Insulin-like growth factor 1 (IGF-1)** production is stimulated primarily by **growth hormone (GH)**, which is secreted by the anterior pituitary.
- This function is not associated with hormones produced in the supraoptic and paraventricular nuclei.
*Maturation of primordial germ cells*
- The maturation of **primordial germ cells** is regulated by **gonadotropins (FSH and LH)**, which are secreted by the anterior pituitary, and sex steroids.
- This process is not directly controlled by hormones originating from the supraoptic and paraventricular nuclei.
More Concentration and dilution of urine US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.