Shock states pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Shock states pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Shock states pathophysiology US Medical PG Question 1: A 24-year-old man is rushed to the emergency room after he was involved in a motor vehicle accident. He says that he is having difficulty breathing and has right-sided chest pain, which he describes as 8/10, sharp in character, and worse with deep inspiration. His vitals are: blood pressure 90/65 mm Hg, respiratory rate 30/min, pulse 120/min, temperature 37.2°C (99.0°F). On physical examination, patient is alert and oriented but in severe distress. There are multiple bruises over the anterior chest wall. There is also significant jugular venous distention and the presence of subcutaneous emphysema at the base of the neck. There is an absence of breath sounds on the right and hyperresonance to percussion. A bedside chest radiograph shows evidence of a collapsed right lung with a depressed right hemidiaphragm and tracheal deviation to the left. Which of the following findings is the strongest indicator of cardiogenic shock in this patient?
- A. Jugular venous distention (Correct Answer)
- B. Hyperresonance to percussion
- C. Subcutaneous emphysema
- D. No right chest raise
- E. Tracheal shift to the left
Shock states pathophysiology Explanation: ***Jugular venous distention***
- In this trauma patient with tension pneumothorax, **jugular venous distention (JVD)** is the strongest indicator that the patient is developing **obstructive shock** with cardiovascular compromise.
- JVD indicates **impaired venous return** to the heart due to increased intrathoracic pressure compressing the vena cava and right atrium.
- While this is technically **obstructive shock** (not pure cardiogenic shock), JVD represents the cardiovascular manifestation indicating that the mechanical obstruction is now critically affecting cardiac filling and output.
- Among the options listed, **JVD is the only finding that directly reflects cardiovascular compromise** and impending circulatory collapse.
*Hyperresonance to percussion*
- This finding indicates **air in the pleural space**, characteristic of pneumothorax.
- While it confirms the diagnosis of pneumothorax, it is a **respiratory finding** rather than a direct indicator of cardiovascular compromise or shock state.
*Subcutaneous emphysema*
- This indicates **air in subcutaneous tissues** from chest wall injury or air leak.
- It confirms significant chest trauma but does not directly indicate the severity of cardiovascular compromise or shock.
*Tracheal shift to the left*
- **Tracheal deviation** away from the affected side is a classic sign of **tension pneumothorax** indicating mediastinal shift.
- While this confirms tension physiology, it is primarily an **anatomical/structural finding** rather than a direct hemodynamic indicator like JVD, which specifically reflects impaired venous return and cardiovascular compromise.
Shock states pathophysiology US Medical PG Question 2: A 27-year-old man is brought to the emergency department 30 minutes after being shot in the abdomen during a violent altercation. His temperature is 36.5°C (97.7°F), pulse is 118/min and regular, and blood pressure is 88/65 mm Hg. Examination shows cool extremities. Abdominal examination shows a 2.5-cm entrance wound in the left upper quadrant at the midclavicular line, below the left costal margin. Focused ultrasound shows free fluid in the left upper quadrant. Which of the following sets of hemodynamic changes is most likely in this patient?
Cardiac output (CO) | Pulmonary capillary wedge pressure (PCWP) | Systemic vascular resistance (SVR) | Central venous pressure (CVP)
- A. ↑ ↓ ↓ ↓
- B. ↓ ↓ ↑ ↑
- C. ↓ ↓ ↓ ↓
- D. ↓ ↓ ↑ ↓ (Correct Answer)
- E. ↓ ↑ ↑ ↑
Shock states pathophysiology Explanation: ***↓ ↓ ↑ ↓***
- This patient is in **hypovolemic shock** due to hemorrhage, leading to decreased **cardiac output (CO)** and **pulmonary capillary wedge pressure (PCWP)** due to reduced preload.
- The body compensates for hypovolemia by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, while **central venous pressure (CVP)** decreases due to the depleted blood volume.
*↑ ↓ ↓ ↓*
- An increased **cardiac output** is inconsistent with hypovolemic shock, where the heart's ability to pump blood is compromised by a lack of circulating volume.
- While **PCWP**, **SVR**, and **CVP** decreasing could be seen in some forms of shock, the elevated CO rules out hypovolemic shock.
*↓ ↓ ↑ ↑*
- An elevated **central venous pressure (CVP)** is inconsistent with hypovolemic shock, as CVP reflects right atrial pressure and would be low due to decreased blood volume.
- While other parameters such as **CO** and **PCWP** decreasing and **SVR** increasing can be seen in hypovolemic shock, the increased CVP suggests a different hemodynamic state, like cardiogenic shock.
*↓ ↓ ↓ ↓*
- A decrease in **systemic vascular resistance (SVR)** is characteristic of **distributive shock** (e.g., septic or neurogenic shock), not hypovolemic shock, where compensatory vasoconstriction would lead to increased SVR.
- While **CO**, **PCWP**, and **CVP** would decrease due to overall poor perfusion, the SVR response differentiates it from hypovolemic shock.
*↓ ↑ ↑ ↑*
- An elevated **pulmonary capillary wedge pressure (PCWP)** and **central venous pressure (CVP)** indicate increased fluid volume or cardiac dysfunction, which is contrary to the reduced preload seen in hypovolemic shock.
- While **cardiac output (CO)** may decrease in cardiogenic shock, the other elevated pressures point away from a primary hypovolemic cause.
Shock states pathophysiology US Medical PG Question 3: A 33-year-old pilot is transported to the emergency department after she was involved in a cargo plane crash during a military training exercise in South Korea. She is conscious but confused. She has no history of serious illness and takes no medications. Physical examination shows numerous lacerations and ecchymoses over the face, trunk, and upper extremities. The lower extremities are cool to the touch. There is continued bleeding despite the application of firm pressure to the sites of injury. The first physiologic response to develop in this patient was most likely which of the following?
- A. Increased respiratory rate
- B. Increased capillary refill time
- C. Decreased systolic blood pressure
- D. Decreased urine output
- E. Increased heart rate (Correct Answer)
Shock states pathophysiology Explanation: ***Increased heart rate***
- **Tachycardia** is often the first physiological response to **hypovolemia** (due to hemorrhage, such as that stemming from multiple lacerations). The heart attempts to compensate for reduced circulating blood volume by increasing its pumping rate.
- This sympathetic nervous system response aims to maintain **cardiac output** and tissue perfusion as **blood pressure** and **venous return** start to fall.
*Increased respiratory rate*
- An increased respiratory rate, or **tachypnea**, typically occurs later as the body attempts to compensate for decreased oxygen delivery and metabolic acidosis that can result from sustained hypoperfusion and shock.
- While significant, it usually follows the initial hemodynamic adjustments of the heart.
*Increased capillary refill time*
- **Increased capillary refill time** indicates impaired peripheral perfusion and is a sign of more significant **hypovolemic shock**, often occurring after initial compensatory mechanisms have been activated.
- This reflects **peripheral vasoconstriction**, a later compensatory mechanism, rather than the very first physiological response.
*Decreased systolic blood pressure*
- **Decreased systolic blood pressure** (hypotension) is a later sign of shock and indicates a failure of the body's compensatory mechanisms to maintain adequate blood volume and perfusion, often reflecting a loss of more than 30-40% of blood volume.
- The body initially tries to maintain blood pressure through increased heart rate and vasoconstriction before it drops.
*Decreased urine output*
- **Decreased urine output** (oliguria) is a renal compensatory mechanism in response to reduced renal perfusion and increased antidiuretic hormone (ADH) release, aiming to conserve fluid.
- This response takes time to manifest and is not typically the very first physiological change after acute blood loss.
Shock states pathophysiology US Medical PG Question 4: A 46-year-old male was found unconscious in the field and brought to the emergency department by EMS. The patient was intubated in transit and given a 2 liter bolus of normal saline. On arrival, the patient's blood pressure is 80/60 mmHg and temperature is 37.5°C. Jugular veins are flat and capillary refill time is 4 seconds.
Vascular parameters are measured and are as follows:
Cardiac index - Low
Pulmonary capillary wedge pressure (PCWP) - Low
Systemic vascular resistance - High
Which of the following is the most likely diagnosis?
- A. Septic shock
- B. Anaphylactic shock
- C. Cardiogenic shock
- D. Hypovolemic shock (Correct Answer)
- E. Neurogenic shock
Shock states pathophysiology Explanation: ***Hypovolemic shock***
- The patient presents with **hypotension**, **flat jugular veins**, **prolonged capillary refill**, and a **low cardiac index** and **low pulmonary capillary wedge pressure (PCWP)**, all indicative of inadequate intravascular volume.
- The **high systemic vascular resistance** is a compensatory mechanism to maintain blood pressure in the setting of decreased circulating volume.
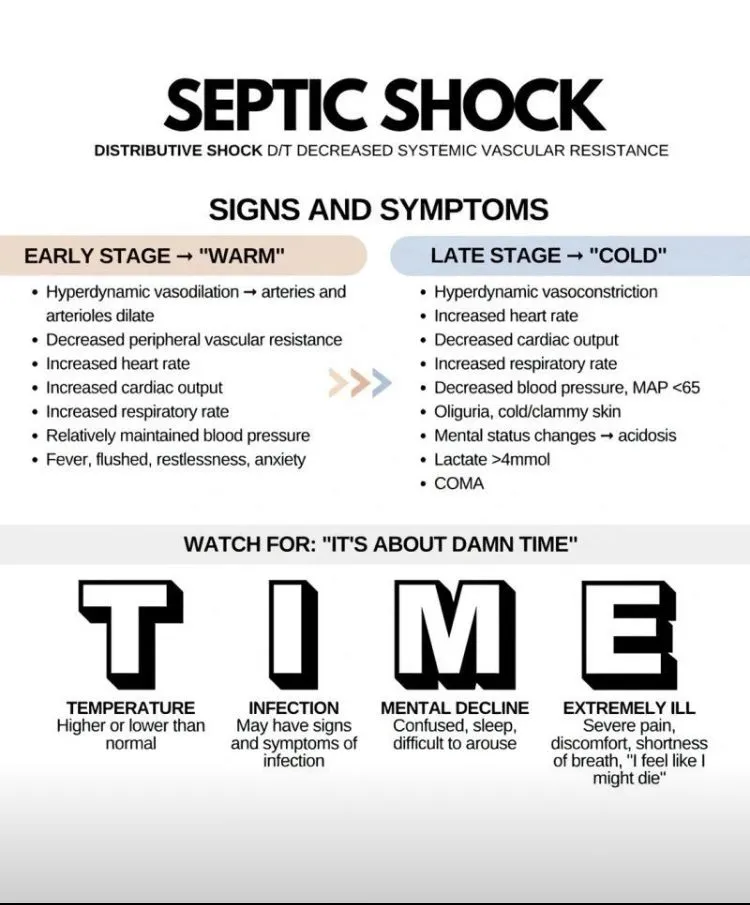
*Septic shock*
- Septic shock typically presents with **vasodilation**, leading to a **low systemic vascular resistance**, which contradicts the findings in this patient.
- While patients can be hypotensive, the vascular parameters, especially SVR, do not align with septic shock.
*Anaphylactic shock*
- This type of shock is characterized by widespread **vasodilation** and increased capillary permeability, leading to a **low systemic vascular resistance** and often significant **edema** or **urticaria**, none of which are suggested here.
- While it can cause hypotension and low PCWP due to fluid shifts, the high SVR makes it less likely.
*Cardiogenic shock*
- Cardiogenic shock is characterized by **pump failure**, leading to a **low cardiac index** but a **high PCWP** due to fluid backup in the pulmonary circulation.
- This directly contrasts the patient's low PCWP.
*Neurogenic shock*
- Neurogenic shock involves a loss of **sympathetic tone**, resulting in widespread **vasodilation** and a **low systemic vascular resistance**, often accompanied by **bradycardia**.
- The high SVR in this patient rules out neurogenic shock.
Shock states pathophysiology US Medical PG Question 5: An otherwise healthy 57-year-old man presents to the emergency department because of progressive shortness of breath and exercise intolerance for the past 5 days. He denies recent travel or illicit habits. His temperature is 36.7°C (98.1°F), the blood pressure is 88/57 mm Hg, and the pulse is 102/min. The radial pulse weakens with inspiration. Physical examination reveals bilateral 1+ pedal edema. There is jugular venous distention at 13 cm and muffled heart sounds. Transthoracic echocardiogram shows reciprocal respiratory ventricular inflow and ventricular diastolic collapse. Which of the following is the best next step in the management of this patient condition?
- A. Pericardiectomy
- B. Pericardial drainage (Correct Answer)
- C. Cardiac catheterization
- D. Cardiac MRI
- E. Chest X-ray
Shock states pathophysiology Explanation: ***Pericardial drainage***
- The clinical presentation, including progressive **shortness of breath**, **hypotension**, **tachycardia**, **pulsus paradoxus** (weak radial pulse with inspiration), **jugular venous distention**, **muffled heart sounds**, and **bilateral pedal edema**, strongly suggests **cardiac tamponade** due to a pericardial effusion.
- Prompt **pericardial drainage** (pericardiocentesis) is a life-saving intervention for cardiac tamponade, as it relieves the pressure on the heart and restores cardiac output.
*Pericardiectomy*
- This is a surgical procedure to remove part or all of the pericardium, typically performed in cases of **constrictive pericarditis** or recurrent effusions that fail conservative management.
- It is a more invasive procedure and not the immediate life-saving intervention required for acute cardiac tamponade.
*Cardiac catheterization*
- This procedure involves inserting a catheter into a blood vessel to measure pressures within the heart chambers and great vessels, often used for diagnosing **coronary artery disease** or valvular heart disease.
- While it can provide hemodynamic data, it is not the most immediate or direct therapeutic intervention for cardiac tamponade.
*Cardiac MRI*
- **Cardiac MRI** provides detailed anatomical imaging of the heart and pericardium, useful for characterizing pericardial effusions or detecting myocardial abnormalities.
- Although it could confirm the diagnosis, it takes time and is not the emergent therapeutic step needed for an unstable patient with cardiac tamponade.
*Chest X-ray*
- A **chest X-ray** might show an enlarged cardiac silhouette (water bottle sign) in cases of large pericardial effusions.
- However, it is not sufficiently sensitive or specific for diagnosing cardiac tamponade and does not provide detailed information about ventricular collapse or hemodynamic compromise.
Shock states pathophysiology US Medical PG Question 6: A 68-year-old woman is brought to the emergency department by ambulance after she was found down by her daughter. She lives alone in her apartment so it is unclear when she began to develop symptoms. Her medical history is significant for cardiac arrhythmias, diabetes, pericarditis, and a stroke 2 years ago. On presentation her temperature is 98.1°F (36.7°C), blood pressure is 88/51 mmHg, pulse is 137/min, and respirations are 18/min. On physical exam her skin is cold and clammy. If special tests were obtained, they would reveal dramatically decreased pulmonary capillary wedge pressure, increased systemic vascular resistance, and mildly decreased cardiac output. Which of the following treatments would most directly target the cause of this patient's low blood pressure?
- A. Vasopressors
- B. Intravenous fluids (Correct Answer)
- C. Antibiotic administration
- D. Relieve obstruction
- E. Intravenous inotropes
Shock states pathophysiology Explanation: ***Intravenous fluids***
- The patient exhibits signs of **hypovolemic shock**, including **hypotension** (BP 88/51 mmHg), **tachycardia** (pulse 137/min), and **cold, clammy skin**. The dramatically decreased **pulmonary capillary wedge pressure (PCWP)** indicates low preload, which is characteristic of hypovolemia.
- Administration of intravenous fluids directly addresses the underlying cause of this patient's low blood pressure by increasing intravascular volume, thereby improving **cardiac preload** and ultimately **cardiac output** and blood pressure.
*Vasopressors*
- While vasopressors can temporarily increase blood pressure by causing **vasoconstriction**, they do not address the root cause of hypovolemic shock, which is insufficient circulating blood volume.
- Using vasopressors without adequate fluid resuscitation in hypovolemic shock can lead to further **organ hypoperfusion** due to increased afterload on an already compromised heart.
*Antibiotic administration*
- Although the patient's presentation with hypotension and tachycardia could raise suspicion for **sepsis**, there is no explicit evidence of infection presented (e.g., fever, focal source).
- The **decreased PCWP** points more strongly towards hypovolemic shock rather than septic shock, where PCWP can be variable or even normal/elevated.
*Relieve obstruction*
- Obstruction, such as in **cardiac tamponade** or **pulmonary embolism**, can cause obstructive shock, which presents with hypotension.
- However, the dramatically **decreased PCWP** is not typically seen in obstructive shock, where PCWP would likely be normal or elevated due to impedance to cardiac filling or outflow.
*Intravenous inotropes*
- **Inotropes** like dobutamine increase myocardial contractility and are primarily indicated in **cardiogenic shock** or severe heart failure with reduced ejection fraction to improve cardiac output.
- While cardiac output is mildly decreased, the primary issue is reduced preload as indicated by the very low PCWP, making fluid resuscitation a more appropriate initial step than directly increasing contractility.
Shock states pathophysiology US Medical PG Question 7: A 27-year-old man is brought to the emergency department by emergency medical services. The patient was an unrestrained passenger in a head-on collision that occurred 15 minutes ago and is currently unresponsive. His temperature is 99.5°F (37.5°C), blood pressure is 60/33 mmHg, pulse is 180/min, respirations are 17/min, and oxygen saturation is 95% on room air. A FAST exam demonstrates fluid in Morrison’s pouch. Laboratory values are drawn upon presentation to the ED and sent off. The patient is started on IV fluids and an initial trauma survey is started. Twenty minutes later, his blood pressure is 95/65 mmHg, and his pulse is 110/min. The patient is further stabilized and is scheduled for emergency surgery. Which of the following best represents this patient’s most likely initial laboratory values?
- A. Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3
- B. Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3
- C. Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3
- D. Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3 (Correct Answer)
- E. Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3
Shock states pathophysiology Explanation: ***Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3***
- The patient experienced significant trauma and is experiencing **hemorrhagic shock**, as evidenced by his initial **hypotension** (BP 60/33 mmHg), **tachycardia** (pulse 180/min), and positive **FAST exam** for fluid in Morrison's pouch, indicating intra-abdominal bleeding.
- The initial hemoglobin and hematocrit could be mildly decreased due to acute blood loss, but significant drops are often *not immediately apparent* as plasma volume has not yet moved into the intravascular compartment to dilute the remaining red blood cells. A hemoglobin of 11 g/dL and hematocrit of 33% are consistent with **acute blood loss** before significant hemodilution occurs. MCV of 88 µm^3 is within the normal range for **normocytic anemia** seen in acute hemorrhage.
*Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3*
- While a hemoglobin of 10 g/dL and hematocrit of 30% are consistent with anemia due to blood loss, an **MCV of 110 µm^3** (macrocytic) is not typically seen in acute hemorrhage.
- Macrocytic anemia usually results from conditions like **B12 or folate deficiency**, alcoholism, or liver disease, which are not suggested by the acute traumatic scenario.
*Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3*
- This indicates **polycythemia** (abnormally high red blood cell count), which is the opposite of what would be expected in a patient experiencing acute hemorrhagic shock.
- These values would suggest conditions like **polycythemia vera** or severe dehydration, which are not relevant in this acute trauma setting.
*Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3*
- While a hemoglobin of 7 g/dL and hematocrit of 21% represent significant anemia consistent with major blood loss, these values are typically seen *later* as **hemodilution** occurs, or in cases of chronic blood loss.
- An **MCV of 75 µm^3** (microcytic) is generally indicative of **iron deficiency anemia** or thalassemia, which develops over time and is not characteristic of acute traumatic blood loss.
*Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3*
- These values are within the **normal range** for hemoglobin and hematocrit, which would not be expected in a patient presenting with signs of **hemorrhagic shock** and a positive FAST exam indicating significant internal bleeding.
- This would suggest either very minor blood loss or that the values were taken before any bleeding had occurred or before hemodilution had a chance to manifest.
Shock states pathophysiology US Medical PG Question 8: A 69-year-old woman is admitted to the hospital with substernal, crushing chest pain. She is emergently moved to the cardiac catheterization lab where she undergoes cardiac angiography. Angiography reveals that the diameter of her left anterior descending artery (LAD) is 50% of normal. If her blood pressure, LAD length, and blood viscosity have not changed, which of the following represents the most likely change in LAD flow from baseline?
- A. Decreased by 93.75% (Correct Answer)
- B. Increased by 6.25%
- C. Decreased by 25%
- D. Decreased by 87.5%
- E. Increased by 25%
Shock states pathophysiology Explanation: ***Decreased by 93.75%***
- This option is correct based on Poiseuille's Law, which states that flow is proportional to the **fourth power of the radius (r^4)**. A 50% decrease in diameter means a 50% decrease in radius (0.5r).
- The new flow would be (0.5)^4 = 0.0625 times the original flow. Therefore, the decrease in flow is 1 - 0.0625 = 0.9375, or **93.75%**.
*Increased by 6.25%*
- This answer incorrectly suggests an **increase** in flow, which is contrary to the effect of a narrowed artery.
- While 6.25% represents the new flow as a percentage of baseline (since 0.0625 = 6.25%), the vessel stenosis causes a **decrease**, not an increase in flow.
*Decreased by 25%*
- This calculation might arise from considering a linear relationship (e.g., radius decreases by 50%, so flow decreases by 50% of 50%, which is incorrect).
- It does not account for the **fourth power relationship** between radius and flow according to Poiseuille's Law.
*Decreased by 87.5%*
- This percentage represents a calculation error, likely from misapplying the fourth power relationship or confusing the calculation steps.
- It does not accurately reflect the dramatic reduction in flow caused by a 50% reduction in vessel diameter.
*Increased by 25%*
- This option implies a significant increase in blood flow, which would not happen with a **stenosed artery**.
- It completely contradicts the physiological response to a **narrowed vessel**.
Shock states pathophysiology US Medical PG Question 9: A 34-year-old male is brought to the emergency department by fire and rescue following a motor vehicle accident in which the patient was an unrestrained driver. The paramedics report that the patient was struck from behind by a drunk driver. He was mentating well at the scene but complained of pain in his abdomen. The patient has no known past medical history. In the trauma bay, his temperature is 98.9°F (37.2°C), blood pressure is 86/51 mmHg, pulse is 138/min, and respirations are 18/min. The patient is somnolent but arousable to voice and pain. His lungs are clear to auscultation bilaterally. He is diffusely tender to palpation on abdominal exam with bruising over the left upper abdomen. His distal pulses are thready, and capillary refill is delayed bilaterally. Two large-bore peripheral intravenous lines are placed to bolus him with intravenous 0.9% saline. Chest radiograph shows multiple left lower rib fractures.
Which of the following parameters is most likely to be seen in this patient?
- A. Increased cardiac output
- B. Increased mixed venous oxygen saturation
- C. Decreased pulmonary capillary wedge pressure (Correct Answer)
- D. Decreased systemic vascular resistance
- E. Increased right atrial pressure
Shock states pathophysiology Explanation: ***Decreased pulmonary capillary wedge pressure***
- The patient presents with classic signs of **hemorrhagic shock** (hypotension, tachycardia, somnolence, abdominal bruising, thready pulses) due to trauma, likely involving the spleen or kidney given the left upper abdominal bruising and rib fractures.
- **Decreased pulmonary capillary wedge pressure (PCWP)** is expected in hypovolemic shock because it reflects left atrial and left ventricular end-diastolic pressure, which will be low due to reduced venous return and intravascular volume.
*Increased cardiac output*
- In **hemorrhagic shock**, the body attempts to compensate by increasing heart rate, but overall **cardiac output is typically decreased** due to profound reduction in preload (venous return) from blood loss.
- While heart rate is elevated, the stroke volume is severely diminished, leading to a net decrease in cardiac output despite compensatory efforts.
*Increased mixed venous oxygen saturation*
- **Mixed venous oxygen saturation (SvO2)** is generally **decreased in hemorrhagic shock** due to increased oxygen extraction by tissues.
- Inadequate oxygen delivery to the tissues forces them to extract more oxygen from the blood, leading to a lower SvO2.
*Decreased systemic vascular resistance*
- In **hemorrhagic shock**, the body activates compensatory mechanisms, including generalized **vasoconstriction**, to maintain blood pressure and prioritize blood flow to vital organs.
- This leads to an **increased systemic vascular resistance (SVR)**, not decreased, as reflected by the thready distal pulses and delayed capillary refill.
*Increased right atrial pressure*
- **Right atrial pressure (RAP)**, representing CVP, is typically **decreased in hemorrhagic shock** due to reduced circulating blood volume.
- A lower RAP indicates decreased venous return to the heart, a hallmark of hypovolemia.
Shock states pathophysiology US Medical PG Question 10: A 52-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He was an unrestrained passenger who was ejected from the vehicle. On presentation, he is found to be actively bleeding from numerous wounds. His blood pressure is 76/42 mmHg and pulse is 152/min. Attempts at resuscitation fail, and he dies 25 minutes later. Autopsy shows blood in the peritoneal cavity, and histology of the kidney reveals swelling of the proximal convoluted tubule epithelial cells. Which of the following is most likely the mechanism underlying the renal cell findings?
- A. Decreased activity of caspase 7
- B. Increased activity of caspase 9
- C. Increased function of the Na+/K+-ATPase
- D. Increased activity of caspase 8
- E. Decreased function of the Na+/K+-ATPase (Correct Answer)
Shock states pathophysiology Explanation: ***Decreased function of the Na+/K+-ATPase***
- The patient experienced **hypovolemic shock** due to severe blood loss, leading to a significant drop in blood pressure and organ perfusion. This results in **ischemia** of the renal cells.
- **Ischemic injury** impairs ATP production, which is essential for the function of the **Na+/K+-ATPase pump**. Failure of this pump leads to intracellular accumulation of sodium and water, causing **cellular swelling**, particularly noticeable in the proximal convoluted tubules.
*Decreased activity of caspase 7*
- **Caspases**, including caspase 7, are involved in **apoptosis** (programmed cell death), which involves cell shrinkage and fragmentation, not the swelling observed here.
- Decreased caspase activity would generally *reduce* apoptosis, which is not the primary mechanism of acute cell injury in shock.
*Increased activity of caspase 9*
- Increased activity of **caspase 9** is indicative of the **intrinsic apoptotic pathway**, typically initiated by mitochondrial damage.
- While prolonged ischemia can eventually lead to apoptotic changes, the acute finding of **cellular swelling** points more directly to immediate membrane pump dysfunction due to ATP depletion.
*Increased function of the Na+/K+-ATPase*
- **Increased function** of the Na+/K+-ATPase would actively pump sodium out of the cell and potassium in, *preventing* intracellular swelling.
- This option contradicts the observed finding of proximal convoluted tubule epithelial cell swelling, which is characteristic of acute cellular injury due to pump failure.
*Increased activity of caspase 8*
- **Caspase 8** is a key initiator caspase in the **extrinsic apoptotic pathway**, often triggered by death receptor signaling.
- Similar to caspase 9, increased caspase 8 activity would lead to apoptosis, characterized by cell shrinkage, not the **cellular swelling** seen in acute ischemic injury.
More Shock states pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.