Pressure gradients across circulation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pressure gradients across circulation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pressure gradients across circulation US Medical PG Question 1: An investigator is studying brachial artery reactivity in women with suspected coronary heart disease. The brachial artery diameter is measured via ultrasound before and after intra-arterial injection of acetylcholine. An increase of 7% in the vascular diameter is noted. The release of which of the following is most likely responsible for the observed effect?
- A. Norepinephrine from the adrenal medulla
- B. Endothelin from the peripheral vasculature
- C. Serotonin from neuroendocrine cells
- D. Atrial natriuretic peptide from atrial myocytes
- E. Nitric oxide from endothelial cells (Correct Answer)
Pressure gradients across circulation Explanation: ***Nitric oxide from endothelial cells***
- **Acetylcholine** stimulates endothelial cells to release **nitric oxide (NO)**, a potent vasodilator, leading to an increase in vascular diameter. This is the basis of **endothelium-dependent vasodilation**.
- The measurement of brachial artery reactivity involves assessing the ability of blood vessels to dilate in response to various stimuli, which is largely mediated by **NO**.
*Norepinephrine from the adrenal medulla*
- **Norepinephrine** is primarily a vasoconstrictor, acting on alpha-adrenergic receptors to cause **smooth muscle contraction** and a decrease in vascular diameter.
- It is released in response to stress and sympathetic nervous system activation, leading to systemic effects rather than localized vasodilation from acetylcholine.
*Endothelin from the peripheral vasculature*
- **Endothelin** is a powerful **vasoconstrictor** produced by endothelial cells, playing a role in maintaining vascular tone and blood pressure.
- Its action would lead to a decrease, not an increase, in vascular diameter, which is contrary to the observed effect in this scenario.
*Serotonin from neuroendocrine cells*
- **Serotonin (5-HT)** can have both vasoconstrictive and vasodilatory effects depending on the receptor type and vascular bed, but it is not the primary mediator of **acetylcholine-induced vasodilation**.
- Neuroendocrine cells release serotonin as a neurotransmitter and hormone, but its role in brachial artery reactivity to acetylcholine is not dominant.
*Atrial natriuretic peptide from atrial myocytes*
- **Atrial natriuretic peptide (ANP)** is a hormone released by atrial myocytes in response to atrial stretch, primarily promoting vasodilation and increased sodium and water excretion to **lower blood pressure**.
- While it causes vasodilation, it is not directly stimulated by acetylcholine in the context of brachial artery reactivity testing.
Pressure gradients across circulation US Medical PG Question 2: A 72-year-old man presents to his primary care physician for a general checkup. The patient works as a farmer and has no concerns about his health. He has a past medical history of hypertension and obesity. His current medications include lisinopril and metoprolol. His temperature is 99.5°F (37.5°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a murmur after S2 over the left sternal border. The patient demonstrates a stable gait and 5/5 strength in his upper and lower extremities. Which of the following is another possible finding in this patient?
- A. Murmur that radiates to the carotids
- B. Wedge pressure lower than expected
- C. Femoral artery murmur (Correct Answer)
- D. Rumbling heard at the cardiac apex
- E. Audible click heard at the cardiac apex
Pressure gradients across circulation Explanation: ***Femoral artery murmur***
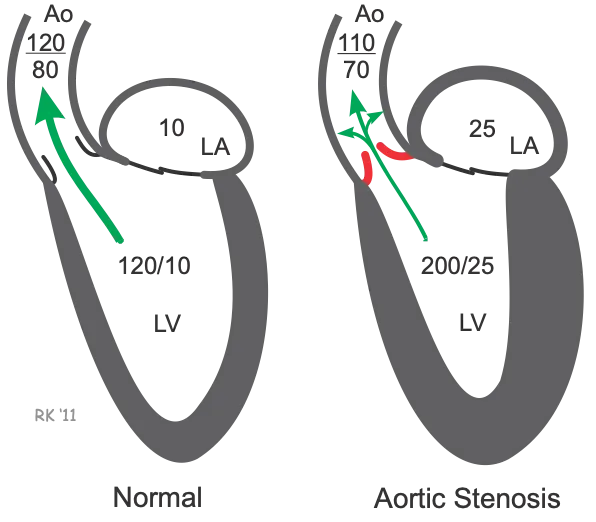
- A murmur heard after S2 over the left sternal border in an elderly patient suggests **aortic regurgitation (AR)**.
- In AR, a **femoral artery murmur (Duroziez's sign)** can be heard, characterized by a systolic murmur over the femoral artery with proximal compression and a diastolic murmur with distal compression.
*Murmur that radiates to the carotids*
- A murmur radiating to the carotids is characteristic of **aortic stenosis**, which typically presents as a systolic murmur, not a diastolic one as heard in this patient.
- Aortic stenosis is also associated with a **crescendo-decrescendo murmur**, in contrast to the diastolic murmur described.
*Wedge pressure lower than expected*
- This patient likely has **aortic regurgitation**, which increases **left ventricular end-diastolic pressure** and, consequently, **pulmonary capillary wedge pressure (PCWP)**.
- A lower than expected wedge pressure would be inconsistent with the volume overload often seen in significant AR.
*Rumbling heard at the cardiac apex*
- A rumbling murmur at the cardiac apex is characteristic of **mitral stenosis**, which is typically preceded by an opening snap.
- The patient's murmur is heard after S2 (diastolic) at the left sternal border, not the apex, making mitral stenosis less likely.
*Audible click heard at the cardiac apex*
- An audible click at the cardiac apex is typically associated with **mitral valve prolapse**, often followed by a mid-systolic murmur.
- This finding is not consistent with the diastolic murmur heard after S2 at the left sternal border.
Pressure gradients across circulation US Medical PG Question 3: A 17-year-old previously healthy, athletic male suddenly falls unconscious while playing soccer. His athletic trainer comes to his aid and notes that he is pulseless. He begins performing CPR on the patient until the ambulance arrives but the teenager is pronounced dead when the paramedics arrived. Upon investigation of his primary care physician's office notes, it was found that the child had a recognized murmur that was ruled to be "benign." Which of the following conditions would have increased the intensity of the murmur?
- A. Inspiration
- B. Placing the patient in a squatting position
- C. Valsalva (Correct Answer)
- D. Passive leg raise
- E. Handgrip
Pressure gradients across circulation Explanation: ***Valsalva***
- The patient's sudden death after collapsing during soccer, coupled with a previously noted "benign" murmur, strongly suggests **hypertrophic obstructive cardiomyopathy (HOCM)**, which is a common cause of sudden cardiac death in young athletes. The **Valsalva maneuver** decreases preload and left ventricular volume, thereby **increasing the left ventricular outflow tract (LVOT) obstruction** and hence the intensity of the HOCM murmur.
- This maneuver reduces venous return to the heart, leading to reduced ventricular filling and decreased stroke volume. This exacerbates the obstruction in HOCM, making the murmur louder.
*Inspiration*
- **Inspiration** typically **increases venous return to the right side of the heart**, which would generally intensify right-sided murmurs (e.g., tricuspid regurgitation).
- It would have **minimal effect or slightly decrease** the intensity of a left-sided obstructive murmur like that in HOCM, as it does not directly increase the LVOT obstruction.
*Placing the patient in a squatting position*
- Squatting increases both **preload** and **afterload** by increasing systemic vascular resistance and venous return.
- This increase in ventricular volume would **reduce the outflow tract obstruction** in HOCM, thereby **decreasing the intensity of the murmur**.
*Passive leg raise*
- A **passive leg raise** increases **venous return** and thus **preload**, leading to increased ventricular filling.
- Similar to squatting, this increased left ventricular volume would **reduce the left ventricular outflow tract obstruction** associated with HOCM, thereby **decreasing the murmur's intensity**.
*Handgrip*
- The **handgrip maneuver** primarily **increases afterload** and, to some extent, preload by increasing systemic vascular resistance.
- While it can increase the intensity of murmurs like mitral regurgitation and ventricular septal defect, it would generally **decrease or have no significant effect** on the murmur of HOCM due to the increased ventricular volume reducing the outflow obstruction.
Pressure gradients across circulation US Medical PG Question 4: An experiment to determine the effects of gravity on blood pressure is conducted on 3 individuals of equal height and blood pressure oriented in different positions in space. Participant A is strapped in a supine position on a bed turned upside down in a vertical orientation with his head towards the floor and his feet towards the ceiling. Participant B is strapped in a supine position on a bed turned downwards in a vertical orientation with his head towards the ceiling and his feet just about touching the floor. Participant C is strapped in a supine position on a bed in a horizontal orientation. Blood pressure readings are then taken at the level of the head, heart, and feet from all 3 participants. Which of these positions will have the lowest recorded blood pressure reading?
- A. Participant B: at the level of the feet
- B. Participant A: at the level of the head
- C. Participant C: at the level of the heart
- D. Participant A: at the level of the feet (Correct Answer)
- E. Participant C: at the level of the feet
Pressure gradients across circulation Explanation: ***Participant A: at the level of the feet***
- In Participant A, the feet are positioned **highest vertically** relative to the heart and are also above the head due to the upside-down vertical orientation. Due to gravity, blood pressure decreases with increasing height above the heart.
- This position would result in the lowest hydrostatic pressure at the feet, leading to the **lowest recorded blood pressure reading**.
*Participant B: at the level of the feet*
- In Participant B, the feet are positioned **below the heart** (towards the floor) in a vertical orientation.
- This position would experience some of the **highest hydrostatic pressure** due to gravity, leading to a high blood pressure reading, not the lowest.
*Participant A: at the level of the head*
- In Participant A, the head is positioned **below the heart** (towards the floor) in an upside-down vertical orientation.
- This position would experience increased hydrostatic pressure, hence a **higher blood pressure** compared to the feet.
*Participant C: at the level of the heart*
- Participant C is in a horizontal position, meaning all body parts are at roughly the same hydrostatic level relative to the heart.
- Blood pressure readings would be **similar across all points** (head, heart, feet) and would reflect the systemic arterial pressure without significant hydrostatic effects, thus not the lowest compared to other extreme positions.
*Participant C: at the level of the feet*
- In Participant C (horizontal), the feet are at approximately the **same hydrostatic level** as the heart.
- The reading at the feet in this position would be close to the **baseline arterial pressure**, not the lowest, as there's minimal hydrostatic gradient.
Pressure gradients across circulation US Medical PG Question 5: An 83-year-old male presents with dyspnea, orthopnea, and a chest radiograph demonstrating pulmonary edema. A diagnosis of congestive heart failure is considered. The following clinical measurements are obtained: 100 bpm heart rate, 0.2 mL O2/mL systemic blood arterial oxygen content, 0.1 mL O2/mL pulmonary arterial oxygen content, and 400 mL O2/min oxygen consumption. Using the above information, which of the following values represents this patient's cardiac stroke volume?
- A. 30 mL/beat
- B. 70 mL/beat
- C. 40 mL/beat (Correct Answer)
- D. 60 mL/beat
- E. 50 mL/beat
Pressure gradients across circulation Explanation: ***40 mL/beat***
- First, calculate cardiac output (CO) using the **Fick principle**: CO = Oxygen Consumption / (Arterial O2 content - Venous O2 content). Here, CO = 400 mL O2/min / (0.2 mL O2/mL - 0.1 mL O2/mL) = 400 mL O2/min / 0.1 mL O2/mL = **4000 mL/min**.
- Next, calculate stroke volume (SV) using the formula: SV = CO / Heart Rate. Given a heart rate of 100 bpm, SV = 4000 mL/min / 100 beats/min = **40 mL/beat**.
*30 mL/beat*
- This answer would result if there was an error in calculating either the **cardiac output** or if the **arteriovenous oxygen difference** was overestimated.
- A stroke volume of 30 mL/beat with a heart rate of 100 bpm would yield a cardiac output of 3 L/min, which is sub-physiologic for an oxygen consumption of 400 mL/min given the provided oxygen content values.
*70 mL/beat*
- This stroke volume is higher than calculated and would imply either a significantly **lower heart rate** or a much **higher cardiac output** than derived from the Fick principle with the given values.
- A stroke volume of 70 mL/beat at a heart rate of 100 bpm would mean a cardiac output of 7 L/min, which is inconsistent with the provided oxygen consumption and arteriovenous oxygen difference.
*60 mL/beat*
- This value is higher than the correct calculation, suggesting an error in the initial calculation of **cardiac output** or the **avO2 difference**.
- To get 60 mL/beat, the cardiac output would need to be 6000 mL/min, which would mean an avO2 difference of 0.067 mL O2/mL, not 0.1 mL O2/mL.
*50 mL/beat*
- This stroke volume would result from an incorrect calculation of the **cardiac output**, potentially from a slight miscalculation of the **arteriovenous oxygen difference**.
- A stroke volume of 50 mL/beat at 100 bpm would mean a cardiac output of 5 L/min, requiring an avO2 difference of 0.08 mL O2/mL, which is not consistent with the given values.
Pressure gradients across circulation US Medical PG Question 6: A 37-year-old male presents to your clinic with shortness of breath and lower extremity edema. He was born in Southeast Asia and emigrated to America ten years prior. Examination demonstrates 2+ pitting edema to the level of his knees, ascites, and bibasilar crackles, as well as an opening snap followed by a mid-to-late diastolic murmur. The patient undergoes a right heart catheterization that demonstrates a pulmonary capillary wedge pressure (PCWP) of 24 mmHg. The patient is most likely to have which of the following?
- A. Normal or decreased left ventricular end diastolic pressure (LVEDP) (Correct Answer)
- B. Decreased transmitral gradient
- C. Decreased pulmonary artery systolic pressure (PASP)
- D. Increased left ventricular end diastolic pressure (LVEDP)
- E. Increased pulmonary vascular compliance
Pressure gradients across circulation Explanation: ***Normal or decreased left ventricular end diastolic pressure (LVEDP)***
- The patient's symptoms (opening snap, mid-to-late diastolic murmur, Southeast Asian origin) strongly suggest **mitral stenosis**.
- In mitral stenosis, the obstruction at the **mitral valve** leads to elevated left atrial pressure (reflected by the high PCWP), but the left ventricle itself is not failing, so LVEDP is typically normal or even decreased.
*Decreased transmitral gradient*
- A **mid-to-late diastolic murmur** and an **opening snap** are classic signs of mitral stenosis, indicating a high pressure gradient across the mitral valve during diastole.
- A decreased transmitral gradient would imply reduced obstruction, which contradicts the patient's strong clinical presentation.
*Decreased pulmonary artery systolic pressure (PASP)*
- Elevated pulmonary capillary wedge pressure (PCWP) of 24 mmHg indicates **pulmonary hypertension secondary to left atrial pressure elevation** in mitral stenosis.
- This consistently leads to an **increased pulmonary artery systolic pressure (PASP)**, not a decreased one, as the right ventricle has to work harder to pump blood through the high-pressure pulmonary vasculature.
*Increased left ventricular end diastolic pressure (LVEDP)*
- While PCWP is elevated due to **left atrial pressure overload** in mitral stenosis, the left ventricle itself is not volume or pressure overloaded during diastole.
- The LVEDP would only be increased if there was actual left ventricular dysfunction or aortic valve disease, which is not suggested here.
*Increased pulmonary vascular compliance*
- Chronic pulmonary hypertension, as seen in advanced mitral stenosis with high PCWP, leads to **pulmonary vascular remodeling** and **decreased pulmonary vascular compliance**.
- The pulmonary vessels become stiffer and less distensible, not more compliant.
Pressure gradients across circulation US Medical PG Question 7: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Pressure gradients across circulation Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
*Myogenic response*
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
Pressure gradients across circulation US Medical PG Question 8: A 19-year-old man presents to the clinic with a complaint of increasing shortness of breath for the past 2 years. His shortness of breath is associated with mild chest pain and occasional syncopal attacks during strenuous activity. There is no history of significant illness in the past, however, one of his uncles had similar symptoms when he was his age and died while playing basketball a few years later. He denies alcohol use, tobacco consumption, and the use of recreational drugs. On examination, pulse rate is 76/min and is regular and bounding; blood pressure is 130/70 mm Hg. A triple apical impulse is observed on the precordium and a systolic ejection crescendo-decrescendo murmur is audible between the apex and the left sternal border along with a prominent fourth heart sound. The physician then asks the patient to take a deep breath, close his mouth, and pinch his nose and try to breathe out without allowing his cheeks to bulge out. In doing so, the intensity of the murmur increases. Which of the following hemodynamic changes would be observed first during this maneuver?
- A. ↓ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↓ Parasympathetic Outflow
- B. ↑ Mean Arterial Pressure, ↓ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow (Correct Answer)
- C. ↑ Mean Arterial Pressure, ↓ Heart rate, ↓ Baroreceptor activity, ↑ Parasympathetic Outflow
- D. ↑ Mean Arterial Pressure, ↑ Heart rate, ↓ Baroreceptor activity, ↓ Parasympathetic Outflow
- E. ↑ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow
Pressure gradients across circulation Explanation: **↑ Mean Arterial Pressure, ↓ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow**
- This maneuver is the **Valsalva Maneuver**, which involves forced expiration against a closed glottis. It causes a transient increase in **intrathoracic pressure**, compressing the great vessels and temporarily increasing **mean arterial pressure**.
- The initial rise in blood pressure is detected by **baroreceptors**, leading to a reflex decrease in **heart rate** via increased **parasympathetic outflow**.
*↓ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↓ Parasympathetic Outflow*
- This option describes changes more typical of the **later phases** of a Valsalva maneuver (Phase 2), where venous return and cardiac output decrease, leading to a fall in MAP and a compensatory increase in heart rate.
- It does not represent the **immediate hemodynamic changes** (Phase 1) that occur during the initial strain of the maneuver.
*↑ Mean Arterial Pressure, ↓ Heart rate, ↓ Baroreceptor activity, ↑ Parasympathetic Outflow*
- A decrease in **baroreceptor activity** would typically lead to an *increase* in heart rate and a *decrease* in parasympathetic outflow, contrary to the initial response to increased blood pressure.
- The initial increase in MAP correctly leads to *increased* baroreceptor activity.
*↑ Mean Arterial Pressure, ↑ Heart rate, ↓ Baroreceptor activity, ↓ Parasympathetic Outflow*
- An increase in **mean arterial pressure** (MAP) would reflexively cause a *decrease* in heart rate and an *increase* in parasympathetic outflow, mediated by *increased* baroreceptor activity, not decreased activity.
- Therefore, the proposed changes in heart rate, baroreceptor activity, and parasympathetic outflow are inconsistent with an initial increase in MAP.
*↑ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow*
- While an increase in **mean arterial pressure** does lead to an increase in **baroreceptor activity** and **parasympathetic outflow**, the reflexive response to this increased pressure is a *decrease* in **heart rate**, not an increase.
- An increased heart rate combined with increased parasympathetic outflow is contradictory, as sympathetic and parasympathetic systems typically exert opposing effects on heart rate.
Pressure gradients across circulation US Medical PG Question 9: A 66-year-old man is brought to the emergency department 20 minutes after being involved in a high-speed motor vehicle collision in which he was the unrestrained passenger. His wife confirms that he has hypertension, atrial fibrillation, and chronic lower back pain. Current medications include metoprolol, warfarin, hydrochlorothiazide, and oxycodone. On arrival, he is lethargic and confused. His pulse is 112/min, respirations are 10/min, and blood pressure is 172/78 mm Hg. The eyes open spontaneously. The pupils are equal and sluggish. He moves his extremities in response to commands. There is a 3-cm scalp laceration. There are multiple bruises over the right upper extremity. Cardiopulmonary examination shows no abnormalities. The abdomen is soft and nontender. Neurologic examination shows no focal findings. Two large-bore peripheral intravenous catheters are inserted. A 0.9% saline infusion is begun. A focused assessment with sonography in trauma is negative. Plain CT of the brain shows a 5-mm right subdural hematoma with no mass effect. Fresh frozen plasma is administered. Which of the following is most likely to reduce this patient's cerebral blood flow?
- A. Hyperventilation (Correct Answer)
- B. Lumbar puncture
- C. Decompressive craniectomy
- D. Intravenous hypertonic saline
- E. Intravenous mannitol
Pressure gradients across circulation Explanation: ***Hyperventilation***
- **Hyperventilation** reduces arterial partial pressure of carbon dioxide (**PaCO2**), causing **cerebral vasoconstriction** and thereby decreasing cerebral blood flow (CBF).
- This effect is used therapeutically to transiently lower **intracranial pressure (ICP)** in cases of acute cerebral edema or herniation by reducing cerebral blood volume.
*Lumbar puncture*
- A **lumbar puncture** drains cerebrospinal fluid (CSF) from the subarachnoid space, which would reduce ICP.
- However, it does not directly impact cerebral blood flow regulations, and in some situations with elevated ICP, it can be hazardous due to the risk of **herniation**.
*Decompressive craniectomy*
- **Decompressive craniectomy** involves removing a portion of the skull to allow the brain to swell, directly reducing ICP by increasing intracranial volume.
- While it lowers ICP, it doesn't directly reduce cerebral blood flow; in fact, by relieving compression, it may help maintain or improve CBF.
*Intravenous hypertonic saline*
- **Intravenous hypertonic saline** increases serum osmolarity, drawing fluid out of brain cells and into the intravascular space, thereby reducing **cerebral edema** and ICP.
- This reduction in edema and ICP can improve rather than reduce cerebral blood flow by reducing extrinsic compression of cerebral vessels.
*Intravenous mannitol*
- **Intravenous mannitol** is an osmotic diuretic that creates an osmotic gradient, drawing fluid from the brain parenchyma into the intravascular compartment, reducing **cerebral edema** and ICP.
- Similar to hypertonic saline, its primary effect is to decrease brain volume and ICP, which tends to improve CBF by reducing vascular compression, not reduce it.
Pressure gradients across circulation US Medical PG Question 10: A 37-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He suffered multiple deep lacerations and experienced significant blood loss during transport. In the emergency department, his temperature is 98.6°F (37°C), blood pressure is 102/68 mmHg, pulse is 112/min, and respirations are 22/min. His lacerations are sutured and he is given 2 liters of saline by large bore intravenous lines. Which of the following changes will occur in this patient's cardiac physiology due to this intervention?
- A. Increased cardiac output and unchanged right atrial pressure
- B. Decreased cardiac output and increased right atrial pressure
- C. Increased cardiac output and decreased right atrial pressure
- D. Increased cardiac output and increased right atrial pressure (Correct Answer)
- E. Decreased cardiac output and decreased right atrial pressure
Pressure gradients across circulation Explanation: ***Increased cardiac output and increased right atrial pressure***
- The patient experienced significant blood loss, leading to a **decreased preload** and subsequent **reduced cardiac output**. Volume resuscitation with saline directly increases the **intravascular volume** which bolsters **venous return** and **right atrial pressure**.
- According to the **Frank-Starling mechanism**, increased right atrial pressure (a measure of preload) results in an increase in ventricular stretch and a more forceful contraction, thereby increasing **stroke volume** and **cardiac output**.
*Increased cardiac output and unchanged right atrial pressure*
- While fluid administration will increase **cardiac output** by improving preload, it will also directly lead to an increase in **right atrial pressure** due to the augmented venous return.
- An unchanged right atrial pressure would imply no significant increase in central venous volume, which contradicts the effect of a large volume fluid resuscitation.
*Decreased cardiac output and increased right atrial pressure*
- This scenario is unlikely because increasing **intravascular volume** through fluid resuscitation typically aims to raise **cardiac output** by optimizing preload, not decrease it.
- A decrease in cardiac output despite increased right atrial pressure could indicate **cardiac pump failure**, which is not suggested by the clinical picture of hypovolemic shock treated with fluids.
*Increased cardiac output and decreased right atrial pressure*
- An increase in **cardiac output** as a result of fluid resuscitation is expected, but a **decreased right atrial pressure** would contradict the mechanism of increased venous return and volume expansion.
- Decreased right atrial pressure would typically indicate ongoing volume loss or inadequate fluid resuscitation to restore central venous volume.
*Decreased cardiac output and decreased right atrial pressure*
- Both decreasing **cardiac output** and decreasing **right atrial pressure** indicate a worsening state of **hypovolemia** or an inadequate response to fluid resuscitation.
- The administration of 2 liters of saline is intended to correct the hypovolemia and improve cardiodynamics, not to worsen them.
More Pressure gradients across circulation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.