RAAS in pathophysiological states US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for RAAS in pathophysiological states. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
RAAS in pathophysiological states US Medical PG Question 1: An investigator is studying patients with acute decompensated congestive heart failure. He takes measurements of a hormone released from atrial myocytes, as well as serial measurements of left atrial and left ventricular pressures. The investigator observes a positive correlation between left atrial pressures and the serum level of this hormone. Which of the following is most likely the mechanism of action of this hormone?
- A. Increases potassium excretion at the collecting ducts
- B. Constricts afferent renal arteriole
- C. Decreases sodium reabsorption at the collecting tubules (Correct Answer)
- D. Decreases reabsorption of bicarbonate in the proximal convoluted tubules
- E. Increases free water reabsorption from the distal tubules
RAAS in pathophysiological states Explanation: ***Decreases sodium reabsorption at the collecting tubules***
- The hormone described, exhibiting a positive correlation with left atrial pressure and released from atrial myocytes, is **Atrial Natriuretic Peptide (ANP)**.
- ANP promotes **natriuresis** (sodium excretion) and **diuresis** by directly inhibiting sodium reabsorption in the collecting tubules, thereby reducing blood volume and cardiac preload.
*Increases potassium excretion at the collecting ducts*
- While ANP does promote fluid and electrolyte excretion, its primary effect is on sodium and water, not a direct increase in **potassium excretion**. **Aldosterone**, not ANP, primarily increases potassium secretion in the collecting ducts.
- This option describes a mechanism more consistent with **mineralocorticoid activity**, which is counteracted by ANP.
*Constricts afferent renal arteriole*
- ANP generally causes **vasodilation** of the afferent arteriole and constriction of the efferent arteriole, increasing glomerular filtration rate (GFR).
- **Angiotensin II** is a primary constrictor of the afferent and efferent renal arterioles, which is the opposite effect of ANP.
*Decreases reabsorption of bicarbonate in the proximal convoluted tubules*
- This mechanism is primarily involved in **acid-base balance** and is influenced by factors like parathyroid hormone or respiratory/metabolic acidosis/alkalosis.
- ANP's main action is on **sodium and water balance**, not directly on bicarbonate reabsorption.
*Increases free water reabsorption from the distal tubules*
- **Vasopressin (Antidiuretic Hormone, ADH)** is responsible for increasing free water reabsorption in the distal tubules and collecting ducts.
- ANP's action is to *increase* water excretion, working in opposition to ADH to reduce circulating fluid volume.
RAAS in pathophysiological states US Medical PG Question 2: A 50-year-old man is brought to the hospital after being found unresponsive in his bed in the morning. He is declared dead on arrival in the emergency room. His wife states that he always had uncontrolled hypertension despite being on multiple medications. An autopsy is performed, and the cause of his death is found to be a hemorrhage in his right basal ganglia. On microscopic examination, the branches of the renal artery have concentric endothelial proliferation with prominent narrowing of the lumen resulting in focal ischemia and hemorrhage of the renal parenchyma. Which of the following is most likely related to the findings in this patient?
- A. Raised cholesterol level in the blood
- B. Elevated ammonia level in the blood
- C. Raised calcium level in the blood
- D. Raised renin level in the blood (Correct Answer)
- E. Elevated C-reactive protein in the blood
RAAS in pathophysiological states Explanation: ***Raised renin level in the blood***
- The patient had uncontrolled **hypertension** leading to a fatal **intracerebral hemorrhage** (typical location: basal ganglia). The key autopsy finding of **concentric endothelial proliferation** with lumen narrowing in renal arteries describes **hyperplastic (proliferative) arteriolosclerosis**, also known as **"onion-skinning"** - the hallmark of **malignant hypertension**.
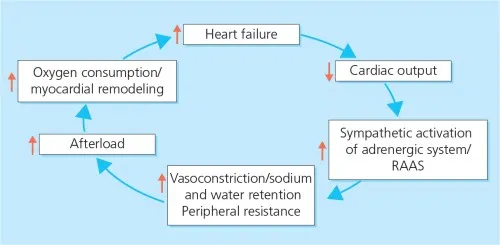
- In malignant hypertension, severe vascular injury causes **renal ischemia**, which triggers massive activation of the **renin-angiotensin-aldosterone system (RAAS)**, leading to markedly **elevated renin levels**. This creates a vicious cycle: renin elevation → further hypertension → more vascular injury → more renin release.
- The combination of uncontrolled hypertension, intracerebral hemorrhage, and hyperplastic arteriolosclerosis strongly indicates a renin-driven hypertensive crisis.
*Raised cholesterol level in the blood*
- While hypercholesterolemia contributes to **atherosclerosis** and chronic vascular disease, it does not explain the acute pathological finding of **concentric endothelial proliferation (onion-skinning)**.
- Atherosclerosis involves **eccentric plaque formation** with lipid deposition, not the concentric smooth muscle and endothelial proliferation seen in malignant hypertension.
- The acute, severe nature of this patient's vascular changes points to hypertensive emergency, not atherosclerotic disease.
*Elevated ammonia level in the blood*
- **Hyperammonemia** is associated with **hepatic encephalopathy** due to severe liver dysfunction (cirrhosis, acute liver failure), which is not suggested by this patient's presentation.
- Elevated ammonia does not cause hypertension, intracerebral hemorrhage, or the specific renal vascular pathology (hyperplastic arteriolosclerosis) described.
*Raised calcium level in the blood*
- **Hypercalcemia** can cause nephrolithiasis, nephrocalcinosis, and various systemic symptoms, but it is not the primary driver of malignant hypertension or intracerebral hemorrhage.
- While chronic hypercalcemia may contribute to vascular calcification (medial calcific sclerosis), it does not produce the **acute proliferative vascular changes** (onion-skinning) characteristic of malignant hypertension.
*Elevated C-reactive protein in the blood*
- **CRP** is a non-specific inflammatory marker that may be elevated in many chronic conditions, including cardiovascular disease.
- However, CRP elevation is a **consequence** rather than a cause of vascular injury, and it does not explain the specific mechanism of malignant hypertension or the pathognomonic finding of hyperplastic arteriolosclerosis.
- The renin-angiotensin system activation is the primary pathophysiologic mechanism in this case.
RAAS in pathophysiological states US Medical PG Question 3: A 33-year-old woman presents to her primary care physician for a wellness check-up. She states that recently she has been feeling well other than headaches that occur occasionally, which improve with ibuprofen and rest. She has a past medical history of hypertension and headaches and is currently taking hydrochlorothiazide. Her temperature is 99.2°F (37.3°C), blood pressure is 157/108 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam reveals a young woman who appears healthy. A normal S1 and S2 are auscultated on cardiac exam, and her lungs are clear with good air movement bilaterally. From her previous visit, it was determined that she has an elevated aldosterone and low renin level. Laboratory values are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 3.7 mEq/L
HCO3-: 29 mEq/L
BUN: 20 mg/dL
Creatinine: 1.1 mg/dL
Which of the following is the most likely diagnosis?
- A. Benign essential hypertension
- B. Pheochromocytoma
- C. Cushing syndrome
- D. Narrowing of the renal arteries
- E. Primary hyperaldosteronism (Correct Answer)
RAAS in pathophysiological states Explanation: ***Primary hyperaldosteronism***
- The patient presents with **hypertension**, **mild hypokalemia (K+ of 3.7 mEq/L)**, and **metabolic alkalosis (HCO3- of 29 mEq/L)**, which are classic signs of primary hyperaldosteronism.
- The elevated aldosterone and low renin levels, as noted from her previous visit, are diagnostic for primary hyperaldosteronism.
*Benign essential hypertension*
- While essential hypertension is common, the presence of **hypokalemia**, **metabolic alkalosis**, and particularly the **elevated aldosterone with low renin** points away from benign essential hypertension, which typically has normal renin-aldosterone ratios.
- This patient's hypertension is likely **secondary** due to a specific endocrine imbalance.
*Pheochromocytoma*
- This condition presents with **episodic or paroxysmal hypertension**, **tachycardia**, **sweating**, and headaches, often in a more dramatic fashion.
- The patient's blood pressure is consistently elevated, and she lacks the typical paroxysmal symptoms and signs of catecholamine excess.
*Cushing syndrome*
- Cushing syndrome is characterized by **hypertension**, central obesity, moon facies, buffalo hump, and striae, none of which are described.
- While it can cause hypertension, it is due to cortisol excess and does not typically present with the specific aldosterone-renin profile seen in this patient.
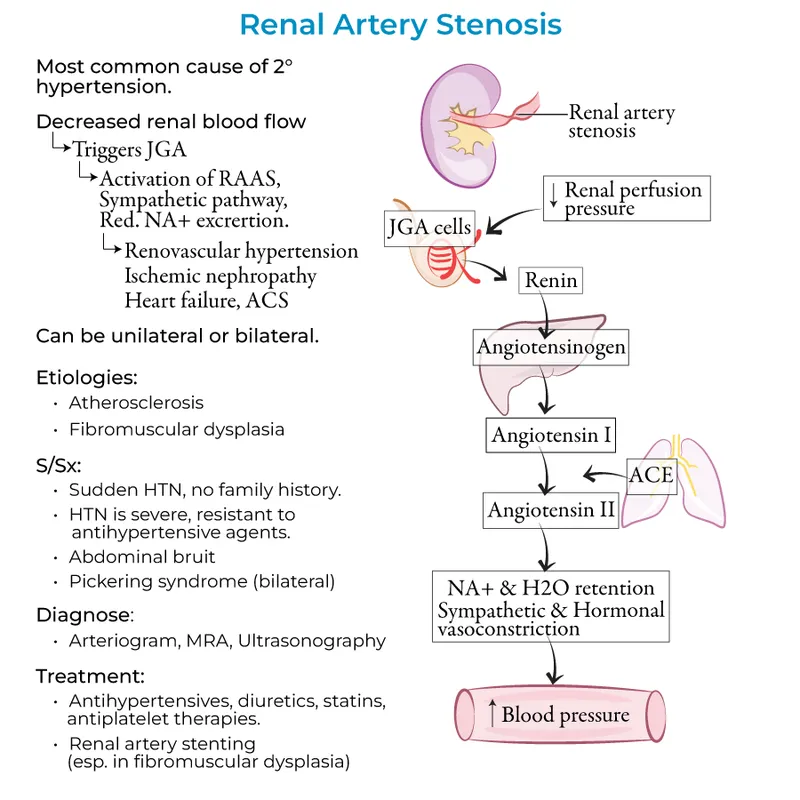
*Narrowing of the renal arteries*
- **Renal artery stenosis** causes **renovascular hypertension** and is associated with **elevated renin levels** as the kidney perceives hypoperfusion and activates the renin-angiotensin-aldosterone system.
- This patient presents with **low renin levels**, which directly contradicts the pathophysiology of renal artery stenosis.
RAAS in pathophysiological states US Medical PG Question 4: A 34-year-old man is being evaluated in an emergency clinic for dizziness and headache after a stressful event at work. He also reports that his face often becomes swollen and he occasionally has difficulty breathing during these spells. Family history is significant for his father who died of a stroke and his mother who often suffers from similar facial swelling. The patient’s blood pressure is 170/80 mm Hg. On physical examination, the patient appears well. Which of the following medications is most likely contraindicated in this patient?
- A. The patient has no contraindications.
- B. Enalapril (Correct Answer)
- C. Sulfadiazine
- D. Penicillin
- E. Losartan
RAAS in pathophysiological states Explanation: **Enalapril**
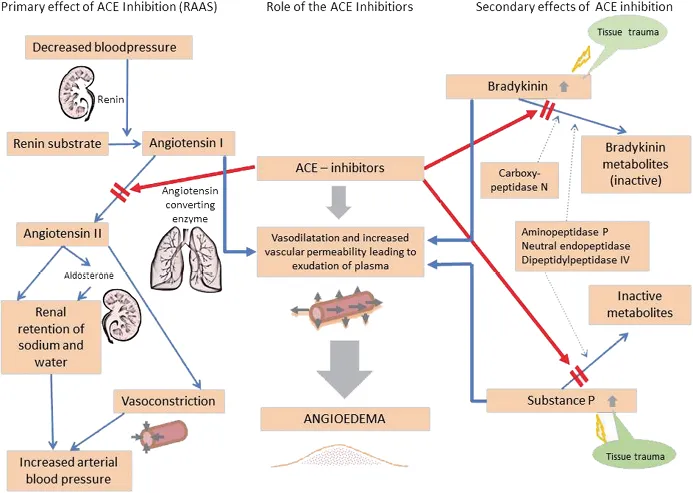
- The patient's presentation with recurrent facial swelling, occasional difficulty breathing, and a family history of similar symptoms in his mother and stroke in his father is highly suggestive of **hereditary angioedema (HAE)**.
- **ACE inhibitors**, such as enalapril, are absolutely contraindicated in patients with HAE because they increase bradykinin levels, which can precipitate or worsen angioedema attacks.
*The patient has no contraindications.*
- The patient's history of recurrent angioedema episodes and a significant family history strongly suggest an underlying condition, likely HAE, which has clear contraindications for certain medications.
- Dismissing contraindications without further investigation into the cause of his angioedema would be unsafe and medically negligent.
*Sulfadiazine*
- **Sulfonamide antibiotics** are not directly contraindicated in HAE.
- While some individuals may have allergies to sulfa drugs, there is no specific link between sulfadiazine and triggering HAE attacks.
*Penicillin*
- Penicillin is a **beta-lactam antibiotic** and is not known to exacerbate or be contraindicated in hereditary angioedema.
- Allergic reactions to penicillin are common, but this is a Type I hypersensitivity, distinct from bradykinin-mediated angioedema.
*Losartan*
- **Angiotensin Receptor Blockers (ARBs)** like losartan generally do not significantly increase bradykinin levels and are typically considered a safer alternative to ACE inhibitors in patients who might develop ACE inhibitor–induced angioedema.
- While rare cases of ARB-induced angioedema have been reported, the risk is considerably lower than with ACE inhibitors, making it a less likely contraindication in this context.
RAAS in pathophysiological states US Medical PG Question 5: An investigator is studying the physiological response during congestive heart failure exacerbations in patients with systolic heart failure. A hormone released by ventricular cardiomyocytes in response to increased wall stress is isolated from a patient's blood sample. The intracellular mechanism by which this hormone acts is most similar to the effect of which of the following substances?
- A. Aldosterone
- B. Platelet-derived growth factor
- C. Nitric oxide (Correct Answer)
- D. Angiotensin II
- E. Human chorionic gonadotropin
RAAS in pathophysiological states Explanation: ***Nitric oxide***
- The hormone described is likely **Brain Natriuretic Peptide (BNP)**, released from ventricular cardiomyocytes in response to **increased wall stress** during heart failure. BNP acts by increasing intracellular **cGMP** to cause vasodilation and natriuresis.
- **Nitric oxide (NO)** also works by stimulating **guanylyl cyclase** to increase intracellular cGMP, leading to smooth muscle relaxation and vasodilation, thus mimicking the intracellular mechanism of BNP.
*Aldosterone*
- **Aldosterone** is a steroid hormone that acts on intracellular mineralocorticoid receptors, altering gene expression to promote **sodium reabsorption** and potassium excretion.
- This mechanism is distinct from the **second messenger system** involving cGMP.
*Platelet-derived growth factor*
- **Platelet-derived growth factor (PDGF)** binds to cell surface receptor tyrosine kinases, initiating a signaling cascade that primarily involves **phosphorylation** and leads to cell growth and proliferation.
- This mechanism is different from the direct activation of **guanylyl cyclase** by BNP.
*Angiotensin II*
- **Angiotensin II** primarily acts on G protein-coupled receptors (GPCRs), leading to vasoconstriction, aldosterone release, and other effects, often through **IP3/DAG** or **cAMP** pathways.
- Its intracellular signaling mechanism is not primarily centered on **cGMP**.
*Human chorionic gonadotropin*
- **Human chorionic gonadotropin (hCG)** is a glycoprotein hormone that binds to **G protein-coupled receptors (GPCRs)**, primarily stimulating the production of **cAMP** as a second messenger.
- While it uses a second messenger system, the specific pathway (cAMP) differs from the **cGMP** pathway activated by BNP.
RAAS in pathophysiological states US Medical PG Question 6: A 71-year-old man presents to his cardiologist with a 1-month history of increasing shortness of breath. He says that he is finding it very difficult to walk up the flight of stairs to his bedroom and he is no longer able to sleep flat on his bed because he wakes up choking for breath. His past medical history is significant for a myocardial infarction 3 years ago. On physical exam, he is found to have diffuse, moist crackles bilaterally on pulmonary auscultation and pitting edema in his lower extremities. Serum tests reveal an increased abundance of a product produced by cardiac myocytes. Which of the following most likely describes the function of this product?
- A. Increases water reabsorption in the kidney
- B. Stimulates parasympathetic nerves
- C. Increases conversion of angiotensin
- D. Inhibits release of renin (Correct Answer)
- E. Binds to intracellular receptors in the collecting duct
RAAS in pathophysiological states Explanation: ***Inhibits release of renin***
- The patient's symptoms (shortness of breath, orthopnea, crackles, edema) and history of MI are consistent with **heart failure**, leading to increased natriuretic peptide production from cardiac myocytes due to ventricular stretch.
- **Brain Natriuretic Peptide (BNP)**, released in heart failure, counteracts fluid retention by inhibiting renin release, thereby reducing aldosterone and angiotensin II, and promoting diuresis and natriuresis.
*Increases water reabsorption in the kidney*
- This is the primary function of **Antidiuretic Hormone (ADH)**, which acts on the collecting ducts to increase water reabsorption.
- Natriuretic peptides, in contrast, promote water excretion rather than retention.
*Stimulates parasympathetic nerves*
- The **parasympathetic nervous system** primarily slows heart rate and promotes digestion through the vagus nerve.
- Natriuretic peptides primarily exert their effects on the cardiovascular and renal systems to regulate blood volume and pressure, not through direct nervous system stimulation.
*Increases conversion of angiotensin*
- The conversion of angiotensin I to **angiotensin II** is mediated by **angiotensin-converting enzyme (ACE)**, primarily in the lungs.
- The product described (natriuretic peptide) works to *inhibit* the renin-angiotensin-aldosterone system (RAAS), thus indirectly reducing angiotensin II levels.
*Binds to intracellular receptors in the collecting duct*
- Hormones that bind to **intracellular receptors** are typically steroid hormones (e.g., aldosterone, cortisol) that regulate gene expression.
- Natriuretic peptides bind to **cell-surface receptors** (guanylyl cyclase receptors) on target cells, activating second messenger systems like cGMP.
RAAS in pathophysiological states US Medical PG Question 7: A 54-year-old man is brought to the emergency department after having been hit by a car while riding his bicycle. He was not wearing a helmet. Despite appropriate life-saving measures, he dies 2 hours later because of a severe intracranial hemorrhage. Autopsy of the heart shows general thickening of the left ventricular wall with narrowing of the ventricular chamber. Which of the following conditions is the most likely underlying cause of the described cardiac changes?
- A. Sarcoidosis
- B. Chronic hypertension (Correct Answer)
- C. Chronic heavy drinking
- D. Aortic regurgitation
- E. Hemochromatosis
RAAS in pathophysiological states Explanation: ***Chronic hypertension***
- **Systemic hypertension** leads to increased **afterload** on the left ventricle, causing **concentric hypertrophy** to normalize wall stress.
- This results in a thickened left ventricular wall and a **reduced ventricular chamber size**, which is a classic finding in long-standing untreated hypertension.
*Sarcoidosis*
- Cardiac sarcoidosis would typically present with **granulomatous inflammation** and could lead to **restrictive cardiomyopathy** or **conduction abnormalities**.
- It is less likely to cause isolated, generalized concentric left ventricular hypertrophy.
*Chronic heavy drinking*
- Chronic heavy alcohol consumption can cause **dilated cardiomyopathy**, characterized by ventricular dilation and systolic dysfunction.
- This is distinct from the concentric hypertrophy and narrowed chamber described.
*Aortic regurgitation*
- **Aortic regurgitation** causes **volume overload** on the left ventricle, leading to **eccentric hypertrophy** (ventricular dilation with increased wall thickness but maintained or increased chamber size).
- This is unlike the "narrowing of the ventricular chamber" seen in concentric hypertrophy.
*Hemochromatosis*
- **Hemochromatosis** causes **iron deposition** in myocardial cells, leading to **restrictive or dilated cardiomyopathy**.
- While it can cause heart failure, it typically does not present as isolated concentric hypertrophy with a narrowed chamber.
RAAS in pathophysiological states US Medical PG Question 8: A 61-year-old obese man with recently diagnosed hypertension returns to his primary care provider for a follow-up appointment and blood pressure check. He reports feeling well with no changes since starting his new blood pressure medication 1 week ago. His past medical history is noncontributory. Besides his blood pressure medication, he takes atorvastatin and a daily multivitamin. The patient reports a 25-pack-year smoking history and is a social drinker on weekends. Today his physical exam is normal. Vital signs and laboratory results are provided in the table.
Laboratory test
2 weeks ago Today
Blood pressure 159/87 mm Hg Blood pressure 164/90 mm Hg
Heart rate 90/min Heart rate 92/min
Sodium 140 mE/L Sodium 142 mE/L
Potassium 3.1 mE/L Potassium 4.3 mE/L
Chloride 105 mE/L Chloride 103 mE/L
Carbon dioxide 23 mE/L Carbon dioxide 22 mE/L
BUN 15 mg/dL BUN 22 mg/dL
Creatinine 0.80 mg/dL Creatinine 1.8 mg/dL
Magnetic resonance angiography (MRA) shows a bilateral narrowing of renal arteries. Which of the following is most likely this patient's new medication that caused his acute renal failure?
- A. Clonidine
- B. Verapamil
- C. Hydralazine
- D. Captopril (Correct Answer)
- E. Hydrochlorothiazide
RAAS in pathophysiological states Explanation: ***Captopril***
- The patient has **bilateral renal artery stenosis** and develops **acute renal failure** after starting a new blood pressure medication. **ACE inhibitors** (like captopril) and **angiotensin receptor blockers (ARBs)** are nephrotoxic in such patients.
- In bilateral renal artery stenosis, the kidneys rely on **angiotensin II** to constrict the efferent arterioles, maintaining **glomerular filtration pressure**. ACE inhibitors block angiotensin II production, leading to a significant drop in glomerular filtration and acute kidney injury.
*Clonidine*
- Clonidine is an **alpha-2 adrenergic agonist** that lowers blood pressure by reducing sympathetic outflow from the central nervous system.
- It is **not directly nephrotoxic** and would not typically cause acute renal failure, especially in the context of renal artery stenosis.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker** that reduces heart rate and blood pressure.
- While it can affect renal hemodynamics, it does not typically cause **acute renal failure** or have a contraindication in bilateral renal artery stenosis like ACE inhibitors.
*Hydralazine*
- Hydralazine is a **direct arterial vasodilator** that lowers blood pressure.
- It is **not associated with acute renal failure** in the setting of renal artery stenosis and would not acutely worsen kidney function.
*Hydrochlorothiazide*
- Hydrochlorothiazide is a **thiazide diuretic** that lowers blood pressure by increasing sodium and water excretion.
- While it can cause **prerenal azotemia** due to volume depletion, it does not directly lead to the severe acute renal failure seen with ACE inhibitors in bilateral renal artery stenosis.
RAAS in pathophysiological states US Medical PG Question 9: A 36-year-old woman is admitted to the hospital for the evaluation of progressive breathlessness. She has no history of major medical illness. Her temperature is 37°C (98.6°F), pulse is 110/min, and respirations are 22/min. Pulse oximetry on room air shows an oxygen saturation of 99%. Cardiac examination shows a loud S1 and S2. There is a grade 2/6 early systolic murmur best heard in the 2nd right intercostal space. Cardiac catheterization shows a mixed venous oxygen saturation of 55% (N= 65–70%). Which of the following is the most likely cause of this patient's breathlessness?
- A. Increased peripheral shunting
- B. Decreased hemoglobin concentration
- C. Increased carbon dioxide retention
- D. Increased pulmonary vascular resistance
- E. Decreased left ventricular ejection fraction (Correct Answer)
RAAS in pathophysiological states Explanation: ***Decreased left ventricular ejection fraction***
- The key finding is a **mixed venous oxygen saturation of 55% (normal 65-70%)** with **normal arterial oxygen saturation (99%)**, which indicates **increased tissue oxygen extraction**
- Increased oxygen extraction occurs when **cardiac output is reduced** → tissues must extract more oxygen from each pass of blood to meet metabolic demands
- This is the classic physiologic compensation in **heart failure with reduced ejection fraction**
- The cardiac findings (loud heart sounds, systolic murmur) suggest underlying cardiac pathology causing reduced cardiac output and progressive breathlessness
*Increased peripheral shunting*
- Peripheral shunting (e.g., arteriovenous malformations) would cause **venous blood to bypass capillary beds**, resulting in **decreased oxygen extraction** and **higher mixed venous O2 saturation**, not lower
- Would typically cause **hypoxemia** with reduced pulse oximetry, but this patient has 99% oxygen saturation
*Decreased hemoglobin concentration*
- Anemia reduces oxygen-carrying capacity but would not explain the **low mixed venous oxygen saturation** to this degree
- The **pulse oximetry of 99%** indicates adequate oxygen saturation of available hemoglobin
- Anemia typically causes **high cardiac output** (compensatory) rather than the low cardiac output state indicated by the low mixed venous O2 saturation
*Increased carbon dioxide retention*
- **Hypercapnia** results from **hypoventilation** and impaired gas exchange, typically causing **respiratory acidosis**
- Would present with altered mental status, drowsiness, or signs of respiratory failure
- Does not explain the **low mixed venous oxygen saturation** with normal arterial oxygen saturation
- The cardiac findings point to a primary cardiac rather than respiratory problem
*Increased pulmonary vascular resistance*
- **Pulmonary hypertension** causes **right ventricular dysfunction** and can present with breathlessness and a loud P2 component of S2
- However, isolated pulmonary hypertension would not cause the same degree of **systemic oxygen extraction** increase
- The low mixed venous O2 saturation indicates **reduced systemic cardiac output**, which primarily reflects **left ventricular dysfunction** rather than isolated right-sided pathology
RAAS in pathophysiological states US Medical PG Question 10: An 83-year-old male presents with dyspnea, orthopnea, and a chest radiograph demonstrating pulmonary edema. A diagnosis of congestive heart failure is considered. The following clinical measurements are obtained: 100 bpm heart rate, 0.2 mL O2/mL systemic blood arterial oxygen content, 0.1 mL O2/mL pulmonary arterial oxygen content, and 400 mL O2/min oxygen consumption. Using the above information, which of the following values represents this patient's cardiac stroke volume?
- A. 30 mL/beat
- B. 70 mL/beat
- C. 40 mL/beat (Correct Answer)
- D. 60 mL/beat
- E. 50 mL/beat
RAAS in pathophysiological states Explanation: ***40 mL/beat***
- First, calculate cardiac output (CO) using the **Fick principle**: CO = Oxygen Consumption / (Arterial O2 content - Venous O2 content). Here, CO = 400 mL O2/min / (0.2 mL O2/mL - 0.1 mL O2/mL) = 400 mL O2/min / 0.1 mL O2/mL = **4000 mL/min**.
- Next, calculate stroke volume (SV) using the formula: SV = CO / Heart Rate. Given a heart rate of 100 bpm, SV = 4000 mL/min / 100 beats/min = **40 mL/beat**.
*30 mL/beat*
- This answer would result if there was an error in calculating either the **cardiac output** or if the **arteriovenous oxygen difference** was overestimated.
- A stroke volume of 30 mL/beat with a heart rate of 100 bpm would yield a cardiac output of 3 L/min, which is sub-physiologic for an oxygen consumption of 400 mL/min given the provided oxygen content values.
*70 mL/beat*
- This stroke volume is higher than calculated and would imply either a significantly **lower heart rate** or a much **higher cardiac output** than derived from the Fick principle with the given values.
- A stroke volume of 70 mL/beat at a heart rate of 100 bpm would mean a cardiac output of 7 L/min, which is inconsistent with the provided oxygen consumption and arteriovenous oxygen difference.
*60 mL/beat*
- This value is higher than the correct calculation, suggesting an error in the initial calculation of **cardiac output** or the **avO2 difference**.
- To get 60 mL/beat, the cardiac output would need to be 6000 mL/min, which would mean an avO2 difference of 0.067 mL O2/mL, not 0.1 mL O2/mL.
*50 mL/beat*
- This stroke volume would result from an incorrect calculation of the **cardiac output**, potentially from a slight miscalculation of the **arteriovenous oxygen difference**.
- A stroke volume of 50 mL/beat at 100 bpm would mean a cardiac output of 5 L/min, requiring an avO2 difference of 0.08 mL O2/mL, which is not consistent with the given values.
More RAAS in pathophysiological states US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.