RAAS in volume regulation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for RAAS in volume regulation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
RAAS in volume regulation US Medical PG Question 1: A 28-year-old woman presents to her primary care physician complaining of intense thirst and frequent urination for the past 2 weeks. She says that she constantly feels the urge to drink water and is also going to the bathroom to urinate frequently throughout the day and multiple times at night. She was most recently hospitalized 1 month prior to presentation following a motor vehicle accident in which she suffered severe impact to her head. The physician obtains laboratory tests, with the results shown below:
Serum:
Na+: 149 mEq/L
Cl-: 103 mEq/L
K+: 3.5 mEq/L
HCO3-: 24 mEq/L
BUN: 20 mg/dL
Glucose: 105 mg/dL
Urine Osm: 250 mOsm/kg
The patient’s condition is most likely caused by inadequate hormone secretion from which of the following locations?
- A. Adrenal cortex
- B. Anterior pituitary
- C. Preoptic nucleus of the hypothalamus
- D. Suprachiasmatic nucleus of the hypothalamus
- E. Posterior pituitary (Correct Answer)
RAAS in volume regulation Explanation: ***Posterior pituitary***
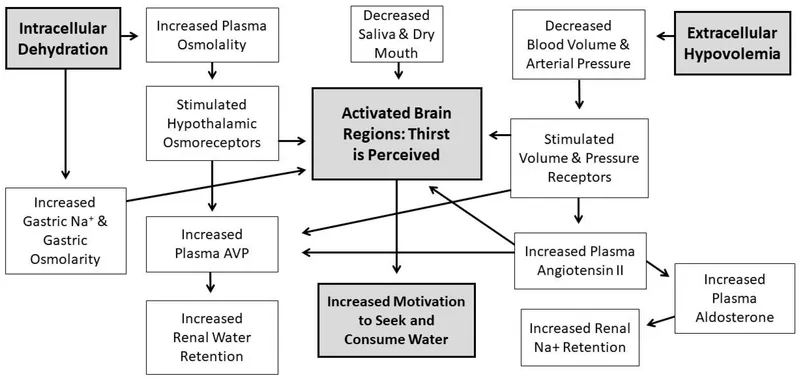
- The patient's symptoms of **polydipsia** and **polyuria**, coupled with **hypernatremia** and **low urine osmolality**, are classic signs of **diabetes insipidus (DI)**.
- The **posterior pituitary gland** is responsible for releasing **antidiuretic hormone (ADH)**, which, when inadequately secreted (neurogenic DI), leads to these findings. The prior **head trauma** is a common cause of damage to this region.
*Adrenal cortex*
- The adrenal cortex produces **mineralocorticoids** (e.g., **aldosterone**), **glucocorticoids** (e.g., **cortisol**), and **androgens**.
- Deficiencies or excesses of these hormones lead to conditions like **Addison's disease** (adrenal insufficiency) or **Cushing's syndrome**, which have different clinical presentations than those described.
*Anterior pituitary*
- The anterior pituitary produces hormones such as **GH, TSH, ACTH, FSH, LH**, and **prolactin**.
- Dysfunction of the anterior pituitary would lead to a range of hormonal imbalances impacting growth, metabolism, and reproduction, but not directly cause diabetes insipidus.
*Preoptic nucleus of the hypothalamus*
- The **preoptic nucleus** is involved in **thermoregulation**, **sleep**, and **hypothalamic control** of reproduction.
- While part of the hypothalamus, its primary functions do not directly involve ADH synthesis or release, thereby not causing diabetes insipidus.
*Suprachiasmatic nucleus of the hypothalamus*
- The **suprachiasmatic nucleus (SCN)** is the body's primary **circadian rhythm** pacemaker.
- Damage to the SCN would disrupt the sleep-wake cycle and other circadian functions, but would not directly lead to symptoms of diabetes insipidus.
RAAS in volume regulation US Medical PG Question 2: What is the primary mechanism for maintaining constant cerebral blood flow despite changes in systemic blood pressure?
- A. Endothelial factors
- B. Baroreceptor reflex
- C. Myogenic autoregulation (Correct Answer)
- D. Metabolic control
RAAS in volume regulation Explanation: ***Myogenic autoregulation***
- **Myogenic autoregulation** is the intrinsic ability of vascular smooth muscle to contract when stretched by increased blood pressure, thereby maintaining a constant cerebral blood flow.
- This mechanism operates within a specific range of mean arterial pressures (typically **60-150 mmHg**) to prevent both hypoperfusion and hyperperfusion of the brain.
*Endothelial factors*
- Endothelial cells release various vasoactive substances like **nitric oxide** and **endothelin**, which influence vascular tone.
- While important for local blood flow regulation, these factors play a secondary role to myogenic autoregulation in maintaining constant cerebral blood flow against systemic pressure changes.
*Baroreceptor reflex*
- The **baroreceptor reflex** primarily controls systemic blood pressure by regulating heart rate and peripheral vascular resistance.
- It does not directly regulate cerebral blood flow stability in response to systemic pressure changes; its main role is to stabilize the overall systemic arterial pressure.
*Metabolic control*
- **Metabolic control** regulates cerebral blood flow in response to the brain's metabolic demands, primarily by sensing local concentrations of **CO2**, **pH**, and **oxygen**.
- While essential for matching blood supply to neuronal activity, it is not the primary mechanism for maintaining cerebral blood flow despite changes in systemic blood pressure.
RAAS in volume regulation US Medical PG Question 3: A 47-year-old man with bipolar I disorder and hypertension comes to the physician because of a 2-week history of increased thirst, urinary frequency, and sleep disturbance. He says that he now drinks up to 30 cups of water daily. He has smoked 2 packs of cigarettes daily for the past 20 years. Examination shows decreased skin turgor. Serum studies show a sodium concentration of 149 mEq/L, a potassium concentration of 4.1 mEq/L, and an elevated antidiuretic hormone concentration. His urine osmolality is 121 mOsm/kg H2O. Which of the following is the most likely explanation for these findings?
- A. Tumor in the adrenal cortex
- B. Adverse effect of a medication (Correct Answer)
- C. Paraneoplastic production of a hormone
- D. Polydipsia caused by acute psychosis
- E. Tumor of the pituitary gland
RAAS in volume regulation Explanation: ***Adverse effect of a medication***
- The patient's presentation of **polyuria**, **polydipsia**, **hypernatremia**, and **elevated ADH** with **low urine osmolality** is consistent with **nephrogenic diabetes insipidus**.
- **Lithium**, a common treatment for bipolar I disorder, is a well-known cause of **nephrogenic diabetes insipidus** by interfering with the renal collecting duct's response to ADH.
*Tumor in the adrenal cortex*
- An adrenal cortical tumor would typically lead to conditions like **Cushing's syndrome** ( excess cortisol) or **Conn's syndrome** (excess aldosterone), causing **hypokalemia** and **hypertension**, but not primarily hypernatremia with low urine osmolality.
- While it can affect fluid balance, it does not directly cause the classic presentation of **diabetes insipidus** with elevated ADH and low urine osmolality.
*Paraneoplastic production of a hormone*
- Paraneoplastic syndromes can cause various endocrine abnormalities, but paraneoplastic production of a hormone leading to **nephrogenic diabetes insipidus** with high ADH and low urine osmolality is highly unlikely.
- More common paraneoplastic syndromes affecting water balance involve inappropriate ADH secretion (SIADH), leading to **hyponatremia**, not hypernatremia.
*Polydipsia caused by acute psychosis*
- Primary polydipsia typically results in **hyponatremia** due to excessive water intake diluting serum sodium, especially if renal concentrating mechanisms are intact. The patient has **hypernatremia**.
- While patients with psychiatric conditions can exhibit **primary polydipsia**, the body usually compensates by suppressing ADH and excreting dilute urine; an **elevated ADH** makes this diagnosis less likely.
*Tumor of the pituitary gland*
- A pituitary tumor could cause **central diabetes insipidus** if it interfered with ADH production or release, but this would lead to a *low* or *inappropriately normal* ADH level, not an **elevated ADH** level.
- An elevated ADH with nephrogenic diabetes insipidus indicates the kidneys are not responding to ADH, rather than a problem with ADH production.
RAAS in volume regulation US Medical PG Question 4: A 32-year-old man presents with hypertension that has been difficult to control with medications. His symptoms include fatigue, frequent waking at night for voiding, and pins and needles in the legs. His symptoms started 2 years ago. Family history is positive for hypertension in his mother. His blood pressure is 160/100 mm Hg in the right arm and 165/107 mm Hg in the left arm, pulse is 85/min, and temperature is 36.5°C (97.7°F). Physical examination reveals global hyporeflexia and muscular weakness. Lab studies are shown:
Serum sodium 147 mEq/L
Serum creatinine 0.7 mg/dL
Serum potassium 2.3 mEq/L
Serum bicarbonate 34 mEq/L
Plasma renin activity low
Which of the following is the most likely diagnosis?
- A. Renal artery stenosis
- B. Coarctation of aorta
- C. Cushing syndrome
- D. Primary aldosteronism (Correct Answer)
- E. Essential hypertension
RAAS in volume regulation Explanation: ***Primary aldosteronism***
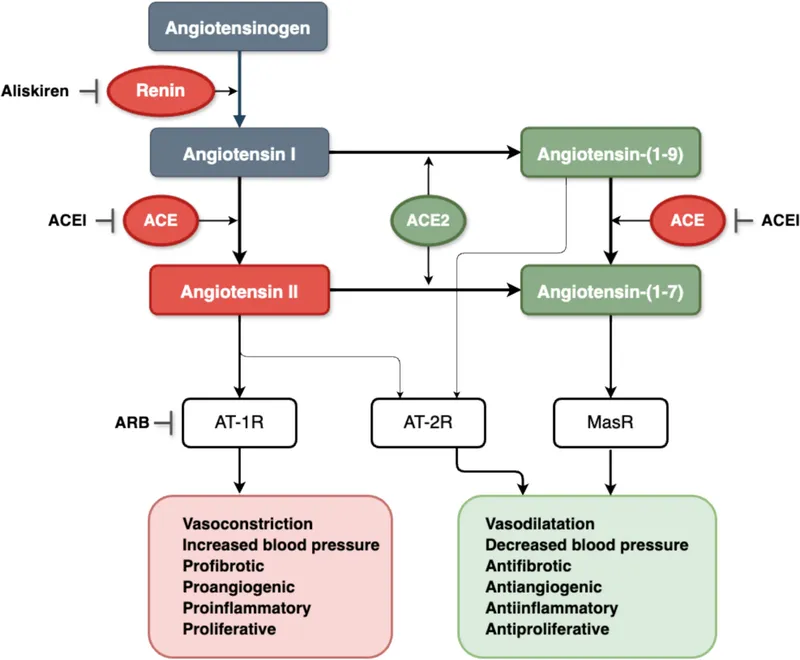
- The patient presents with **resistant hypertension**, **hypokalemia** (2.3 mEq/L), **metabolic alkalosis** (bicarbonate 34 mEq/L), and **low plasma renin activity**, which are classic features of primary aldosteronism.
- Symptoms like **fatigue**, **nocturia**, and **paresthesias** (pins and needles) in the legs are consistent with severe hypokalemia, directly resulting from excessive aldosterone secretion.
*Renal artery stenosis*
- This condition typically causes **secondary hypertension** with **elevated renin levels** due to decreased renal perfusion, which contradicts the low plasma renin activity seen in this patient.
- While it can cause hypokalemia because of increased renin-angiotensin-aldosterone system activation, the **primary driver** in this case, based on low renin, points away from renal artery stenosis.
*Coarctation of aorta*
- Characterized by **differential blood pressures** between the upper and lower extremities and sometimes between the arms, and a **systolic murmur** that is often present.
- It does not typically present with severe **hypokalemia** or metabolic alkalosis or the low plasma renin activity observed in this patient.
*Cushing syndrome*
- This syndrome is caused by **excessive cortisol** and can lead to hypertension and hypokalemia, but it is also associated with distinct clinical features like **central obesity**, buffalo hump, moon facies, and proximal muscle weakness, which are not described.
- While it can cause similar electrolyte imbalances, the lack of classic Cushingoid features makes it less likely, and the specific **low plasma renin** points more strongly to aldosterone excess.
*Essential hypertension*
- This is a diagnosis of exclusion, typically presenting without a clear secondary cause and with **normal electrolyte levels**.
- The presence of severe **hypokalemia**, **metabolic alkalosis**, and **low plasma renin activity** indicates a secondary cause, ruling out essential hypertension.
RAAS in volume regulation US Medical PG Question 5: Activation of the renin-angiotensin-aldosterone system yields a significant physiological effect on renal blood flow and filtration. Which of the following is most likely to occur in response to increased levels of Angiotensin-II?
- A. Decreased renal plasma flow, decreased filtration fraction
- B. Decreased renal plasma flow, increased glomerular capillary oncotic pressure
- C. Increased renal plasma flow, decreased filtration fraction
- D. Increased renal plasma flow, increased filtration fraction
- E. Decreased renal plasma flow, increased filtration fraction (Correct Answer)
RAAS in volume regulation Explanation: ***Decreased renal plasma flow, increased filtration fraction***
- **Angiotensin II** causes **efferent arteriolar constriction**, which reduces blood flow leaving the glomerulus, thereby **decreasing renal plasma flow**.
- This efferent constriction also increases **glomerular hydrostatic pressure** and reduces plasma flow distal to the glomerulus, leading to a **higher filtration fraction** (GFR/RPF).
*Decreased renal plasma flow, decreased filtration fraction*
- While **renal plasma flow decreases**, a **decreased filtration fraction** would imply that either GFR decreases disproportionately more than RPF or GFR does not increase despite the RPF reduction, which is not the typical response to **angiotensin II** due to its predominant effect on the **efferent arteriole**.
*Decreased renal plasma flow, increased glomerular capillary oncotic pressure*
- **Increased glomerular capillary oncotic pressure** is a consequence of increased filtration fraction, as more fluid is filtered out, leaving behind a more concentrated plasma. This option includes a correct element (decreased RPF) but pairs it with a less direct and defining outcome of acute Angiotensin II action as the primary physiological effect.
*Increased renal plasma flow, decreased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, predominantly of the efferent arteriole, which by definition would **decrease renal plasma flow**, not increase it.
- A **decreased filtration fraction** would be inconsistent with efferent arteriolar constriction which typically raises GFR relative to RPF.
*Increased renal plasma flow, increased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, leading to a **decrease in renal plasma flow**, not an increase.
- While **filtration fraction is increased**, the initial premise of increased renal plasma flow is incorrect.
RAAS in volume regulation US Medical PG Question 6: A 57-year-old otherwise healthy male presents to his primary care physician for a check-up. He has no complaints. His blood pressure at the previous visit was 160/95. The patient did not wish to be on any medications and at the time attempted to manage his blood pressure with diet and exercise. On repeat measurement of blood pressure today, the reading is 163/92. His physician decides to prescribe a medication which the patient agrees to take. The patient calls his physician 6 days later complaining of a persistent cough, but otherwise states that his BP was measured as 145/85 at a local pharmacy. Which of the following is a contraindication to this medication?
- A. Congestive heart failure
- B. Black race
- C. Bilateral renal artery stenosis (Correct Answer)
- D. Chronic obstructive pulmonary disease
- E. Gout
RAAS in volume regulation Explanation: ***Bilateral renal artery stenosis***
- The patient's developing **cough** after starting a new antihypertensive suggests he was likely prescribed an **ACE inhibitor**.
- **Bilateral renal artery stenosis** is a strong contraindication for ACE inhibitors due to the risk of precipitating **acute kidney injury**, as these medications rely on efferent arteriolar vasodilation to maintain renal perfusion when there's reduced afferent flow.
*Congestive heart failure*
- **ACE inhibitors** are often a **first-line treatment** for heart failure due to their ability to improve cardiac remodeling and reduce mortality.
- They are used to prevent ventricular remodeling and reduce afterload, making this an indication, not a contraindication.
*Black race*
- While ACE inhibitors may be **less effective as monotherapy** in black patients, they are not contraindicated and can be effectively used in combination with other antihypertensives, such as **thiazide diuretics** or **calcium channel blockers**.
- **African Americans** often respond better to calcium channel blockers and diuretics for hypertension but ACE inhibitors are not absolutely contraindicated.
*Chronic obstructive pulmonary disease*
- **ACE inhibitors** are **not contraindicated** in COPD, as they do not affect bronchial smooth muscle tone.
- **Beta-blockers**, not ACE inhibitors, are typically avoided or used with caution in patients with reactive airway diseases like asthma or severe COPD.
*Gout*
- **ACE inhibitors** do not significantly impact **uric acid levels** and are generally safe for use in patients with gout.
- In contrast, **thiazide diuretics** can increase uric acid levels and worsen gout, but this is not the medication indicated by the patient's cough.
RAAS in volume regulation US Medical PG Question 7: A 63-year-old woman presents to your outpatient clinic complaining of headaches, blurred vision, and fatigue. She has a blood pressure of 171/91 mm Hg and heart rate of 84/min. Physical examination is unremarkable. Her lab results include K+ of 3.1mEq/L and a serum pH of 7.51. Of the following, which is the most likely diagnosis for this patient?
- A. Pheochromocytoma
- B. Renal artery stenosis
- C. Cushing’s syndrome
- D. Primary hyperaldosteronism (Conn’s syndrome) (Correct Answer)
- E. Addison’s disease
RAAS in volume regulation Explanation: ***Primary hyperaldosteronism (Conn’s syndrome)***
- The combination of **hypertension**, **hypokalemia (K+ 3.1 mEq/L)**, and **metabolic alkalosis (pH 7.51)** is highly characteristic of primary hyperaldosteronism.
- Excess aldosterone leads to increased sodium reabsorption and potassium/hydrogen ion excretion, causing these electrolyte imbalances.
*Pheochromocytoma*
- This condition involves episodic **hypertension**, palpitations, sweating, and anxiety due to catecholamine excess.
- While hypertension is present, the absence of paroxysmal symptoms and the specific electrolyte abnormalities (hypokalemia, alkalosis) make it less likely.
*Renal artery stenosis*
- This can cause **secondary hypertension** and occasionally hypokalemia, but it typically presents with **renal bruits**, and the metabolic alkalosis is not a direct or prominent feature.
- The elevated renin-angiotensin-aldosterone axis would lead to secondary hyperaldosteronism, but primary hyperaldosteronism is suggested by the overall clinical picture.
*Cushing’s syndrome*
- Cushing's syndrome is characterized by **central obesity**, striae, moon facies, and **hyperglycemia**, among other symptoms.
- While hypertension and hypokalemia can occur in severe cases, the predominant clinical features are not aligned with this patient's presentation.
*Addison’s disease*
- This condition is characterized by **adrenal insufficiency**, leading to hypoglycemia, **hyponatremia**, **hyperkalemia**, and **hypotension**.
- The patient's hypertension and hypokalemia directly contradict the typical presentation of Addison’s disease.
RAAS in volume regulation US Medical PG Question 8: A 48-year-old woman comes to the physician for a follow-up examination. At her visit 1 month ago, her glomerular filtration rate (GFR) was 100 mL/min/1.73 m2 and her renal plasma flow (RPF) was 588 mL/min. Today, her RPF is 540 mL/min and her filtration fraction (FF) is 0.2. After her previous appointment, this patient was most likely started on a drug that has which of the following effects?
- A. Inhibition of the renal Na-K-Cl cotransporter
- B. Constriction of the afferent arteriole
- C. Relaxation of urinary smooth muscle
- D. Constriction of the efferent arteriole (Correct Answer)
- E. Inhibition of vasopressin
RAAS in volume regulation Explanation: ***Constriction of the efferent arteriole***
- The previous GFR was 100 mL/min and RPF was 588 mL/min. For the follow-up, RPF is 540 mL/min and FF is 0.2. The new GFR can be calculated as FF × RPF = 0.2 × 540 = **108 mL/min**.
- The patient shows **increased GFR** (100→108 mL/min) with **decreased RPF** (588→540 mL/min), resulting in an **increased filtration fraction**.
- Medications that **constrict the efferent arteriole**, such as **NSAIDs**, produce this pattern by blocking prostaglandin synthesis. Prostaglandins normally cause vasodilation (predominantly of the afferent arteriole). When blocked, there is relatively more **efferent arteriolar constriction**, which increases glomerular hydrostatic pressure, thereby **increasing GFR while reducing overall RPF**.
*Inhibition of the renal Na-K-Cl cotransporter*
- This effect describes **loop diuretics** (e.g., furosemide), which increase sodium excretion and water diuresis.
- Loop diuretics typically cause a **decrease in GFR** due to reduced fluid volume and lower filtration pressure, which contradicts the slight increase in GFR observed.
*Constriction of the afferent arteriole*
- **Afferent arteriole constriction** (e.g., by NSAIDs in high doses or norepinephrine) would decrease blood flow into the glomerulus, leading to a **decrease in both RPF and GFR**.
- While RPF decreased in this case, GFR actually increased, making this option incorrect.
*Relaxation of urinary smooth muscle*
- Relaxation of urinary smooth muscle is characteristic of drugs like **alpha-blockers** (e.g., tamsulosin) or antimuscarinics used for conditions like benign prostatic hyperplasia or overactive bladder.
- This effect primarily impacts urine flow out of the bladder and does **not directly affect GFR or RPF** in the way described.
*Inhibition of vasopressin*
- Vasopressin (ADH) inhibition leads to **increased water excretion** and is seen with drugs like **vasopressin receptor antagonists** (vaptans) or ethanol.
- While it affects fluid balance, it typically causes a **decrease in GFR** due to hypovolemia and has no direct mechanism to increase GFR with decreased RPF as observed.
RAAS in volume regulation US Medical PG Question 9: A 32-year-old female presents to her obstetrician 3 weeks postpartum for failure to lactate. Of note, she has been unable to tolerate cold environments since the birth of her child. Review of systems is positive for fatigue, lightheadedness, and a 3-pound weight gain over the last 3 weeks. Her delivery was complicated by placenta accreta with postpartum blood loss. Her newborn infant is doing well on formula. She denies any personal or family history of thyroid disease. Physical exam is overall unremarkable. On a panel of hormone testing, which of the following levels is most likely to be normal in this patient?
- A. Thyroid hormone
- B. Cortisol
- C. Luteinizing hormone
- D. Antidiuretic hormone (Correct Answer)
- E. Aldosterone
RAAS in volume regulation Explanation: ***Antidiuretic hormone***
- This patient is presenting with symptoms consistent with **Sheehan syndrome**, which is postpartum pituitary necrosis due to severe hemorrhage and hypovolemic shock.
- Sheehan syndrome **primarily affects the anterior pituitary**, where most pituitary hormones are produced.
- **Antidiuretic hormone (ADH)** is synthesized by the **hypothalamus** and stored/released by the **posterior pituitary**, which is typically **spared** in Sheehan syndrome due to its separate blood supply.
- Therefore, **ADH levels would be normal** in this patient, making this the correct answer.
*Aldosterone*
- The **renin-angiotensin-aldosterone system (RAAS)** is regulated independently by the kidneys and is preserved in pituitary disorders.
- Aldosterone levels would also likely be **normal** in this patient.
- However, ADH is the better answer as it specifically demonstrates the anatomical distinction between anterior and posterior pituitary function.
*Thyroid hormone*
- The **anterior pituitary** fails to produce **thyroid-stimulating hormone (TSH)** in Sheehan syndrome, leading to secondary hypothyroidism.
- This results in **low thyroid hormone levels**.
- Her symptoms of **cold intolerance**, **fatigue**, and **weight gain** are classic manifestations of hypothyroidism.
*Cortisol*
- The anterior pituitary produces **adrenocorticotropic hormone (ACTH)**, which stimulates cortisol release from the adrenal glands.
- In Sheehan syndrome, failure of ACTH production leads to **secondary adrenal insufficiency** with **low cortisol levels**.
- This contributes to her **fatigue** and **lightheadedness**.
*Luteinizing hormone*
- The anterior pituitary produces **luteinizing hormone (LH)**, which is crucial for ovarian function and ovulation.
- The patient's **failure to lactate** is due to **prolactin deficiency** (another anterior pituitary hormone), not LH deficiency.
- Lack of LH and other gonadotropins would contribute to amenorrhea and loss of reproductive function that often accompany Sheehan syndrome.
RAAS in volume regulation US Medical PG Question 10: An investigator studying hormone synthesis and transport uses immunocytochemical techniques to localize a carrier protein in the central nervous system of an experimental animal. The investigator finds that this protein is synthesized together with a specific hormone from a composite precursor. The protein is involved in the transport of the hormone from the supraoptic and paraventricular nuclei to its destination. The hormone transported by these carrier proteins is most likely responsible for which of the following functions?
- A. Stimulation of thyroglobulin cleavage
- B. Upregulation of renal aquaporin-2 channels (Correct Answer)
- C. Hyperplasia of the adrenal zona fasciculata
- D. Increased insulin-like growth factor 1 production
- E. Maturation of primordial germ cells
RAAS in volume regulation Explanation: ***Upregulation of renal aquaporin-2 channels***
- The description of a hormone synthesized in the **supraoptic** and **paraventricular nuclei** and transported by a carrier protein refers to **antidiuretic hormone (ADH)**, also known as vasopressin.
- ADH's primary function in the kidney is to **increase water reabsorption** by upregulating **aquaporin-2 channels** in the principal cells of the collecting ducts.
*Stimulation of thyroglobulin cleavage*
- **Thyroglobulin cleavage** and subsequent release of thyroid hormones (T3, T4) are stimulated by **thyroid-stimulating hormone (TSH)**, which is produced by the anterior pituitary, not the hypothalamus.
- The described origin in the supraoptic and paraventricular nuclei is inconsistent with TSH.
*Hyperplasia of the adrenal zona fasciculata*
- **Adrenocorticotropic hormone (ACTH)** from the anterior pituitary stimulates the adrenal cortex, including the zona fasciculata, to produce cortisol.
- The hormone described here originates in the hypothalamus and is transported to the posterior pituitary, not stimulating adrenal hyperplasia.
*Increased insulin-like growth factor 1 production*
- **Insulin-like growth factor 1 (IGF-1)** production is stimulated primarily by **growth hormone (GH)**, which is secreted by the anterior pituitary.
- This function is not associated with hormones produced in the supraoptic and paraventricular nuclei.
*Maturation of primordial germ cells*
- The maturation of **primordial germ cells** is regulated by **gonadotropins (FSH and LH)**, which are secreted by the anterior pituitary, and sex steroids.
- This process is not directly controlled by hormones originating from the supraoptic and paraventricular nuclei.
More RAAS in volume regulation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.