Negative feedback mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Negative feedback mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Negative feedback mechanisms US Medical PG Question 1: A 75 year-old gentleman presents to his general practitioner. He is currently being treated for hypertension and is on a multi-drug regimen. His current blood pressure is 180/100. The physician would like to begin treatment with minoxidil or hydralazine. Which of the following side effects is associated with administration of these drugs?
- A. Persistent cough
- B. Cyanosis in extremities
- C. Fetal renal toxicity
- D. Systemic volume loss
- E. Reflex tachycardia (Correct Answer)
Negative feedback mechanisms Explanation: ***Reflex tachycardia***
- Both **minoxidil** and **hydralazine** are direct arterial vasodilators, causing a significant drop in **peripheral vascular resistance**.
- This vasodilation triggers a **baroreflex response**, leading to an increase in heart rate and **cardiac contractility** to maintain cardiac output, resulting in reflex tachycardia.
*Persistent cough*
- **Persistent cough** is a common side effect associated with **ACE inhibitors**, such as lisinopril or enalapril, due to the accumulation of **bradykinin**.
- This side effect is not typically seen with **minoxidil** or **hydralazine**, which act directly on vascular smooth muscle to cause vasodilation.
*Cyanosis in extremities*
- **Cyanosis** (bluish discoloration of the skin and mucous membranes) usually indicates **hypoxemia** or poor peripheral perfusion.
- While sometimes associated with severe cardiogenic shock or specific drug toxicities like methemoglobinemia (not related to minoxidil or hydralazine), it is not a direct or typical side effect of these vasodilators.
*Fetal renal toxicity*
- **Fetal renal toxicity**, including **fetal renal dysfunction** and **oligohydramnios**, is a well-known risk associated with **ACE inhibitors** and **ARBs** during pregnancy.
- Neither **minoxidil** nor **hydralazine** are primarily linked to this specific fetal adverse effect, though hydralazine can be used in pregnancy for severe hypertension.
*Systemic volume loss*
- **Systemic volume loss** is usually caused by conditions like **dehydration**, excessive diuresis, or hemorrhage.
- While vasodilators can reduce blood pressure, they do not directly cause **systemic volume depletion**; rather, the reflex response to vasodilation can include fluid retention to counteract the blood pressure drop.
Negative feedback mechanisms US Medical PG Question 2: A 59-year-old man with a history of congestive heart failure presents to his cardiologist for a follow-up visit. His past medical history is notable for diabetes mellitus, hypertension, and obesity. He takes metformin, glyburide, aspirin, lisinopril, and metoprolol. He has a 40 pack-year smoking history and drinks alcohol socially. His temperature is 99.1°F (37.2°C), blood pressure is 150/65 mmHg, pulse is 75/min, and respirations are 20/min. Physical examination reveals bilateral rales at the lung bases and 1+ edema in the bilateral legs. The physician decides to start the patient on an additional diuretic but warns the patient about an increased risk of breast enlargement. Which of the following is the most immediate physiologic effect of the medication in question?
- A. Decreased sodium reabsorption in the distal convoluted tubule
- B. Decreased bicarbonate reabsorption in the proximal convoluted tubule
- C. Decreased sodium reabsorption in the thick ascending limb
- D. Decreased renin enzyme activity
- E. Decreased sodium reabsorption in the collecting duct (Correct Answer)
Negative feedback mechanisms Explanation: ***Decreased sodium reabsorption in the collecting duct***
- The physician is initiating **spironolactone**, an **aldosterone antagonist**, due to its known side effect of **gynecomastia** (breast enlargement).
- Spironolactone acts on the **collecting duct** to inhibit aldosterone's effects, leading to decreased sodium reabsorption and **decreased potassium excretion** (potassium-sparing effect).
- This makes it useful in heart failure but requires monitoring for **hyperkalemia**, especially in patients on ACE inhibitors like lisinopril.
*Decreased sodium reabsorption in the distal convoluted tubule*
- This is the primary site of action for **thiazide diuretics**, such as **hydrochlorothiazide** or **chlorthalidone**.
- While effective for heart failure, thiazides are not associated with breast enlargement.
*Decreased bicarbonate reabsorption in the proximal convoluted tubule*
- This is the main action of **carbonic anhydrase inhibitors**, such as **acetazolamide**.
- These diuretics are typically used for conditions like glaucoma or metabolic alkalosis, not first-line for heart failure and do not cause breast enlargement.
*Decreased sodium reabsorption in the thick ascending limb*
- This is the mechanism of action for **loop diuretics**, such as **furosemide** or **bumetanide**.
- Loop diuretics are potent and frequently used in heart failure, but they do not cause breast enlargement.
*Decreased renin enzyme activity*
- This effect is primarily seen with **beta-blockers** or **direct renin inhibitors**.
- While beta-blockers (like metoprolol, which the patient is already taking) are used in heart failure, they do not cause breast enlargement.
Negative feedback mechanisms US Medical PG Question 3: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Negative feedback mechanisms Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
Negative feedback mechanisms US Medical PG Question 4: Which hormone's secretion is primarily stimulated by increased plasma osmolality?
- A. EPO
- B. PTH
- C. ADH (Correct Answer)
- D. Aldosterone
- E. ANP
Negative feedback mechanisms Explanation: ***ADH***
- **Antidiuretic hormone (ADH)**, also known as vasopressin, is primarily released in response to an increase in **plasma osmolality**.
- Its main function is to promote water reabsorption in the kidneys, thereby decreasing osmolality and concentrating urine.
*EPO*
- **Erythropoietin (EPO)** is a hormone primarily produced by the kidneys in response to **hypoxia** (low oxygen levels), not increased plasma osmolality.
- It stimulates the production of **red blood cells** in the bone marrow.
*PTH*
- **Parathyroid hormone (PTH)** regulates **calcium** and phosphate levels in the blood, primarily stimulated by low plasma calcium concentrations.
- It does not directly respond to changes in plasma osmolality.
*Aldosterone*
- **Aldosterone** is a mineralocorticoid hormone involved in regulating **blood pressure** and electrolyte balance, particularly sodium and potassium.
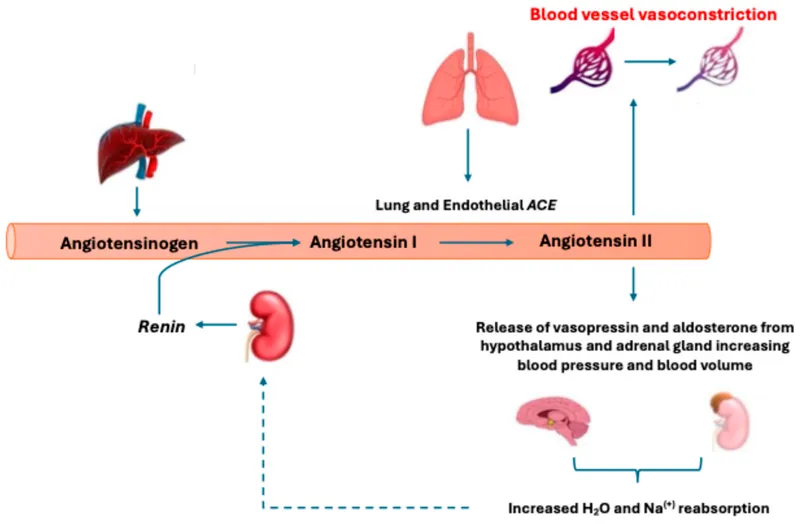
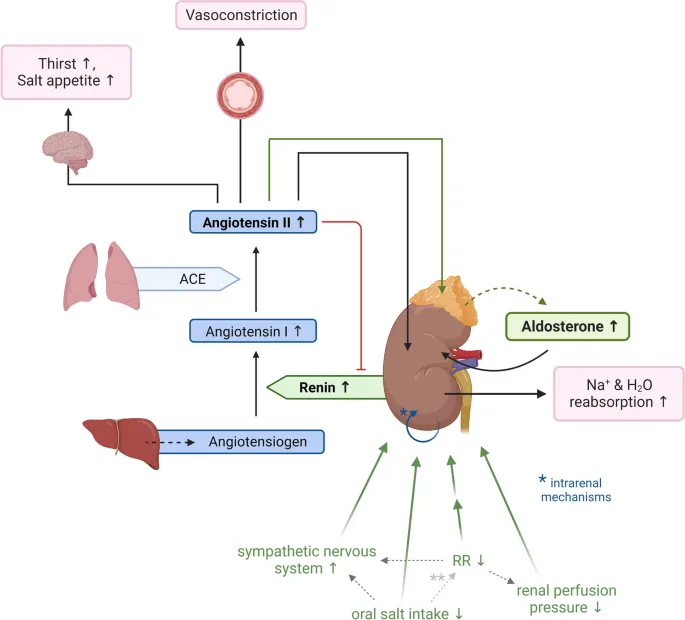
- Its secretion is primarily stimulated by the **renin-angiotensin-aldosterone system** in response to low blood volume or pressure, and high potassium levels, not plasma osmolality.
Negative feedback mechanisms US Medical PG Question 5: A new drug X is being tested for its effect on renal function. During the experiments, the researchers found that in patients taking substance X, the urinary concentration of sodium decreases while urine potassium concentration increase. Which of the following affects the kidneys in the same way as does substance X?
- A. Aldosterone (Correct Answer)
- B. Furosemide
- C. Spironolactone
- D. Atrial natriuretic peptide
- E. Hydrochlorothiazide
Negative feedback mechanisms Explanation: ***Aldosterone***
- **Aldosterone** acts on the **principal cells** of the **collecting duct** to increase sodium reabsorption and potassium secretion.
- This action leads to a decrease in urinary sodium concentration and an increase in urinary potassium concentration, matching the effects of drug X.
*Furosemide*
- **Furosemide** is a **loop diuretic** that inhibits the **Na-K-2Cl cotransporter** in the **thick ascending limb** of the loop of Henle.
- This inhibition leads to increased excretion of sodium, potassium, and water, resulting in higher urinary sodium concentration.
*Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that blocks aldosterone's effects on the collecting duct.
- This leads to increased sodium excretion and decreased potassium excretion (potassium-sparing effect), which is the opposite of drug X.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** is released in response to atrial stretch and causes **natriuresis** (increased sodium excretion) and **diuresis**.
- It works by dilating afferent arterioles and constricting efferent arterioles, increasing GFR, and inhibiting sodium reabsorption, thus increasing urinary sodium concentration.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that inhibits the **Na-Cl cotransporter** in the **distal convoluted tubule**.
- This leads to increased sodium and chloride excretion but typically causes potassium wasting (hypokalemia), which differs from the increased urinary potassium concentration seen with drug X.
Negative feedback mechanisms US Medical PG Question 6: A physician is choosing whether to prescribe losartan or lisinopril to treat hypertension in a 56-year-old male. Relative to losartan, one would expect treatment with lisinopril to produce which of the following changes in the circulating levels of these peptides?
- A. Aldosterone increase; bradykinin decrease
- B. Angiotensin II increase; bradykinin decrease
- C. Renin decrease; angiotensin I increase
- D. Bradykinin increase; angiotensin II decrease (Correct Answer)
- E. Renin decrease; angiotensin II increase
Negative feedback mechanisms Explanation: ***Bradykinin increase; angiotensin II decrease***
- **Lisinopril** is an **ACE inhibitor**, which directly blocks the conversion of **angiotensin I** to **angiotensin II**, leading to a decrease in circulating **angiotensin II** levels.
- ACE is also responsible for the breakdown of **bradykinin**, so inhibiting ACE with lisinopril will lead to an **increase in bradykinin** levels, contributing to vasodilation but also the characteristic cough.
*Aldosterone increase; bradykinin decrease*
- **Lisinopril** (an ACE inhibitor) decreases **angiotensin II**, which in turn leads to a **decrease in aldosterone** synthesis and release, not an increase.
- **Bradykinin** levels would increase due to ACE inhibition, as ACE is involved in its degradation.
*Angiotensin II increase; bradykinin decrease*
- **Lisinopril** directly inhibits the enzyme responsible for producing **angiotensin II**, thus leading to its **decrease**, not an increase.
- **Bradykinin** levels would increase because its degradation pathway (via ACE) is blocked, not decrease.
*Renin decrease; angiotensin I increase*
- **Lisinopril** reduces the negative feedback on **renin** release, leading to an **increase in renin** levels, not a decrease.
- While ACE is inhibited by lisinopril, this leads to an accumulation of its substrate, **angiotensin I**, resulting in an increase of angiotensin I.
*Renin decrease; angiotensin II increase*
- As an ACE inhibitor, lisinopril would lead to an **increase in renin** due to reduced negative feedback from angiotensin II, not a decrease.
- **Angiotensin II** levels would **decrease** because its production from angiotensin I is directly inhibited by lisinopril.
Negative feedback mechanisms US Medical PG Question 7: A 71-year-old African American man diagnosed with high blood pressure presents to the outpatient clinic. In the clinic, his blood pressure is 161/88 mm Hg with a pulse of 88/min. He has had similar blood pressure measurements in the past, and you initiate captopril. He presents back shortly after initiation with extremely swollen lips, tongue, and face. After captopril is discontinued, what is the most appropriate step for the management of his high blood pressure?
- A. Initiate a beta-blocker
- B. Switch to ramipril
- C. Initiate a thiazide diuretic (Correct Answer)
- D. Reinitiate captopril
- E. Initiate an ARB
Negative feedback mechanisms Explanation: ***Initiate a thiazide diuretic***
- The patient experienced **angioedema** after taking **captopril**, which is an **ACE inhibitor**. This is a life-threatening adverse effect, and it indicates that all **ACE inhibitors** should be avoided in the future.
- Due to the risk of angioedema, a different class of antihypertensive should be used. Given his African American ethnicity, a **thiazide diuretic** or **calcium channel blocker** would be an appropriate initial choice for monotherapy if hypertension is stage 1, or combination therapy if stage 2 hypertension, otherwise, a second agent, such as a **calcium channel blocker**, can be added.
*Initiate a beta-blocker*
- While beta-blockers are a class of antihypertensive drugs, they are generally not preferred as **first-line monotherapy** for **hypertension**, especially in older African American patients, unless there are specific comorbidities like heart failure or coronary artery disease.
- The most appropriate first-line choice after **ACE inhibitor-induced angioedema** would be a thiazide diuretic or calcium channel blocker, as per ACC/AHA guidelines for primary hypertension.
*Switch to ramipril*
- **Ramipril** is also an **ACE inhibitor**, and the patient experienced **angioedema** with **captopril** (another ACE inhibitor).
- Cross-reactivity and recurrence of angioedema are high with other ACE inhibitors, making this choice extremely dangerous and contraindicated.
*Reinitiate captopril*
- The patient developed **angioedema**, a severe and potentially fatal hypersensitivity reaction, to **captopril**.
- Reinitiating the same drug could lead to recurrent, and potentially more severe, angioedema and is therefore absolutely contraindicated.
*Initiate an ARB*
- **Angiotensin receptor blockers (ARBs)**, while a different class from ACE inhibitors, act on the renin-angiotensin system and carry a **small but significant risk of cross-reactivity** leading to angioedema, especially in patients who have experienced it with an ACE inhibitor.
- Given the life-threatening nature of angioedema, it is generally recommended to avoid ARBs if a patient has a history of ACE inhibitor-induced angioedema.
Negative feedback mechanisms US Medical PG Question 8: Which mechanism primarily regulates sodium reabsorption in the collecting duct?
- A. Glomerulotubular balance
- B. Atrial natriuretic peptide
- C. Antidiuretic hormone
- D. Aldosterone (Correct Answer)
Negative feedback mechanisms Explanation: ***Aldosterone***
- **Aldosterone** is the primary hormone that stimulates **sodium reabsorption** and **potassium secretion** in the principal cells of the collecting duct.
- It acts by increasing the synthesis and activity of **ENaC channels** on the apical membrane and **Na+/K+-ATPase pumps** on the basolateral membrane.
*Glomerulotubular balance*
- **Glomerulotubular balance** refers to the mechanism by which the **proximal tubule** reabsorbs a constant fraction of the filtered load, regardless of changes in glomerular filtration rate (GFR).
- This mechanism maintains a relatively constant delivery of fluid and solutes to downstream segments but does not primarily regulate sodium in the collecting duct.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** primarily **inhibits sodium reabsorption** in the collecting duct, leading to **natriuresis** and **diuresis**, which is the opposite of sodium reabsorption.
- ANP is released in response to atrial stretch, indicating increased blood volume.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)** primarily regulates **water reabsorption** in the collecting duct by increasing the insertion of **aquaporin-2 channels** into the apical membrane, making the collecting duct permeable to water.
- While ADH can indirectly affect sodium concentration by influencing water movement, it does not directly regulate sodium transport to the same extent as aldosterone.
Negative feedback mechanisms US Medical PG Question 9: A senior medicine resident receives negative feedback on a grand rounds presentation from his attending. He is told sternly that he must improve his performance on the next project. Later that day, he yells at his medical student for not showing enough initiative, though he had voiced only satisfaction with the student's performance up until this point. Which of the following psychological defense mechanisms is he demonstrating?
- A. Transference
- B. Projection
- C. Countertransference
- D. Externalization
- E. Displacement (Correct Answer)
Negative feedback mechanisms Explanation: ***Displacement***
- **Displacement** occurs when a person redirects an emotional response from a dangerous or threatening object to a safer, less threatening one. In this scenario, the resident, unable to express frustration towards his attending, redirects it onto the medical student.
- The resident's anger and frustration stemmed from the negative feedback and stern reprimand from his attending; his subsequent yelling at the medical student despite prior satisfaction is a clear example of shifting these feelings to a less powerful target.
*Transference*
- **Transference** involves a patient unconsciously redirecting feelings and attitudes from important past relationships (e.g., parents) onto the therapist or other individuals in the present.
- This scenario describes the resident's reaction to current stress, not the re-enactment of past relational patterns in a clinical setting.
*Projection*
- **Projection** is a defense mechanism where individuals attribute their own unacceptable thoughts, feelings, or impulses to another person.
- The resident is not attributing his own perceived inadequacy or anger to the student; rather, he is expressing his anger *at* the student, which originated from a different source.
*Countertransference*
- **Countertransference** is a phenomenon in therapy where the therapist projects their own feelings onto the patient, often in response to the patient's transference.
- This mechanism is specific to the therapeutic context and involves the therapist's emotional reactions, which is not applicable to the resident's general interaction with a medical student.
*Externalization*
- **Externalization** is a broad term referring to the tendency to blame outside factors for one's problems or failures, essentially viewing distress as coming from outside oneself.
- While related to projection, externalization specifically focuses on attributing causality of one's struggles to external circumstances rather than a direct redirection of an emotional response to a different target. The resident isn't just blaming others for his problems; he is actively expressing displaced anger.
Negative feedback mechanisms US Medical PG Question 10: A 71-year old man is brought to the emergency department because of progressively worsening shortness of breath and fatigue for 3 days. During the last month, he has also noticed dark colored urine. He had an upper respiratory infection 6 weeks ago. He underwent a cholecystectomy at the age of 30 years. He has hypertension, hyperlipidemia, and type 2 diabetes mellitus. He immigrated to the US from Italy 50 years ago. Current medications include simvastatin, lisinopril, and metformin. He appears pale. His temperature is 37.1°C (98.8°F), pulse is 96/min, respirations are 21/min, and blood pressure is 150/80 mm Hg. Auscultation of the heart shows a grade 4/6 systolic murmur over the right second intercostal space that radiates to the carotids. Laboratory studies show:
Leukocyte count 9,000/mm3
Hemoglobin 8.3 g/dL
Hematocrit 24%
Platelet count 180,000/mm3
LDH 212 U/L
Haptoglobin 15 mg/dL (N=41–165)
Serum
Na+ 138 mEq/L
K+ 4.5 mEq/L
CL- 102 mEq/L
HCO3- 24 mEq/L
Urea nitrogen 20 mg/dL
Creatinine 1.2 mg/dL
Total bilirubin 1.8 mg/dL
Stool testing for occult blood is negative. Direct Coombs test is negative. Echocardiography shows an aortic jet velocity of 4.2 m/s and a mean pressure gradient of 46 mm Hg. Which of the following is the most appropriate next step in management to treat this patient's anemia?
- A. Aortic valve replacement (Correct Answer)
- B. Administration of corticosteroids
- C. Discontinuation of medication
- D. Administration of hydroxyurea
- E. Supplementation with iron
Negative feedback mechanisms Explanation: ***Aortic valve replacement***
- The patient's **severe aortic stenosis** (aortic jet velocity >4.0 m/s and mean pressure gradient >40 mmHg) is causing **shear stress** on red blood cells, leading to **microangiopathic hemolytic anemia**. This is characterized by low hemoglobin, high LDH, low haptoglobin, and negative Coombs test.
- **Aortic valve replacement** is the definitive treatment to reduce the shear stress, resolve the hemolysis, and improve the patient's symptoms of anemia and heart failure.
*Administration of corticosteroids*
- Corticosteroids are primarily used in **autoimmune hemolytic anemia** (positive Coombs test), which is not the case here as the direct Coombs test is negative.
- They would not address the underlying **mechanical destruction of red blood cells** due to aortic stenosis.
*Discontinuation of medication*
- The patient's current medications (simvastatin, lisinopril, metformin) are for managing his chronic conditions and are **not associated with hemolytic anemia**. Discontinuing them would be inappropriate and potentially harmful.
- There is no evidence to suggest a **drug-induced hemolytic anemia** in this case.
*Administration of hydroxyurea*
- Hydroxyurea is used in conditions like **sickle cell anemia** or **polycythemia vera** to modify red blood cell production or reduce cell counts, respectively.
- It has no role in treating **mechanical hemolytic anemia** caused by valvular heart disease.
*Supplementation with iron*
- While the patient has anemia, it is a **hemolytic anemia**, not an iron deficiency anemia, as indicated by the low haptoglobin and elevated LDH.
- Iron supplementation would **not stop the destruction of red blood cells** caused by the turbulent flow across the aortic valve.
More Negative feedback mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.