Angiotensin converting enzyme function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Angiotensin converting enzyme function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Angiotensin converting enzyme function US Medical PG Question 1: A 75 year-old gentleman presents to his general practitioner. He is currently being treated for hypertension and is on a multi-drug regimen. His current blood pressure is 180/100. The physician would like to begin treatment with minoxidil or hydralazine. Which of the following side effects is associated with administration of these drugs?
- A. Persistent cough
- B. Cyanosis in extremities
- C. Fetal renal toxicity
- D. Systemic volume loss
- E. Reflex tachycardia (Correct Answer)
Angiotensin converting enzyme function Explanation: ***Reflex tachycardia***
- Both **minoxidil** and **hydralazine** are direct arterial vasodilators, causing a significant drop in **peripheral vascular resistance**.
- This vasodilation triggers a **baroreflex response**, leading to an increase in heart rate and **cardiac contractility** to maintain cardiac output, resulting in reflex tachycardia.
*Persistent cough*
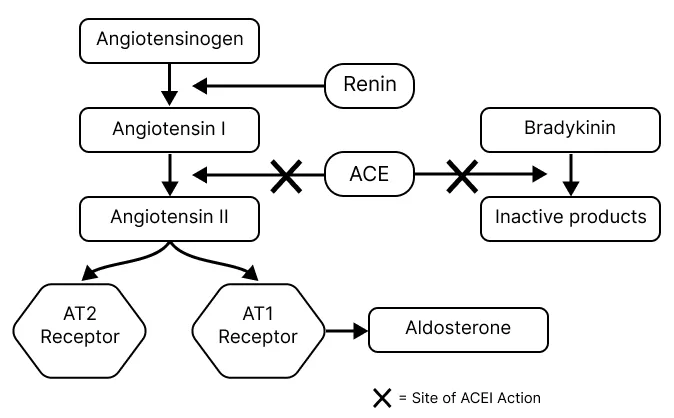
- **Persistent cough** is a common side effect associated with **ACE inhibitors**, such as lisinopril or enalapril, due to the accumulation of **bradykinin**.
- This side effect is not typically seen with **minoxidil** or **hydralazine**, which act directly on vascular smooth muscle to cause vasodilation.
*Cyanosis in extremities*
- **Cyanosis** (bluish discoloration of the skin and mucous membranes) usually indicates **hypoxemia** or poor peripheral perfusion.
- While sometimes associated with severe cardiogenic shock or specific drug toxicities like methemoglobinemia (not related to minoxidil or hydralazine), it is not a direct or typical side effect of these vasodilators.
*Fetal renal toxicity*
- **Fetal renal toxicity**, including **fetal renal dysfunction** and **oligohydramnios**, is a well-known risk associated with **ACE inhibitors** and **ARBs** during pregnancy.
- Neither **minoxidil** nor **hydralazine** are primarily linked to this specific fetal adverse effect, though hydralazine can be used in pregnancy for severe hypertension.
*Systemic volume loss*
- **Systemic volume loss** is usually caused by conditions like **dehydration**, excessive diuresis, or hemorrhage.
- While vasodilators can reduce blood pressure, they do not directly cause **systemic volume depletion**; rather, the reflex response to vasodilation can include fluid retention to counteract the blood pressure drop.
Angiotensin converting enzyme function US Medical PG Question 2: An investigator is studying patients with acute decompensated congestive heart failure. He takes measurements of a hormone released from atrial myocytes, as well as serial measurements of left atrial and left ventricular pressures. The investigator observes a positive correlation between left atrial pressures and the serum level of this hormone. Which of the following is most likely the mechanism of action of this hormone?
- A. Increases potassium excretion at the collecting ducts
- B. Constricts afferent renal arteriole
- C. Decreases sodium reabsorption at the collecting tubules (Correct Answer)
- D. Decreases reabsorption of bicarbonate in the proximal convoluted tubules
- E. Increases free water reabsorption from the distal tubules
Angiotensin converting enzyme function Explanation: ***Decreases sodium reabsorption at the collecting tubules***
- The hormone described, exhibiting a positive correlation with left atrial pressure and released from atrial myocytes, is **Atrial Natriuretic Peptide (ANP)**.
- ANP promotes **natriuresis** (sodium excretion) and **diuresis** by directly inhibiting sodium reabsorption in the collecting tubules, thereby reducing blood volume and cardiac preload.
*Increases potassium excretion at the collecting ducts*
- While ANP does promote fluid and electrolyte excretion, its primary effect is on sodium and water, not a direct increase in **potassium excretion**. **Aldosterone**, not ANP, primarily increases potassium secretion in the collecting ducts.
- This option describes a mechanism more consistent with **mineralocorticoid activity**, which is counteracted by ANP.
*Constricts afferent renal arteriole*
- ANP generally causes **vasodilation** of the afferent arteriole and constriction of the efferent arteriole, increasing glomerular filtration rate (GFR).
- **Angiotensin II** is a primary constrictor of the afferent and efferent renal arterioles, which is the opposite effect of ANP.
*Decreases reabsorption of bicarbonate in the proximal convoluted tubules*
- This mechanism is primarily involved in **acid-base balance** and is influenced by factors like parathyroid hormone or respiratory/metabolic acidosis/alkalosis.
- ANP's main action is on **sodium and water balance**, not directly on bicarbonate reabsorption.
*Increases free water reabsorption from the distal tubules*
- **Vasopressin (Antidiuretic Hormone, ADH)** is responsible for increasing free water reabsorption in the distal tubules and collecting ducts.
- ANP's action is to *increase* water excretion, working in opposition to ADH to reduce circulating fluid volume.
Angiotensin converting enzyme function US Medical PG Question 3: A 70-year-old male presents to his primary care provider complaining of decreased sexual function. He reports that over the past several years, he has noted a gradual decline in his ability to sustain an erection. He used to wake up with erections but no longer does. His past medical history is notable for diabetes, hyperlipidemia, and a prior myocardial infarction. He takes metformin, glyburide, aspirin, and atorvastatin. He drinks 2-3 drinks per week and has a 25 pack-year smoking history. He has been happily married for 40 years. He retired from his job as a construction worker 5 years ago and has been enjoying retirement with his wife. His physician recommends starting a medication that is also used in the treatment of pulmonary hypertension. Which of the following is a downstream effect of this medication?
- A. Increase cGMP degradation
- B. Increase cAMP production
- C. Increase PDE5 activity
- D. Decrease nitric oxide production
- E. Decrease cGMP degradation (Correct Answer)
Angiotensin converting enzyme function Explanation: ***Decrease cGMP degradation***
- The medication described is likely a **phosphodiesterase-5 (PDE5) inhibitor** (e.g., sildenafil, tadalafil), used for erectile dysfunction and pulmonary hypertension.
- These drugs work by inhibiting the enzyme PDE5, which is responsible for the breakdown of **cyclic GMP (cGMP)**, thereby increasing cGMP levels.
*Increase cGMP degradation*
- This is the **opposite** of the medication's intended effect, as it would lead to reduced cGMP levels and worsen erectile dysfunction.
- An increase in cGMP degradation would diminish the **vasodilatory** effects necessary for erection.
*Increase cAMP production*
- This medication primarily affects the **cGMP pathway**, not directly boosting cyclic AMP (cAMP) production.
- While cAMP also plays a role in vasodilation, it's regulated by different enzymes and pathways, such as **adenylyl cyclase**.
*Increase PDE5 activity*
- This would lead to a more **rapid breakdown of cGMP**, counteracting the goal of the medication and exacerbating erectile dysfunction.
- The medication's mechanism is specifically designed to **inhibit PDE5 activity**.
*Decrease nitric oxide production*
- **Nitric oxide (NO)** production is a **precursor** to cGMP synthesis, as NO activates guanylate cyclase to produce cGMP.
- Decreasing NO production would **reduce cGMP levels**, which is contrary to the action of PDE5 inhibitors.
Angiotensin converting enzyme function US Medical PG Question 4: A 56-year-old man with substernal chest pain calls 911. When paramedics arrive, they administer drug X sublingually for the immediate relief of angina. What is the most likely site of action of drug X?
- A. Pulmonary arteries
- B. Large veins (Correct Answer)
- C. Cardiac muscle
- D. Large arteries
- E. Arterioles
Angiotensin converting enzyme function Explanation: ***Large veins***
- Drug X is most likely **nitroglycerin**, which is administered sublingually for rapid relief of angina.
- Its primary mechanism of action involves **vasodilation of large veins**, leading to **decreased preload** and reduced myocardial oxygen demand.
*Pulmonary arteries*
- While nitroglycerin can cause some pulmonary vasodilation, its primary therapeutic effect in angina is not focused on the **pulmonary arteries**.
- Medications targeting pulmonary arteries are typically used for conditions like **pulmonary hypertension**.
*Cardiac muscle*
- Nitroglycerin does not directly act on **cardiac muscle** to improve angina; its effects are primarily vascular.
- It does not directly enhance contractility or directly reduce oxygen consumption at the myocardial cellular level.
*Large arteries*
- Nitroglycerin does cause some **arterial vasodilation**, but this effect is less prominent than its venodilating effect at typical anti-anginal doses.
- Significant arterial dilation can lead to **hypotension**, which is a side effect, not the primary therapeutic mechanism for angina relief.
*Arterioles*
- Nitroglycerin causes **less vasodilation of resistance arterioles** compared to its venodilating effects.
- While some arteriolar dilation occurs, it mainly contributes to a decrease in **afterload**, but the predominant effect for angina relief is preload reduction.
Angiotensin converting enzyme function US Medical PG Question 5: An investigator is studying the physiological response during congestive heart failure exacerbations in patients with systolic heart failure. A hormone released by ventricular cardiomyocytes in response to increased wall stress is isolated from a patient's blood sample. The intracellular mechanism by which this hormone acts is most similar to the effect of which of the following substances?
- A. Aldosterone
- B. Platelet-derived growth factor
- C. Nitric oxide (Correct Answer)
- D. Angiotensin II
- E. Human chorionic gonadotropin
Angiotensin converting enzyme function Explanation: ***Nitric oxide***
- The hormone described is likely **Brain Natriuretic Peptide (BNP)**, released from ventricular cardiomyocytes in response to **increased wall stress** during heart failure. BNP acts by increasing intracellular **cGMP** to cause vasodilation and natriuresis.
- **Nitric oxide (NO)** also works by stimulating **guanylyl cyclase** to increase intracellular cGMP, leading to smooth muscle relaxation and vasodilation, thus mimicking the intracellular mechanism of BNP.
*Aldosterone*
- **Aldosterone** is a steroid hormone that acts on intracellular mineralocorticoid receptors, altering gene expression to promote **sodium reabsorption** and potassium excretion.
- This mechanism is distinct from the **second messenger system** involving cGMP.
*Platelet-derived growth factor*
- **Platelet-derived growth factor (PDGF)** binds to cell surface receptor tyrosine kinases, initiating a signaling cascade that primarily involves **phosphorylation** and leads to cell growth and proliferation.
- This mechanism is different from the direct activation of **guanylyl cyclase** by BNP.
*Angiotensin II*
- **Angiotensin II** primarily acts on G protein-coupled receptors (GPCRs), leading to vasoconstriction, aldosterone release, and other effects, often through **IP3/DAG** or **cAMP** pathways.
- Its intracellular signaling mechanism is not primarily centered on **cGMP**.
*Human chorionic gonadotropin*
- **Human chorionic gonadotropin (hCG)** is a glycoprotein hormone that binds to **G protein-coupled receptors (GPCRs)**, primarily stimulating the production of **cAMP** as a second messenger.
- While it uses a second messenger system, the specific pathway (cAMP) differs from the **cGMP** pathway activated by BNP.
Angiotensin converting enzyme function US Medical PG Question 6: A 57-year-old otherwise healthy male presents to his primary care physician for a check-up. He has no complaints. His blood pressure at the previous visit was 160/95. The patient did not wish to be on any medications and at the time attempted to manage his blood pressure with diet and exercise. On repeat measurement of blood pressure today, the reading is 163/92. His physician decides to prescribe a medication which the patient agrees to take. The patient calls his physician 6 days later complaining of a persistent cough, but otherwise states that his BP was measured as 145/85 at a local pharmacy. Which of the following is a contraindication to this medication?
- A. Congestive heart failure
- B. Black race
- C. Bilateral renal artery stenosis (Correct Answer)
- D. Chronic obstructive pulmonary disease
- E. Gout
Angiotensin converting enzyme function Explanation: ***Bilateral renal artery stenosis***
- The patient's developing **cough** after starting a new antihypertensive suggests he was likely prescribed an **ACE inhibitor**.
- **Bilateral renal artery stenosis** is a strong contraindication for ACE inhibitors due to the risk of precipitating **acute kidney injury**, as these medications rely on efferent arteriolar vasodilation to maintain renal perfusion when there's reduced afferent flow.
*Congestive heart failure*
- **ACE inhibitors** are often a **first-line treatment** for heart failure due to their ability to improve cardiac remodeling and reduce mortality.
- They are used to prevent ventricular remodeling and reduce afterload, making this an indication, not a contraindication.
*Black race*
- While ACE inhibitors may be **less effective as monotherapy** in black patients, they are not contraindicated and can be effectively used in combination with other antihypertensives, such as **thiazide diuretics** or **calcium channel blockers**.
- **African Americans** often respond better to calcium channel blockers and diuretics for hypertension but ACE inhibitors are not absolutely contraindicated.
*Chronic obstructive pulmonary disease*
- **ACE inhibitors** are **not contraindicated** in COPD, as they do not affect bronchial smooth muscle tone.
- **Beta-blockers**, not ACE inhibitors, are typically avoided or used with caution in patients with reactive airway diseases like asthma or severe COPD.
*Gout*
- **ACE inhibitors** do not significantly impact **uric acid levels** and are generally safe for use in patients with gout.
- In contrast, **thiazide diuretics** can increase uric acid levels and worsen gout, but this is not the medication indicated by the patient's cough.
Angiotensin converting enzyme function US Medical PG Question 7: A 75-year-old woman is brought to a physician’s office by her son with complaints of diarrhea and vomiting for 1 day. Her stool is loose, watery, and yellow-colored, while her vomitus contains partially digested food particles. She denies having blood or mucus in her stools and vomitus. Since the onset of her symptoms, she has not had anything to eat and her son adds that she is unable to tolerate fluids. The past medical history is unremarkable and she does not take any medications regularly. The pulse is 115/min, the respiratory rate is 16/min, the blood pressure is 100/60 mm Hg, and the temperature is 37.0°C (98.6°F). The physical examination shows dry mucous membranes and slightly sunken eyes. The abdomen is soft and non-tender. Which of the following physiologic changes in glomerular filtration rate (GFR), renal plasma flow (RPF), and filtration fraction (FF) are expected?
- A. Decreased GFR, decreased RPF, decreased FF
- B. Decreased GFR, decreased RPF, no change in FF
- C. Increased GFR, increased RPF, increased FF
- D. Increased GFR, decreased RPF, increased FF
- E. Decreased GFR, decreased RPF, increased FF (Correct Answer)
Angiotensin converting enzyme function Explanation: ***Decreased GFR, decreased RPF, increased FF***
- Due to **dehydration** from diarrhea and vomiting, there is a decrease in blood volume leading to decreased renal blood flow and **renal plasma flow (RPF)**.
- The body responds to hypovolemia by activating the renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system, which cause **preferential efferent arteriolar constriction** (more than afferent constriction). This helps maintain glomerular hydrostatic pressure despite reduced renal perfusion.
- As a result, **GFR decreases** but proportionally **less than RPF decreases**, causing the **filtration fraction (FF = GFR/RPF) to increase**.
- In this patient with significant dehydration (tachycardia, hypotension, dry mucous membranes), both GFR and RPF are reduced, but FF is elevated due to compensatory mechanisms.
*Decreased GFR, decreased RPF, decreased FF*
- While GFR and RPF will decrease due to dehydration, the **filtration fraction is expected to increase**, not decrease.
- A decreased FF would imply GFR fell proportionally more than RPF, which contradicts the physiologic response where efferent arteriolar constriction helps preserve GFR relative to RPF.
*Decreased GFR, decreased RPF, no change in FF*
- With significant fluid loss and compensatory mechanisms (efferent arteriolar constriction via angiotensin II), a change in **filtration fraction** is expected.
- The body actively alters arteriolar tone to prioritize GFR maintenance, which directly increases FF.
*Increased GFR, increased RPF, increased FF*
- This pattern suggests **hypervolemia** or increased renal perfusion, which directly contradicts the patient's severe dehydration.
- Both GFR and RPF are expected to decrease in volume depletion, not increase.
*Increased GFR, decreased RPF, increased FF*
- An increase in GFR is physiologically impossible given the patient's severe volume depletion and reduced renal perfusion.
- While FF does increase in dehydration, this occurs in the context of **both GFR and RPF being decreased**, not with an increased GFR.
Angiotensin converting enzyme function US Medical PG Question 8: A 69-year-old woman is admitted to the hospital with substernal, crushing chest pain. She is emergently moved to the cardiac catheterization lab where she undergoes cardiac angiography. Angiography reveals that the diameter of her left anterior descending artery (LAD) is 50% of normal. If her blood pressure, LAD length, and blood viscosity have not changed, which of the following represents the most likely change in LAD flow from baseline?
- A. Decreased by 93.75% (Correct Answer)
- B. Increased by 6.25%
- C. Decreased by 25%
- D. Decreased by 87.5%
- E. Increased by 25%
Angiotensin converting enzyme function Explanation: ***Decreased by 93.75%***
- This option is correct based on Poiseuille's Law, which states that flow is proportional to the **fourth power of the radius (r^4)**. A 50% decrease in diameter means a 50% decrease in radius (0.5r).
- The new flow would be (0.5)^4 = 0.0625 times the original flow. Therefore, the decrease in flow is 1 - 0.0625 = 0.9375, or **93.75%**.
*Increased by 6.25%*
- This answer incorrectly suggests an **increase** in flow, which is contrary to the effect of a narrowed artery.
- While 6.25% represents the new flow as a percentage of baseline (since 0.0625 = 6.25%), the vessel stenosis causes a **decrease**, not an increase in flow.
*Decreased by 25%*
- This calculation might arise from considering a linear relationship (e.g., radius decreases by 50%, so flow decreases by 50% of 50%, which is incorrect).
- It does not account for the **fourth power relationship** between radius and flow according to Poiseuille's Law.
*Decreased by 87.5%*
- This percentage represents a calculation error, likely from misapplying the fourth power relationship or confusing the calculation steps.
- It does not accurately reflect the dramatic reduction in flow caused by a 50% reduction in vessel diameter.
*Increased by 25%*
- This option implies a significant increase in blood flow, which would not happen with a **stenosed artery**.
- It completely contradicts the physiological response to a **narrowed vessel**.
Angiotensin converting enzyme function US Medical PG Question 9: A 63-year-old man comes to the physician because of fatigue and muscle cramps for 6 weeks. He also noticed several episodes of tingling around the mouth and in the fingers and toes. He has osteoarthritis of his knees and hypertension. Current medications include ibuprofen and ramipril. He has smoked one pack of cigarettes daily for 35 years. Tapping over the facial nerve area in front of the ear elicits twitching of the facial muscles on the same side of the face. His serum alkaline phosphatase activity is 66 U/L. An ECG shows sinus rhythm with a prolonged QT interval. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Medication side effect
- B. Ectopic hormone production
- C. Vitamin D deficiency
- D. Destruction of parathyroid glands (Correct Answer)
- E. Albright hereditary osteodystrophy
Angiotensin converting enzyme function Explanation: ***Destruction of parathyroid glands***
- The patient presents with **fatigue**, **muscle cramps**, and **paresthesias** (tingling around the mouth, fingers, and toes), which are classic symptoms of **hypocalcemia**.
- The positive **Chvostek's sign** (tapping over the facial nerve leading to facial muscle twitching) further confirms hypocalcemia, and a **prolonged QT interval** on ECG is also a known manifestation of low calcium levels. Destruction of the parathyroid glands (e.g., due to surgery, autoimmune disease, or radiation) leads to primary hypoparathyroidism and subsequent hypocalcemia.
*Medication side effect*
- While some medications can affect calcium levels, neither **ibuprofen** nor **ramipril** are typically associated with profound hypocalcemia leading to such prominent symptoms.
- The constellation of symptoms and signs (Chvostek's sign, prolonged QT) strongly points to an underlying calcium metabolism disorder, not a common drug side effect.
*Ectopic hormone production*
- **Ectopic hormone production** (e.g., PTHrP from tumors) usually causes **hypercalcemia**, not hypocalcemia, by mimicking parathyroid hormone action.
- Tumors that could lead to hypocalcemia are rare and usually involve extensive osteoblastic metastases consuming calcium, which is not suggested by the patient's presentation.
*Vitamin D deficiency*
- **Vitamin D deficiency** primarily causes osteomalacia in adults and rickets in children and can lead to **secondary hyperparathyroidism** as the body tries to compensate for low calcium.
- While severe vitamin D deficiency can cause some hypocalcemia symptoms, it doesn't typically present with the acute, symptomatic hypocalcemia signs like Chvostek's sign and prolonged QT interval in this direct manner without other signs of bone disease.
*Albright hereditary osteodystrophy*
- **Albright hereditary osteodystrophy** is a genetic disorder causing **pseudohypoparathyroidism**, where the body is resistant to PTH, leading to hypocalcemia.
- This condition is often associated with characteristic physical features such as **short stature**, **brachydactyly**, and **obesity**, which are not mentioned in this patient.
Angiotensin converting enzyme function US Medical PG Question 10: A 23-year-old woman presents to a medical clinic for a follow-up visit. She initially came with complaints of recurrent headaches and darkening of her knuckles and skin creases, which first began 6 months ago after she underwent bilateral adrenalectomy. Today, she says that she frequently bumps into people and objects while walking. Which of the following mechanisms most likely account for this patient’s symptoms?
- A. Feedback inhibition by an exogenous source
- B. Hormonal receptor downregulation
- C. Dissemination of tumor to distant sites
- D. Ectopic secretion of a trophic hormone
- E. Loss of a regulatory process (Correct Answer)
Angiotensin converting enzyme function Explanation: ***Loss of a regulatory process***
- This patient likely has **Nelson's syndrome**, which develops after bilateral adrenalectomy for **Cushing's disease**. The removal of adrenal glands eliminates the **negative feedback** normally exerted by cortisol on the pituitary gland.
- This leads to unchecked growth of a pre-existing corticotroph adenoma, causing excessive **ACTH** secretion. The high ACTH levels result in **hyperpigmentation** (darkening knuckles and skin creases) due to its melanocyte-stimulating properties, and the growing tumor can cause **visual field defects** (bumping into objects) due to compression of the optic chiasm.
*Feedback inhibition by an exogenous source*
- This mechanism involves the suppression of endogenous hormone production by an external agent, such as corticosteroid medication.
- In this case, the patient's symptoms are due to a lack of feedback, not an excess.
*Hormonal receptor downregulation*
- This process involves a decrease in the number or sensitivity of receptors in response to prolonged high hormone levels, making the cells less responsive.
- While relevant in some endocrine disorders, it does not explain the pituitary tumor growth or the specific constellation of symptoms seen here.
*Dissemination of tumor to distant sites*
- This option refers to metastasis, where a cancer spreads from its primary location to other parts of the body.
- Although the pituitary adenoma grows, Nelson's syndrome is primarily characterized by local tumor expansion and hormonal effects, not distant metastasis.
*Ectopic secretion of a trophic hormone*
- Ectopic secretion refers to the production of hormones by tissues that do not normally produce them, often associated with paraneoplastic syndromes.
- In this scenario, the ACTH is secreted by an adenoma within the pituitary gland, which is its normal site of production, albeit in an unregulated and excessive manner.
More Angiotensin converting enzyme function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.