Pulmonary circulation hemodynamics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pulmonary circulation hemodynamics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pulmonary circulation hemodynamics US Medical PG Question 1: A 43-year-old woman presents to her primary care provider with shortness of breath. She reports a 4-month history of progressively worsening difficulty breathing with associated occasional chest pain. She is a long-distance runner but has had trouble running recently due to her breathing difficulties. Her past medical history is notable for well-controlled hypertension for which she takes hydrochlorothiazide. She had a tibial osteosarcoma lesion with pulmonary metastases as a child and successfully underwent chemotherapy and surgical resection. She has a 10 pack-year smoking history but quit 15 years ago. She drinks a glass of wine 3 times per week. Her temperature is 98.6°F (37°C), blood pressure is 140/85 mmHg, pulse is 82/min, and respirations are 18/min. On exam, she has increased work of breathing with a normal S1 and loud P2. An echocardiogram in this patient would most likely reveal which of the following?
- A. Biventricular dilatation with a decreased ejection fraction
- B. Left ventricular dilatation with an incompetent aortic valve
- C. Left atrial dilatation with mitral valve stenosis
- D. Right ventricular hypertrophy with a dilated pulmonary artery (Correct Answer)
- E. Left ventricular hypertrophy with a bicuspid aortic valve
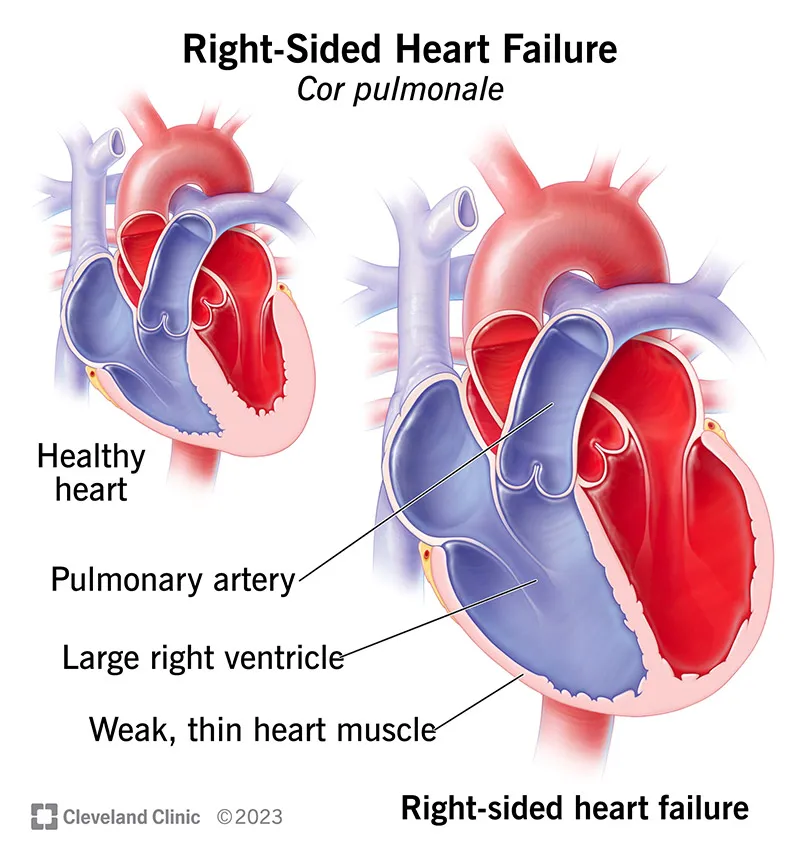
Pulmonary circulation hemodynamics Explanation: The patient's history of **pulmonary metastases** (even successfully treated) and a **loud P2 heart sound** suggest **pulmonary hypertension**, which leads to increased afterload on the right ventricle. [1] **Pulmonary hypertension** causes the **right ventricle to hypertrophy** to overcome the elevated pulmonary arterial pressure, and the **pulmonary artery itself often dilates** due to the sustained high pressure. [1] [2] This describes **dilated cardiomyopathy**, which typically presents with **symptoms of heart failure** but doesn't specifically explain the **loud P2**, which points to pulmonary hypertension. [2]
Pulmonary circulation hemodynamics US Medical PG Question 2: A 62-year-old woman with no significant past medical history presents with progressive dyspnea on exertion over the past 6 months. Echocardiogram reveals elevated pulmonary artery pressure (PAP) of 55 mmHg with normal left ventricular ejection fraction and no evidence of left-sided valvular disease. Right heart catheterization confirms mean PAP of 50 mmHg with pulmonary capillary wedge pressure of 10 mmHg. Intraoperative administration of intravenous adenosine causes the PAP to decrease to 35 mmHg. What pharmacological therapy is most likely to provide long-term benefit for this patient?
- A. Amlodipine (Correct Answer)
- B. Bosentan
- C. Epoprostenol
- D. Sildenafil
- E. Adenosine
Pulmonary circulation hemodynamics Explanation: ***Amlodipine***
- The patient has **idiopathic pulmonary arterial hypertension (PAH, Group 1 PH)** confirmed by elevated mean PAP >20 mmHg with normal pulmonary capillary wedge pressure (≤15 mmHg), excluding left heart disease.
- The **positive acute vasodilator response** (PAP drop >10 mmHg to <40 mmHg) during right heart catheterization indicates **vasoreactivity**, which predicts favorable response to **calcium channel blockers (CCBs)**.
- **Amlodipine** or other CCBs (nifedipine, diltiazem) are the **first-line long-term therapy** for vasoreactive idiopathic PAH, with some patients achieving near-normalization of PAP.
- Only about **10% of idiopathic PAH patients** are vasoreactive, making this finding clinically significant.
*Bosentan*
- **Bosentan** is an **endothelin receptor antagonist** used for **PAH (Group 1)**.
- While effective for PAH, it is typically reserved for patients who are **non-vasoreactive** or who fail CCB therapy.
- Given this patient's positive vasodilator response, a **CCB trial is preferred first** due to better long-term outcomes in vasoreactive patients.
*Epoprostenol*
- **Epoprostenol** is a **prostacyclin analog** used for severe **PAH**, particularly WHO functional class III-IV.
- It requires **continuous intravenous infusion** and is reserved for more advanced or refractory PAH.
- Not appropriate as **first-line therapy** in a vasoreactive patient who can be treated with oral CCBs.
*Sildenafil*
- **Sildenafil** is a **phosphodiesterase-5 inhibitor** effective for **PAH**.
- Like bosentan, it is used for patients who are **non-vasoreactive** or have failed CCB therapy.
- In a vasoreactive patient, **CCBs are preferred** due to superior long-term outcomes in this subset.
*Adenosine*
- **Adenosine** is an **ultrashort-acting vasodilator** used as a **diagnostic agent** during right heart catheterization to assess vasoreactivity.
- It has a half-life of seconds and is **not suitable for long-term therapy**.
- Alternative agents for vasoreactivity testing include inhaled nitric oxide and intravenous epoprostenol.
Pulmonary circulation hemodynamics US Medical PG Question 3: Which of the following physiologic changes decreases pulmonary vascular resistance (PVR)?
- A. Inhaling the inspiratory reserve volume (IRV)
- B. Exhaling the entire vital capacity (VC)
- C. Exhaling the expiratory reserve volume (ERV)
- D. Breath holding maneuver at functional residual capacity (FRC)
- E. Inhaling the entire vital capacity (VC) (Correct Answer)
Pulmonary circulation hemodynamics Explanation: ***Inhaling the entire vital capacity (VC)***
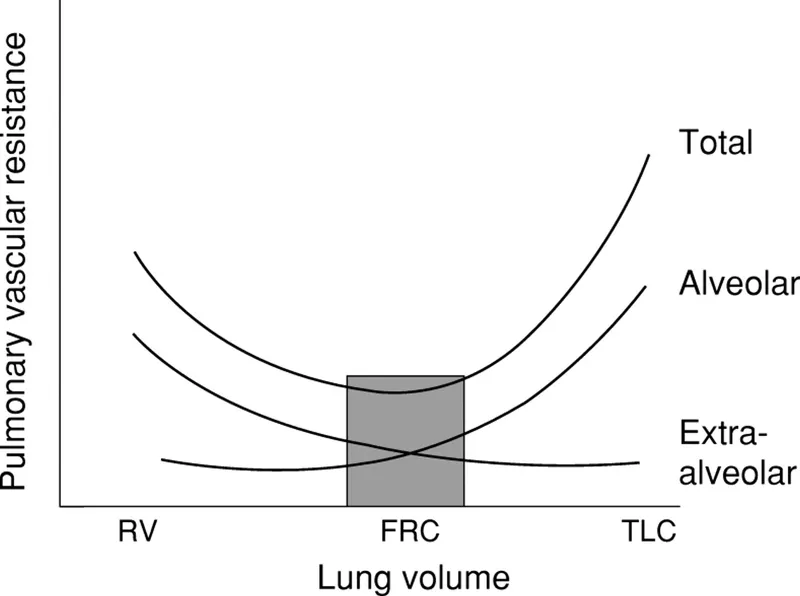
- As lung volume increases from FRC to TLC (which includes inhaling the entire VC), alveolar vessels are **stretched open**, and extra-alveolar vessels are **pulled open** by the increased radial traction, leading to a decrease in PVR.
- This **maximizes the cross-sectional area** of the pulmonary vascular bed, lowering resistance.
*Inhaling the inspiratory reserve volume (IRV)*
- While inhaling IRV increases lung volume, it's not the maximal inspiration of the entire VC where **PVR is typically at its lowest**.
- PVR continues to decrease as lung volume approaches total lung capacity (TLC).
*Exhaling the entire vital capacity (VC)*
- Exhaling the entire vital capacity leads to very low lung volumes, where PVR significantly **increases**.
- At low lung volumes, **alveolar vessels become compressed** and extra-alveolar vessels **narrow**, increasing resistance.
*Exhaling the expiratory reserve volume (ERV)*
- Exhaling the ERV results in a lung volume below FRC, which causes a **marked increase in PVR**.
- This is due to the **compression of alveolar vessels** and decreased radial traction on extra-alveolar vessels.
*Breath holding maneuver at functional residual capacity (FRC)*
- At FRC, the PVR is at an **intermediate level**, not its lowest.
- This is the point where the opposing forces affecting alveolar and extra-alveolar vessels are somewhat balanced, but not optimized for minimal resistance.
Pulmonary circulation hemodynamics US Medical PG Question 4: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Pulmonary circulation hemodynamics Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
Pulmonary circulation hemodynamics US Medical PG Question 5: Which mechanism is primarily responsible for the increase in pulmonary diffusing capacity during exercise?
- A. Decreased airway resistance
- B. Reduced membrane thickness
- C. Increased alveolar ventilation
- D. Pulmonary capillary recruitment (Correct Answer)
Pulmonary circulation hemodynamics Explanation: ***Pulmonary capillary recruitment***
- During exercise, more **pulmonary capillaries** that were previously unperfused or poorly perfused open up, increasing the **surface area available for gas exchange**.
- This **recruitment** directly enhances the pulmonary diffusing capacity by providing more sites for oxygen to cross from the alveoli into the blood.
*Decreased airway resistance*
- While airway resistance can decrease during exercise due to **bronchodilation**, this primarily affects **airflow** and ventilation, not the efficiency of gas diffusion across the alveolar-capillary membrane.
- Reduced airway resistance facilitates getting air into and out of the lungs but does not expand the surface area for diffusion or thin the membrane.
*Reduced membrane thickness*
- The thickness of the **alveolar-capillary membrane** is a structural characteristic that does not significantly change acutely during exercise.
- While a thinner membrane would improve diffusion, this is not the primary mechanism behind the exercise-induced increase in diffusing capacity.
*Increased alveolar ventilation*
- Increased alveolar ventilation ensures a higher **partial pressure of oxygen** in the alveoli.
- While essential for delivering oxygen, it primarily affects the **driving pressure for diffusion** rather than the physical capacity of the diffusion barrier itself.
Pulmonary circulation hemodynamics US Medical PG Question 6: A 37-year-old male presents to your clinic with shortness of breath and lower extremity edema. He was born in Southeast Asia and emigrated to America ten years prior. Examination demonstrates 2+ pitting edema to the level of his knees, ascites, and bibasilar crackles, as well as an opening snap followed by a mid-to-late diastolic murmur. The patient undergoes a right heart catheterization that demonstrates a pulmonary capillary wedge pressure (PCWP) of 24 mmHg. The patient is most likely to have which of the following?
- A. Normal or decreased left ventricular end diastolic pressure (LVEDP) (Correct Answer)
- B. Decreased transmitral gradient
- C. Decreased pulmonary artery systolic pressure (PASP)
- D. Increased left ventricular end diastolic pressure (LVEDP)
- E. Increased pulmonary vascular compliance
Pulmonary circulation hemodynamics Explanation: ***Normal or decreased left ventricular end diastolic pressure (LVEDP)***
- The patient's symptoms (opening snap, mid-to-late diastolic murmur, Southeast Asian origin) strongly suggest **mitral stenosis**.
- In mitral stenosis, the obstruction at the **mitral valve** leads to elevated left atrial pressure (reflected by the high PCWP), but the left ventricle itself is not failing, so LVEDP is typically normal or even decreased.
*Decreased transmitral gradient*
- A **mid-to-late diastolic murmur** and an **opening snap** are classic signs of mitral stenosis, indicating a high pressure gradient across the mitral valve during diastole.
- A decreased transmitral gradient would imply reduced obstruction, which contradicts the patient's strong clinical presentation.
*Decreased pulmonary artery systolic pressure (PASP)*
- Elevated pulmonary capillary wedge pressure (PCWP) of 24 mmHg indicates **pulmonary hypertension secondary to left atrial pressure elevation** in mitral stenosis.
- This consistently leads to an **increased pulmonary artery systolic pressure (PASP)**, not a decreased one, as the right ventricle has to work harder to pump blood through the high-pressure pulmonary vasculature.
*Increased left ventricular end diastolic pressure (LVEDP)*
- While PCWP is elevated due to **left atrial pressure overload** in mitral stenosis, the left ventricle itself is not volume or pressure overloaded during diastole.
- The LVEDP would only be increased if there was actual left ventricular dysfunction or aortic valve disease, which is not suggested here.
*Increased pulmonary vascular compliance*
- Chronic pulmonary hypertension, as seen in advanced mitral stenosis with high PCWP, leads to **pulmonary vascular remodeling** and **decreased pulmonary vascular compliance**.
- The pulmonary vessels become stiffer and less distensible, not more compliant.
Pulmonary circulation hemodynamics US Medical PG Question 7: A 35-year-old woman volunteers for a study on respiratory physiology. Pressure probes A and B are placed as follows:
Probe A: between the parietal and visceral pleura
Probe B: within the cavity of an alveolus
The probes provide a pressure reading relative to atmospheric pressure. To obtain a baseline reading, she is asked to sit comfortably and breathe normally. Which of the following sets of values will most likely be seen at the end of inspiration?
- A. Probe A: -6 mm Hg; Probe B: 0 mm Hg (Correct Answer)
- B. Probe A: 0 mm Hg; Probe B: -1 mm Hg
- C. Probe A: -4 mm Hg; Probe B: 0 mm Hg
- D. Probe A: -4 mm Hg; Probe B: -1 mm Hg
- E. Probe A: -6 mm Hg; Probe B: -1 mm Hg
Pulmonary circulation hemodynamics Explanation: ***Probe A: -6 mm Hg; Probe B: 0 mm Hg***
- At the **end of inspiration**, the **intrapleural pressure (Probe A)** is at its most negative, typically around -6 to -8 cm H2O (equivalent to -4 to -6 mmHg), reflecting the maximum expansion of the thoracic cavity.
- At the **end of inspiration**, just before exhalation begins, there is **no airflow**, so the **intrapulmonary pressure (Probe B)** equalizes with atmospheric pressure, resulting in a 0 mm Hg reading.
*Probe A: 0 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of 0 mm Hg** would indicate a **pneumothorax** since it should always be negative to prevent lung collapse.
- An **intrapulmonary pressure of -1 mm Hg** would indicate that **inspiration is still ongoing**, as air would be flowing into the lungs.
*Probe A: -4 mm Hg; Probe B: 0 mm Hg*
- While an **intrapulmonary pressure of 0 mm Hg** is correct at the end of inspiration, an **intrapleural pressure of -4 mm Hg** is typical for the **end of expiration (Functional Residual Capacity)** during quiet breathing, not the end of inspiration.
- The **intrapleural pressure becomes more negative** during inspiration due to increased thoracic volume, so -4 mm Hg would be insufficient.
*Probe A: -4 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of -4 mm Hg** is the normal pressure at the **end of expiration**, not the end of inspiration, where it becomes more negative.
- An **intrapulmonary pressure of -1 mm Hg** indicates that **inspiration is still in progress**, not at its end, as air would still be flowing into the lungs.
*Probe A: -6 mm Hg; Probe B: -1 mm Hg*
- While an **intrapleural pressure of -6 mm Hg** is consistent with the end of inspiration, an **intrapulmonary pressure of -1 mm Hg** means that **airflow is still occurring into the lungs**.
- At the **very end of inspiration**, just before the start of exhalation, airflow momentarily ceases, and intrapulmonary pressure becomes zero relative to the atmosphere.
Pulmonary circulation hemodynamics US Medical PG Question 8: A 33-year-old woman comes to the physician because of a 6-month history of worsening shortness of breath and fatigue. Her paternal uncle had similar symptoms and died of respiratory failure at 45 years of age. The lungs are clear to auscultation. Pulmonary function testing shows an FVC of 84%, an FEV1/FVC ratio of 92%, and a normal diffusion capacity. An ECG shows a QRS axis greater than +90 degrees. Genetic analysis shows an inactivating mutation in the bone morphogenetic protein receptor type II (BMPR2) gene. Which of the following is the most likely cause of this patient's symptoms?
- A. Thickening of the interventricular septum
- B. Fibrosis of the pulmonary parenchyma
- C. Chronic intravascular hemolysis
- D. Elevated left atrial pressure
- E. Elevated pulmonary arterial pressure (Correct Answer)
Pulmonary circulation hemodynamics Explanation: ***Elevated pulmonary arterial pressure***
- The patient's symptoms (dyspnea, fatigue), family history of early respiratory failure, and the presence of an inactivating mutation in **BMPR2** are highly suggestive of **heritable pulmonary arterial hypertension (PAH)**.
- **PAH** is characterized by elevated pressures in the pulmonary arteries, leading to right ventricular strain, which is reflected by the **ECG finding of a QRS axis greater than +90 degrees** (right axis deviation).
- The **normal diffusion capacity** helps distinguish PAH from parenchymal lung diseases, and the **FEV1/FVC ratio of 92%** (elevated) with relatively preserved FVC is consistent with the restrictive physiology sometimes seen in PAH.
*Thickening of the interventricular septum*
- While septal thickening can occur in some cardiac conditions, it is not the primary cause of symptoms in the context of heritable PAH, nor is it directly indicated by the given pulmonary function tests or ECG.
- **Hypertrophic cardiomyopathy** can cause septal thickening, but it typically presents with different cardiac pathologies and is not associated with BMPR2 mutations.
*Fibrosis of the pulmonary parenchyma*
- This would cause a **restrictive lung disease** with a **reduced FVC** and **reduced diffusion capacity** due to impaired gas exchange across thickened alveolar-capillary membranes.
- The patient's **normal diffusion capacity** specifically rules out significant pulmonary fibrosis or other interstitial lung diseases.
*Chronic intravascular hemolysis*
- This condition would typically present with **anemia**, **jaundice**, **elevated LDH**, and possibly **splenomegaly**, none of which are mentioned.
- It is not associated with the BMPR2 genetic mutation or the specific PFT and ECG findings in this case.
*Elevated left atrial pressure*
- Elevated left atrial pressure (e.g., due to **left-sided heart failure** or mitral stenosis) can cause pulmonary congestion and dyspnea, but would typically lead to **pulmonary edema** with crackles on auscultation and **reduced diffusion capacity** due to fluid in the alveoli.
- The patient's clear lung auscultation and normal diffusion capacity make elevated left atrial pressure unlikely.
Pulmonary circulation hemodynamics US Medical PG Question 9: A 22-year-old man volunteers for a research study on lung function. He has no history of lung disease or allergies and does not smoke. His pulmonary blood flow is measured in the various labeled segments of the lungs while standing. Then the volunteer, still standing, is given very low continuous positive airway pressure and the blood flow measured again. Which of the following sets of findings are most likely to be present in the second measurements relative to the first?
- A. Increased blood flow in zone 2
- B. Reduced blood flow in zone 3
- C. Reduced blood flow in zone 1
- D. Increased blood flow in zone 3
- E. Increased blood flow in zone 1 (Correct Answer)
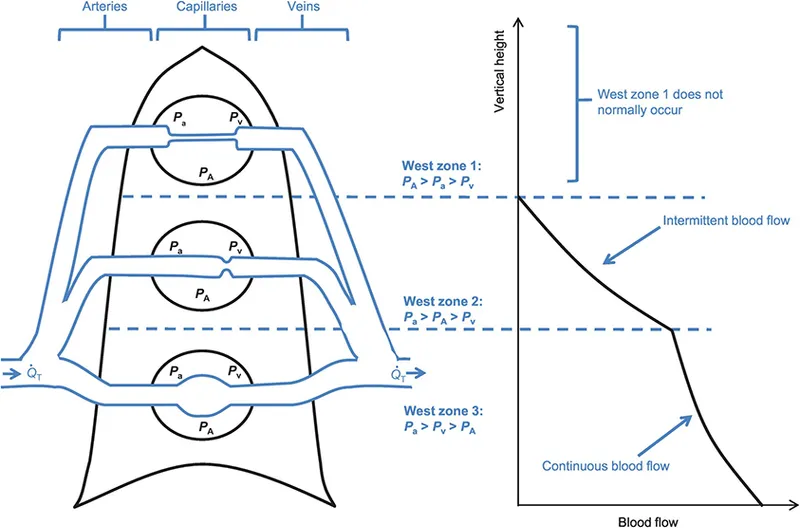
Pulmonary circulation hemodynamics Explanation: ***Increased blood flow in zone 1***
- In healthy standing subjects, **Zone 1** may not exist or is minimal at the apex where alveolar pressure (PA) can exceed arterial pressure (Pa).
- **Very low CPAP** increases alveolar pressure, but when applied at very low levels, it may **recruit collapsed or under-perfused alveoli** by preventing alveolar collapse and improving the pressure gradient.
- The net effect with **very low CPAP** can paradoxically **improve perfusion** in Zone 1 by optimizing alveolar mechanics and reducing vascular resistance through **alveolar recruitment**, particularly in previously under-ventilated apical regions.
*Increased blood flow in zone 2*
- In Zone 2, arterial pressure exceeds alveolar pressure, which exceeds venous pressure (**Pa > PA > Pv**), creating a waterfall effect.
- While CPAP increases alveolar pressure (PA), this would increase the downstream resistance and typically **reduce** the arterial-alveolar pressure gradient (Pa - PA), decreasing flow rather than increasing it.
*Increased blood flow in zone 3*
- **Zone 3** (lung base) normally has the **highest blood flow** where both arterial and venous pressures exceed alveolar pressure (**Pa > Pv > PA**).
- CPAP increases alveolar pressure (PA), which would compress capillaries and **reduce** the pressure gradient, typically decreasing rather than increasing blood flow in this zone.
*Reduced blood flow in zone 1*
- While increasing alveolar pressure with CPAP might be expected to **reduce** Zone 1 perfusion by compressing capillaries, **very low levels of CPAP** can have the opposite effect through **alveolar recruitment** and optimization of lung mechanics.
- The question specifies **very low** CPAP, which is the key—this level improves alveolar patency without significantly compressing capillaries.
*Reduced blood flow in zone 3*
- Zone 3 typically has the highest blood flow due to favorable pressure gradients from gravity.
- CPAP increases PA, which could compress capillaries and reduce the (Pa - PA) gradient, but the **very low level** specified means this effect is minimal and Zone 3 generally maintains adequate perfusion.
Pulmonary circulation hemodynamics US Medical PG Question 10: A 72-year-old obese man presents as a new patient to his primary care physician because he has been feeling tired and short of breath after recently moving to Denver. He is a former 50 pack-year smoker and has previously had deep venous thrombosis. Furthermore, he previously had a lobe of the lung removed due to lung cancer. Finally, he has a family history of a progressive restrictive lung disease. Laboratory values are obtained as follows:
Oxygen tension in inspired air = 130 mmHg
Alveolar carbon dioxide tension = 48 mmHg
Arterial oxygen tension = 58 mmHg
Respiratory exchange ratio = 0.80
Respiratory rate = 20/min
Tidal volume = 500 mL
Which of the following mechanisms is consistent with these values?
- A. Shunt physiology
- B. High altitude
- C. V/Q mismatch
- D. Pulmonary fibrosis
- E. Hypoventilation (Correct Answer)
Pulmonary circulation hemodynamics Explanation: ***Hypoventilation***
- The arterial oxygen tension (PaO2) of 58 mmHg is consistent with hypoxemia, and the alveolar carbon dioxide tension (PACO2) of 48 mmHg (normal 35-45 mmHg) indicates **hypercapnia**, a hallmark of hypoventilation.
- The **alveolar-arterial (A-a) gradient** can be calculated using the alveolar gas equation: PAO2 = PiO2 - PACO2/R. Here, PAO2 = 130 mmHg - 48 mmHg/0.8 = 130 - 60 = 70 mmHg. The A-a gradient is PAO2 - PaO2 = 70 - 58 = 12 mmHg, which is within the normal range (5-15 mmHg), indicating that the hypoxemia is primarily due to **decreased alveolar ventilation**.
*Shunt physiology*
- A shunt would cause a significant reduction in PaO2 and a **widened A-a gradient** (typically >15 mmHg) due to deoxygenated blood bypassing ventilated areas.
- While shunts do not typically cause hypercapnia unless very severe, the normal A-a gradient here rules out a significant shunt as the primary mechanism for hypoxemia.
*High altitude*
- Moving to a high altitude (like Denver) causes a decrease in **inspired oxygen tension (PiO2)**, leading to hypoxemia.
- However, the provided inspired oxygen tension (130 mmHg) is above what would be expected for significant high-altitude hypoxemia at sea level equivalent, and the hypoxemia here is associated with hypercapnia, which is not a direct result of high altitude itself.
*V/Q mismatch*
- A V/Q mismatch leads to hypoxemia and a **widened A-a gradient**, as some areas of the lung are either underventilated or underperfused.
- While it can cause hypoxemia, a V/Q mismatch is typically associated with **normal or low PaCO2** due to compensatory hyperventilation, not hypercapnia, and the A-a gradient would be elevated.
*Pulmonary fibrosis*
- Pulmonary fibrosis is a restrictive lung disease that leads to impaired gas exchange, causing hypoxemia primarily due to **V/Q mismatch** and **diffusion limitation**.
- This would result in a **widened A-a gradient** and often a **low PaCO2** due to compensatory hyperventilation, rather than the elevated PaCO2 observed in this patient.
More Pulmonary circulation hemodynamics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.