Venous pressure and return US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Venous pressure and return. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Venous pressure and return US Medical PG Question 1: A 40-year-old female volunteers for an invasive study to measure her cardiac function. She has no previous cardiovascular history and takes no medications. With the test subject at rest, the following data is collected using blood tests, intravascular probes, and a closed rebreathing circuit:
Blood hemoglobin concentration 14 g/dL
Arterial oxygen content 0.22 mL O2/mL
Arterial oxygen saturation 98%
Venous oxygen content 0.17 mL O2/mL
Venous oxygen saturation 78%
Oxygen consumption 250 mL/min
The patient's pulse is 75/min, respiratory rate is 14/ min, and blood pressure is 125/70 mm Hg. What is the cardiac output of this volunteer?
- A. Body surface area is required to calculate cardiac output.
- B. Stroke volume is required to calculate cardiac output.
- C. 250 mL/min
- D. 5.0 L/min (Correct Answer)
- E. 50 L/min
Venous pressure and return Explanation: ***5.0 L/min***
- Cardiac output can be calculated using the **Fick principle**: Cardiac Output $(\text{CO}) = \frac{{\text{Oxygen Consumption}}}{{\text{Arterial } \text{O}_2 \text{ Content} - \text{Venous O}_2 \text{ Content}}}$.
- Given Oxygen Consumption = 250 mL/min, Arterial O$_2$ Content = 0.22 mL/mL, and Venous O$_2$ Content = 0.17 mL/mL. Thus, CO = $\frac{{250 \text{ mL/min}}}{{(0.22 - 0.17) \text{ mL } \text{O}_2/\text{mL blood}}} = \frac{{250 \text{ mL/min}}}{{0.05 \text{ mL } \text{O}_2/\text{mL blood}}} = 5000 \text{ mL/min } = 5.0 \text{ L/min}$.
*Body surface area is required to calculate cardiac output.*
- **Body surface area (BSA)** is used to calculate **cardiac index**, which is cardiac output normalized to body size, but not cardiac output directly.
- While a normal cardiac output might be compared to a patient's BSA for context, it is not a necessary component for calculating the absolute cardiac output.
*Stroke volume is required to calculate cardiac output.*
- Cardiac output can be calculated as **Stroke Volume (SV) x Heart Rate (HR)**. However, stroke volume is not provided directly in this question.
- The Fick principle allows for the calculation of cardiac output **without explicit knowledge of stroke volume** or heart rate, using oxygen consumption and arteriovenous oxygen difference.
*250 mL/min*
- 250 mL/min represents the **oxygen consumption**, not the cardiac output.
- Cardiac output is the volume of blood pumped by the heart per minute, which is influenced by both oxygen consumption and the difference in oxygen content between arterial and venous blood.
*50 L/min*
- A cardiac output of 50 L/min is an **extremely high and physiologically impossible** value for a resting individual.
- This value is 10 times higher than the calculated cardiac output and typically represents a calculation error.
Venous pressure and return US Medical PG Question 2: A 27-year-old man is brought to the emergency department 30 minutes after being shot in the abdomen during a violent altercation. His temperature is 36.5°C (97.7°F), pulse is 118/min and regular, and blood pressure is 88/65 mm Hg. Examination shows cool extremities. Abdominal examination shows a 2.5-cm entrance wound in the left upper quadrant at the midclavicular line, below the left costal margin. Focused ultrasound shows free fluid in the left upper quadrant. Which of the following sets of hemodynamic changes is most likely in this patient?
Cardiac output (CO) | Pulmonary capillary wedge pressure (PCWP) | Systemic vascular resistance (SVR) | Central venous pressure (CVP)
- A. ↑ ↓ ↓ ↓
- B. ↓ ↓ ↑ ↑
- C. ↓ ↓ ↓ ↓
- D. ↓ ↓ ↑ ↓ (Correct Answer)
- E. ↓ ↑ ↑ ↑
Venous pressure and return Explanation: ***↓ ↓ ↑ ↓***
- This patient is in **hypovolemic shock** due to hemorrhage, leading to decreased **cardiac output (CO)** and **pulmonary capillary wedge pressure (PCWP)** due to reduced preload.
- The body compensates for hypovolemia by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, while **central venous pressure (CVP)** decreases due to the depleted blood volume.
*↑ ↓ ↓ ↓*
- An increased **cardiac output** is inconsistent with hypovolemic shock, where the heart's ability to pump blood is compromised by a lack of circulating volume.
- While **PCWP**, **SVR**, and **CVP** decreasing could be seen in some forms of shock, the elevated CO rules out hypovolemic shock.
*↓ ↓ ↑ ↑*
- An elevated **central venous pressure (CVP)** is inconsistent with hypovolemic shock, as CVP reflects right atrial pressure and would be low due to decreased blood volume.
- While other parameters such as **CO** and **PCWP** decreasing and **SVR** increasing can be seen in hypovolemic shock, the increased CVP suggests a different hemodynamic state, like cardiogenic shock.
*↓ ↓ ↓ ↓*
- A decrease in **systemic vascular resistance (SVR)** is characteristic of **distributive shock** (e.g., septic or neurogenic shock), not hypovolemic shock, where compensatory vasoconstriction would lead to increased SVR.
- While **CO**, **PCWP**, and **CVP** would decrease due to overall poor perfusion, the SVR response differentiates it from hypovolemic shock.
*↓ ↑ ↑ ↑*
- An elevated **pulmonary capillary wedge pressure (PCWP)** and **central venous pressure (CVP)** indicate increased fluid volume or cardiac dysfunction, which is contrary to the reduced preload seen in hypovolemic shock.
- While **cardiac output (CO)** may decrease in cardiogenic shock, the other elevated pressures point away from a primary hypovolemic cause.
Venous pressure and return US Medical PG Question 3: A 60-year-old male engineer who complains of shortness of breath when walking a few blocks undergoes a cardiac stress test because of concern for coronary artery disease. During the test he asks his cardiologist about what variables are usually used to quantify the functioning of the heart. He learns that one of these variables is stroke volume. Which of the following scenarios would be most likely to lead to a decrease in stroke volume?
- A. Anxiety
- B. Heart failure (Correct Answer)
- C. Exercise
- D. Pregnancy
- E. Digitalis
Venous pressure and return Explanation: ***Heart failure***
- In **heart failure**, the heart's pumping ability is impaired, leading to a reduced **ejection fraction** and thus a decreased **stroke volume**.
- The weakened myocardium cannot effectively contract to expel the normal volume of blood, resulting in lower blood output per beat.
*Anxiety*
- **Anxiety** typically causes an increase in **sympathetic nervous system** activity, leading to increased heart rate and myocardial contractility.
- This often results in a temporary **increase in stroke volume** due to enhanced cardiac performance, not a decrease.
*Exercise*
- During **exercise**, there is a significant **increase in venous return** and sympathetic stimulation, leading to increased **end-diastolic volume** and contractility.
- This physiological response causes a substantial **increase in stroke volume** to meet the body's higher oxygen demands.
*Pregnancy*
- **Pregnancy** leads to significant **physiological adaptations** to accommodate the growing fetus, including a substantial increase in **blood volume**.
- This increased blood volume and cardiac output result in an **increase in stroke volume** to maintain adequate perfusion for both mother and fetus.
*Digitalis*
- **Digitalis** is a cardiac glycoside that **increases intracellular calcium** in myocardial cells, enhancing the **force of contraction**.
- This positive inotropic effect leads to an **increased stroke volume** by improving the heart's pumping efficiency.
Venous pressure and return US Medical PG Question 4: A 32-year-old woman comes to the physician for a screening health examination that is required for scuba diving certification. The physician asks her to perform a breathing technique: following deep inspiration, she is instructed to forcefully exhale against a closed airway and contract her abdominal muscles while different cardiovascular parameters are evaluated. Which of the following effects is most likely after 10 seconds in this position?
- A. Decreased intra-abdominal pressure
- B. Decreased left ventricular stroke volume (Correct Answer)
- C. Decreased pulse rate
- D. Decreased systemic vascular resistance
- E. Increased venous return to left atrium
Venous pressure and return Explanation: ***Decreased left ventricular stroke volume***
- After 10 seconds of performing the **Valsalva maneuver**, the increased intrathoracic pressure significantly reduces **venous return** to the heart.
- Reduced venous return leads to decreased **ventricular filling** (preload), which in turn diminishes **left ventricular stroke volume** and cardiac output.
*Decreased intra-abdominal pressure*
- The instruction to "contract her abdominal muscles" during forceful exhalation against a closed airway (Valsalva maneuver) directly leads to an **increase** in **intra-abdominal pressure**, not a decrease.
- This increase in intra-abdominal pressure further impedes venous return from the lower extremities to the heart.
*Decreased pulse rate*
- In the initial phase of the Valsalva maneuver (first 5-10 seconds), the decrease in cardiac output triggers a **reflex tachycardia** to maintain blood pressure, leading to an **increased pulse rate**.
- A decrease in pulse rate (bradycardia) is more characteristic of the release phase, not during the sustained strain.
*Decreased systemic vascular resistance*
- During the Valsalva maneuver, the body attempts to compensate for the drop in cardiac output and blood pressure by increasing **sympathetic tone**, which causes **vasoconstriction** and thus **increases systemic vascular resistance**.
- A decrease in systemic vascular resistance would further drop blood pressure and is not the physiological response during this phase.
*Increased venous return to left atrium*
- The Valsalva maneuver dramatically **reduces venous return** to both the right and left atria due to the high intrathoracic pressure compressing the great veins.
- This decreased venous return is the primary mechanism leading to the subsequent fall in cardiac output during the maneuver.
Venous pressure and return US Medical PG Question 5: A 37-year-old man is brought to the emergency department following a motor vehicle collision. His temperature is 38.1°C (100.6°F), pulse is 39/min, respirations are 29/min, and blood pressure is 58/42 mm Hg. There is no improvement in his blood pressure despite adequate fluid resuscitation. A drug is administered that causes increased IP3 concentrations in arteriolar smooth muscle cells and increased cAMP concentrations in cardiac myocytes. This drug only has a negligible effect on cAMP concentration in bronchial smooth muscle cells. Which of the following sets of cardiovascular changes is most likely following administration of this drug?
- A. Heart Rate ↓ Blood Pressure ↓ Systemic Vascular Resistance ↑
- B. Heart Rate ↑ Blood Pressure ↑ Systemic Vascular Resistance ↓
- C. Heart Rate ↑ Blood Pressure ↑ Systemic Vascular Resistance ↑ (Correct Answer)
- D. Heart Rate ↑ Blood Pressure ↓ Systemic Vascular Resistance ↓
- E. Heart Rate No change Blood Pressure ↑ Systemic Vascular Resistance ↑
Venous pressure and return Explanation: ***Heart Rate ↑ Blood Pressure ↑ Systemic Vascular Resistance ↑***
- This drug profile describes **norepinephrine**, which has potent **α1 (increases IP3)** and **β1 (increases cAMP in heart)** agonist activity with minimal β2 effects.
- The increase in **IP3 in arteriolar smooth muscle cells** leads to **vasoconstriction** via increased intracellular calcium, resulting in markedly **increased systemic vascular resistance (SVR)**.
- The increase in **cAMP in cardiac myocytes** provides **positive inotropy (contractility) and chronotropy (heart rate)** through β1 receptor stimulation.
- The combined effects of increased cardiac output and increased SVR result in a **significant increase in blood pressure**, making this the ideal vasopressor for distributive shock.
- Note: While baroreceptor reflexes might blunt the heart rate increase in normal states, in severe shock with autonomic dysfunction, the direct β1 effect predominates.
*Heart Rate ↓ Blood Pressure ↓ Systemic Vascular Resistance ↑*
- An increase in **IP3 in arteriolar smooth muscle cells** would cause **vasoconstriction (increased SVR)**, which tends to increase blood pressure, not decrease it.
- An increase in **cAMP in cardiac myocytes** would increase heart rate and contractility through β1 stimulation, not decrease them.
*Heart Rate ↑ Blood Pressure ↑ Systemic Vascular Resistance ↓*
- While heart rate and blood pressure would increase due to the drug's effects on cardiac myocytes, the increased IP3 in arteriolar smooth muscle cells would lead to **vasoconstriction** and thus an **increase in systemic vascular resistance**, not a decrease.
- A decrease in systemic vascular resistance would typically lower blood pressure unless cardiac output increases significantly to compensate.
*Heart Rate ↑ Blood Pressure ↓ Systemic Vascular Resistance ↓*
- The drug's mechanism of action, particularly the increase in **IP3 leading to vasoconstriction**, is fundamentally inconsistent with a decrease in both blood pressure and systemic vascular resistance.
- While heart rate would increase via β1 stimulation, decreased BP with decreased SVR contradicts the described α1-mediated vascular effects.
*Heart Rate No change Blood Pressure ↑ Systemic Vascular Resistance ↑*
- The increase in **cAMP in cardiac myocytes** directly stimulates **β1 adrenergic receptors**, leading to increased **heart rate**, not "no change."
- While **blood pressure** and **systemic vascular resistance** would correctly increase, the absence of heart rate change is inconsistent with the drug's β1 agonist effects on the heart.
Venous pressure and return US Medical PG Question 6: A 71-year-old man presents to the emergency department with severe substernal chest pain. An initial EKG demonstrates ST elevation in leads V2, V3, V4, and V5 with reciprocal changes. The patient is started on aspirin and heparin and is transferred to the cardiac catheterization lab. The patient recovers over the next several days. On the floor, the patient complains of feeling very fatigued and feels too weak to ambulate even with the assistance of physical therapy. Chest radiography reveals an enlarged cardiac silhouette with signs of fluid bilaterally in the lung bases. His temperature is 98.4°F (36.9°C), blood pressure is 85/50 mmHg, pulse is 110/min, respirations are 13/min, and oxygen saturation is 97% on room air. Which of the following would be expected to be seen in this patient?
- A. Decreased systemic vascular resistance
- B. Increased venous oxygen content
- C. Increased ejection fraction
- D. Decreased tissue oxygen extraction
- E. Increased pulmonary capillary wedge pressure (Correct Answer)
Venous pressure and return Explanation: ***Increased pulmonary capillary wedge pressure***
- The patient's symptoms of **fatigue**, **weakness**, **hypotension**, **tachycardia**, and **pulmonary congestion** (enlarged cardiac silhouette, bilateral pleural effusions) after a significant myocardial infarction are highly suggestive of **cardiogenic shock**.
- In cardiogenic shock, the heart's pumping ability is severely compromised, leading to **increased end-diastolic filling pressures** in the left ventricle, which is reflected as an elevated **pulmonary capillary wedge pressure (PCWP)**.
*Decreased systemic vascular resistance*
- **Decreased systemic vascular resistance (SVR)** is a hallmark of **distributive shock**, such as septic shock, where widespread vasodilation occurs.
- In **cardiogenic shock**, the body typically tries to compensate for reduced cardiac output by **increasing SVR** to maintain blood pressure, although this compensation may be overwhelmed, leading to hypotension.
*Increased venous oxygen content*
- **Increased mixed venous oxygen saturation (SvO2)** or **venous oxygen content** is seen when tissues are not adequately extracting oxygen, either due to shunt physiology or when oxygen delivery far exceeds demand.
- In **cardiogenic shock**, tissue oxygen demand often exceeds delivery due to severely impaired cardiac output, leading to **increased oxygen extraction** by tissues and thus **decreased venous oxygen content**.
*Increased ejection fraction*
- The patient experienced a **large myocardial infarction (ST elevation in V2-V5)**, indicating substantial damage to the left ventricle.
- This damage would severely impair the heart's pumping function, leading to a **decreased ejection fraction**, which is characteristic of **cardiogenic shock**.
*Decreased tissue oxygen extraction*
- **Decreased tissue oxygen extraction** would imply that tissues are not properly utilizing the delivered oxygen, or that oxygen delivery is so high that tissues don't need to extract as much.
- In **cardiogenic shock**, cardiac output is severely reduced, leading to **inadequate oxygen delivery** to tissues, forcing them to **maximally extract oxygen** from the blood to meet metabolic demands.
Venous pressure and return US Medical PG Question 7: A 64-year-old man who recently immigrated to the United States from Haiti comes to the physician because of a 3-week history of progressively worsening exertional dyspnea and fatigue. For the past few days, he has also had difficulty lying flat due to trouble breathing. Over the past year, he has had intermittent fever, night sweats, and cough but he has not been seen by a physician for evaluation of these symptoms. His temperature is 37.8°C (100°F). An x-ray of the chest is shown. Further evaluation of this patient is most likely to show which of the following findings?
- A. Head bobbing in synchrony with heart beat
- B. Jugular venous distention on inspiration (Correct Answer)
- C. Prominent "a" wave on jugular venous pressure tracing
- D. Elimination of S2 heart sound splitting with inspiration
- E. Crescendo-decrescendo systolic ejection murmur
Venous pressure and return Explanation: ***Jugular venous distention on inspiration***
- The patient's symptoms (dyspnea, fatigue, orthopnea, fever, night sweats, cough), Haitian origin, and chest X-ray findings (likely indicating **pericardial effusion** or **constrictive pericarditis**) are highly suggestive of **tuberculosis** involving the pericardium.
- **Kussmaul's sign** (paradoxical rise in JVP with inspiration) is a classic finding in **constrictive pericarditis** and **restrictive cardiomyopathy**, indicating impaired right ventricular filling.
*Head bobbing in synchrony with heart beat*
- This symptom, also known as **de Musset's sign**, is associated with severe **aortic regurgitation**.
- There are no other clinical signs to suggest aortic regurgitation, and the patient's symptoms point towards a restrictive or constrictive cardiac pathology.
*Prominent "a" wave on jugular venous pressure tracing*
- A prominent "a" wave (atrial contraction against a closed tricuspid valve) is typically seen in **tricuspid stenosis**, **pulmonary hypertension**, or certain types of **right ventricular hypertrophy**, none of which are suggested here.
- The findings in this patient are more consistent with impaired ventricular filling due to pericardial disease affecting both atria and ventricles.
*Elimination of S2 heart sound splitting with inspiration*
- **Physiologic splitting of S2** widens with inspiration due to delayed pulmonary valve closure.
- The **elimination of S2 splitting** or a paradoxically split S2 is associated with conditions like **aortic stenosis** or **left bundle branch block**, which are not indicated by the patient's presentation.
*Crescendo-decrescendo systolic ejection murmur*
- This type of murmur is characteristic of **aortic stenosis** or **pulmonic stenosis**.
- The patient's symptoms are more consistent with a pericardial process affecting cardiac filling rather than outflow obstruction.
Venous pressure and return US Medical PG Question 8: A 64-year-old male with a history of coronary artery disease, hypertension, hyperlipidemia, and type II diabetes presents to his primary care physician with increasing shortness of breath and ankle swelling over the past month. Which of the following findings is more likely to be seen in left-sided heart failure and less likely to be seen in right-sided heart failure?
- A. Abdominal fullness
- B. Basilar crackles on pulmonary auscultation (Correct Answer)
- C. Hepatojugular reflex
- D. Increased ejection fraction on echocardiogram
- E. Lower extremity edema
Venous pressure and return Explanation: ***Basilar crackles on pulmonary auscultation***
- **Left-sided heart failure** leads to increased pressure in the pulmonary veins, causing fluid to leak into the **pulmonary interstitium and alveoli**, manifesting as **basilar crackles** on auscultation.
- This symptom is a direct result of **pulmonary congestion** and edema, which is not characteristic of isolated right-sided heart failure.
*Abdominal fullness*
- **Abdominal fullness** is typically a symptom of **right-sided heart failure**, due to **venous congestion** in the splanchnic circulation, leading to hepatomegaly and ascites.
- While it can occur in severe biventricular failure, it is not a primary or earlier sign of isolated left-sided heart failure.
*Hepatojugular reflex*
- The **hepatojugular reflex** is a sign of **right ventricular dysfunction** and **elevated right atrial pressure**, indicating systemic venous congestion.
- It is elicited by applying pressure to the liver, which causes a temporary increase in jugular venous distention.
*Increased ejection fraction on echocardiogram*
- **Heart failure**, whether left- or right-sided, is characterized by a **reduced (or preserved but not increased)** ejection fraction, reflecting impaired pumping ability.
- An **increased ejection fraction** would indicate supra-normal cardiac function and is not associated with heart failure.
*Lower extremity edema*
- **Lower extremity edema** is a hallmark symptom of **right-sided heart failure**, as venous congestion leads to fluid accumulation in the peripheral tissues.
- While present in biventricular failure, it is not a primary or early symptom of isolated left-sided heart failure.
Venous pressure and return US Medical PG Question 9: A 37-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He suffered multiple deep lacerations and experienced significant blood loss during transport. In the emergency department, his temperature is 98.6°F (37°C), blood pressure is 102/68 mmHg, pulse is 112/min, and respirations are 22/min. His lacerations are sutured and he is given 2 liters of saline by large bore intravenous lines. Which of the following changes will occur in this patient's cardiac physiology due to this intervention?
- A. Increased cardiac output and unchanged right atrial pressure
- B. Decreased cardiac output and increased right atrial pressure
- C. Increased cardiac output and decreased right atrial pressure
- D. Increased cardiac output and increased right atrial pressure (Correct Answer)
- E. Decreased cardiac output and decreased right atrial pressure
Venous pressure and return Explanation: ***Increased cardiac output and increased right atrial pressure***
- The patient experienced significant blood loss, leading to a **decreased preload** and subsequent **reduced cardiac output**. Volume resuscitation with saline directly increases the **intravascular volume** which bolsters **venous return** and **right atrial pressure**.
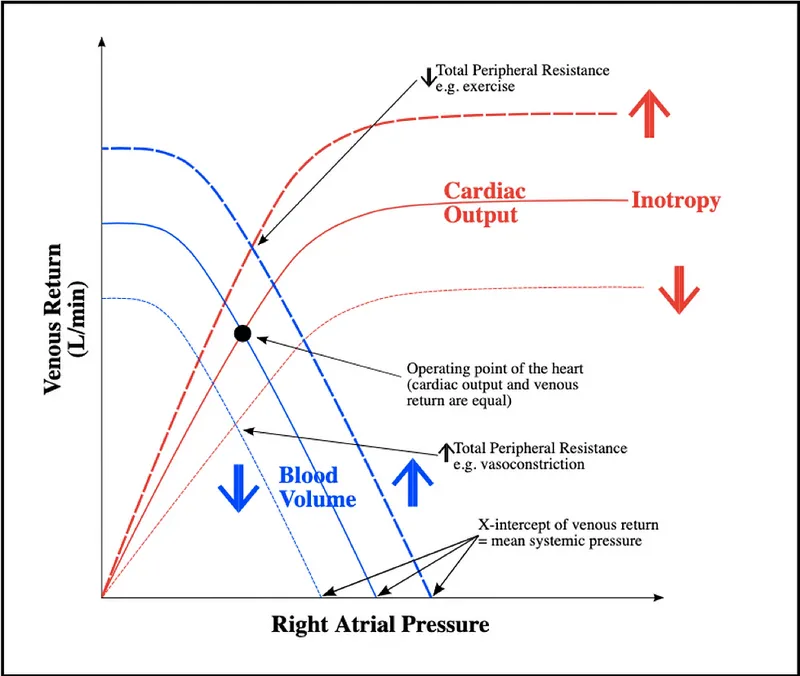
- According to the **Frank-Starling mechanism**, increased right atrial pressure (a measure of preload) results in an increase in ventricular stretch and a more forceful contraction, thereby increasing **stroke volume** and **cardiac output**.
*Increased cardiac output and unchanged right atrial pressure*
- While fluid administration will increase **cardiac output** by improving preload, it will also directly lead to an increase in **right atrial pressure** due to the augmented venous return.
- An unchanged right atrial pressure would imply no significant increase in central venous volume, which contradicts the effect of a large volume fluid resuscitation.
*Decreased cardiac output and increased right atrial pressure*
- This scenario is unlikely because increasing **intravascular volume** through fluid resuscitation typically aims to raise **cardiac output** by optimizing preload, not decrease it.
- A decrease in cardiac output despite increased right atrial pressure could indicate **cardiac pump failure**, which is not suggested by the clinical picture of hypovolemic shock treated with fluids.
*Increased cardiac output and decreased right atrial pressure*
- An increase in **cardiac output** as a result of fluid resuscitation is expected, but a **decreased right atrial pressure** would contradict the mechanism of increased venous return and volume expansion.
- Decreased right atrial pressure would typically indicate ongoing volume loss or inadequate fluid resuscitation to restore central venous volume.
*Decreased cardiac output and decreased right atrial pressure*
- Both decreasing **cardiac output** and decreasing **right atrial pressure** indicate a worsening state of **hypovolemia** or an inadequate response to fluid resuscitation.
- The administration of 2 liters of saline is intended to correct the hypovolemia and improve cardiodynamics, not to worsen them.
Venous pressure and return US Medical PG Question 10: A 19-year-old man presents to the clinic with a complaint of increasing shortness of breath for the past 2 years. His shortness of breath is associated with mild chest pain and occasional syncopal attacks during strenuous activity. There is no history of significant illness in the past, however, one of his uncles had similar symptoms when he was his age and died while playing basketball a few years later. He denies alcohol use, tobacco consumption, and the use of recreational drugs. On examination, pulse rate is 76/min and is regular and bounding; blood pressure is 130/70 mm Hg. A triple apical impulse is observed on the precordium and a systolic ejection crescendo-decrescendo murmur is audible between the apex and the left sternal border along with a prominent fourth heart sound. The physician then asks the patient to take a deep breath, close his mouth, and pinch his nose and try to breathe out without allowing his cheeks to bulge out. In doing so, the intensity of the murmur increases. Which of the following hemodynamic changes would be observed first during this maneuver?
- A. ↓ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↓ Parasympathetic Outflow
- B. ↑ Mean Arterial Pressure, ↓ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow (Correct Answer)
- C. ↑ Mean Arterial Pressure, ↓ Heart rate, ↓ Baroreceptor activity, ↑ Parasympathetic Outflow
- D. ↑ Mean Arterial Pressure, ↑ Heart rate, ↓ Baroreceptor activity, ↓ Parasympathetic Outflow
- E. ↑ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow
Venous pressure and return Explanation: **↑ Mean Arterial Pressure, ↓ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow**
- This maneuver is the **Valsalva Maneuver**, which involves forced expiration against a closed glottis. It causes a transient increase in **intrathoracic pressure**, compressing the great vessels and temporarily increasing **mean arterial pressure**.
- The initial rise in blood pressure is detected by **baroreceptors**, leading to a reflex decrease in **heart rate** via increased **parasympathetic outflow**.
*↓ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↓ Parasympathetic Outflow*
- This option describes changes more typical of the **later phases** of a Valsalva maneuver (Phase 2), where venous return and cardiac output decrease, leading to a fall in MAP and a compensatory increase in heart rate.
- It does not represent the **immediate hemodynamic changes** (Phase 1) that occur during the initial strain of the maneuver.
*↑ Mean Arterial Pressure, ↓ Heart rate, ↓ Baroreceptor activity, ↑ Parasympathetic Outflow*
- A decrease in **baroreceptor activity** would typically lead to an *increase* in heart rate and a *decrease* in parasympathetic outflow, contrary to the initial response to increased blood pressure.
- The initial increase in MAP correctly leads to *increased* baroreceptor activity.
*↑ Mean Arterial Pressure, ↑ Heart rate, ↓ Baroreceptor activity, ↓ Parasympathetic Outflow*
- An increase in **mean arterial pressure** (MAP) would reflexively cause a *decrease* in heart rate and an *increase* in parasympathetic outflow, mediated by *increased* baroreceptor activity, not decreased activity.
- Therefore, the proposed changes in heart rate, baroreceptor activity, and parasympathetic outflow are inconsistent with an initial increase in MAP.
*↑ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow*
- While an increase in **mean arterial pressure** does lead to an increase in **baroreceptor activity** and **parasympathetic outflow**, the reflexive response to this increased pressure is a *decrease* in **heart rate**, not an increase.
- An increased heart rate combined with increased parasympathetic outflow is contradictory, as sympathetic and parasympathetic systems typically exert opposing effects on heart rate.
More Venous pressure and return US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.