Orthostatic changes in hemodynamics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Orthostatic changes in hemodynamics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Orthostatic changes in hemodynamics US Medical PG Question 1: A 66-year-old woman presents to the emergency department after a fall 4 hours ago. She was on her way to the bathroom when she fell to the ground and lost consciousness. Although she regained consciousness within one minute, she experienced lightheadedness for almost half an hour. She has experienced on-and-off dizziness for the past 2 weeks whenever she tries to stand. She has a history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, and chronic kidney disease secondary to polycystic kidneys. Her medications include aspirin, bisoprolol, doxazosin, erythropoietin, insulin, rosuvastatin, and calcium and vitamin D supplements. She has a blood pressure of 111/74 mm Hg while supine and 84/60 mm Hg on standing, the heart rate of 48/min, the respiratory rate of 14/min, and the temperature of 37.0°C (98.6°F). CT scan of the head is unremarkable. Electrocardiogram reveals a PR interval of 250 ms. What is the next best step in the management of this patient?
- A. Tilt table testing
- B. Holter monitoring
- C. Stop antihypertensive medicines (Correct Answer)
- D. Electroencephalogram
- E. Start anti-epileptics
Orthostatic changes in hemodynamics Explanation: ***Stop antihypertensive medicines***
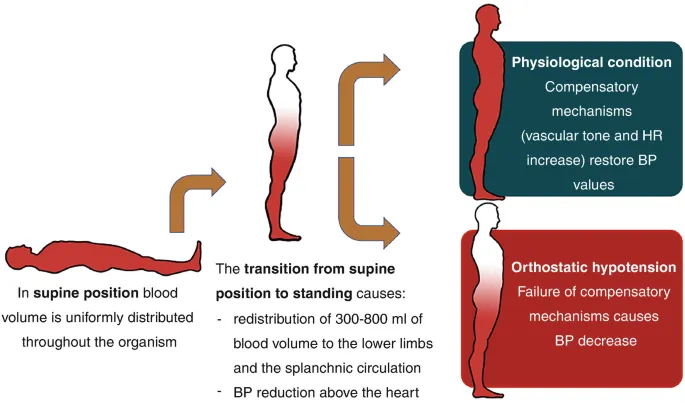
- The patient exhibits significant **orthostatic hypotension** (systolic drop of 27 mm Hg and diastolic drop of 14 mm Hg, along with lightheadedness lasting 30 minutes) [1] and **bradycardia** (48/min), suggesting that her antihypertensive medications, particularly **doxazosin** (an alpha-blocker causing vasodilation) and **bisoprolol** (a beta-blocker causing bradycardia), are contributing to her symptoms [4].
- Given her fall, lightheadedness, and profound orthostatic changes, immediately reducing or discontinuing the medications causing hypotension and bradycardia is the priority to stabilize her blood pressure and heart rate, preventing further syncopal episodes or falls [1], [4].
*Tilt table testing*
- This test is primarily used to diagnose **vasovagal syncope** or **postural orthostatic tachycardia syndrome (POTS)**, often when routine orthostatic measurements are equivocal or other causes have been ruled out [2].
- In this case, the patient's orthostatic hypotension is clearly documented with current medications, and the immediate concern is medication-induced, making further diagnostic testing for this specific cause less urgent than medication adjustment.
*Holter monitoring*
- **Holter monitoring** is useful for detecting intermittent **cardiac arrhythmias** that may cause syncope.
- While the patient has a prolonged PR interval (250 ms) indicating first-degree AV block, which rarely causes syncope on its own, her primary issue appears to be profound orthostatic hypotension [2] and bradycardia likely exacerbated by medications, rather than an uncaptured paroxysmal arrhythmia.
*Electroencephalogram*
- An **EEG** is indicated to diagnose **seizures** as a cause of loss of consciousness.
- The patient's fall and brief loss of consciousness followed by lightheadedness align with syncope rather than a seizure [3]; her CT scan is unremarkable, and there are no typical seizure features (e.g., tonic-clonic movements, postictal confusion, tongue biting) [3].
*Start anti-epileptics*
- Starting **anti-epileptics** would only be appropriate if there was strong evidence of a seizure disorder, such as clear clinical presentation of seizure or abnormal EEG findings.
- There is no clinical or imaging evidence to support a seizure diagnosis in this patient; her symptoms are more consistent with cardiovascular causes, specifically medication-induced syncope [3].
Orthostatic changes in hemodynamics US Medical PG Question 2: An experiment to determine the effects of gravity on blood pressure is conducted on 3 individuals of equal height and blood pressure oriented in different positions in space. Participant A is strapped in a supine position on a bed turned upside down in a vertical orientation with his head towards the floor and his feet towards the ceiling. Participant B is strapped in a supine position on a bed turned downwards in a vertical orientation with his head towards the ceiling and his feet just about touching the floor. Participant C is strapped in a supine position on a bed in a horizontal orientation. Blood pressure readings are then taken at the level of the head, heart, and feet from all 3 participants. Which of these positions will have the lowest recorded blood pressure reading?
- A. Participant B: at the level of the feet
- B. Participant A: at the level of the head
- C. Participant C: at the level of the heart
- D. Participant A: at the level of the feet (Correct Answer)
- E. Participant C: at the level of the feet
Orthostatic changes in hemodynamics Explanation: ***Participant A: at the level of the feet***
- In Participant A, the feet are positioned **highest vertically** relative to the heart and are also above the head due to the upside-down vertical orientation. Due to gravity, blood pressure decreases with increasing height above the heart.
- This position would result in the lowest hydrostatic pressure at the feet, leading to the **lowest recorded blood pressure reading**.
*Participant B: at the level of the feet*
- In Participant B, the feet are positioned **below the heart** (towards the floor) in a vertical orientation.
- This position would experience some of the **highest hydrostatic pressure** due to gravity, leading to a high blood pressure reading, not the lowest.
*Participant A: at the level of the head*
- In Participant A, the head is positioned **below the heart** (towards the floor) in an upside-down vertical orientation.
- This position would experience increased hydrostatic pressure, hence a **higher blood pressure** compared to the feet.
*Participant C: at the level of the heart*
- Participant C is in a horizontal position, meaning all body parts are at roughly the same hydrostatic level relative to the heart.
- Blood pressure readings would be **similar across all points** (head, heart, feet) and would reflect the systemic arterial pressure without significant hydrostatic effects, thus not the lowest compared to other extreme positions.
*Participant C: at the level of the feet*
- In Participant C (horizontal), the feet are at approximately the **same hydrostatic level** as the heart.
- The reading at the feet in this position would be close to the **baseline arterial pressure**, not the lowest, as there's minimal hydrostatic gradient.
Orthostatic changes in hemodynamics US Medical PG Question 3: A 33-year-old pilot is transported to the emergency department after she was involved in a cargo plane crash during a military training exercise in South Korea. She is conscious but confused. She has no history of serious illness and takes no medications. Physical examination shows numerous lacerations and ecchymoses over the face, trunk, and upper extremities. The lower extremities are cool to the touch. There is continued bleeding despite the application of firm pressure to the sites of injury. The first physiologic response to develop in this patient was most likely which of the following?
- A. Increased respiratory rate
- B. Increased capillary refill time
- C. Decreased systolic blood pressure
- D. Decreased urine output
- E. Increased heart rate (Correct Answer)
Orthostatic changes in hemodynamics Explanation: ***Increased heart rate***
- **Tachycardia** is often the first physiological response to **hypovolemia** (due to hemorrhage, such as that stemming from multiple lacerations). The heart attempts to compensate for reduced circulating blood volume by increasing its pumping rate.
- This sympathetic nervous system response aims to maintain **cardiac output** and tissue perfusion as **blood pressure** and **venous return** start to fall.
*Increased respiratory rate*
- An increased respiratory rate, or **tachypnea**, typically occurs later as the body attempts to compensate for decreased oxygen delivery and metabolic acidosis that can result from sustained hypoperfusion and shock.
- While significant, it usually follows the initial hemodynamic adjustments of the heart.
*Increased capillary refill time*
- **Increased capillary refill time** indicates impaired peripheral perfusion and is a sign of more significant **hypovolemic shock**, often occurring after initial compensatory mechanisms have been activated.
- This reflects **peripheral vasoconstriction**, a later compensatory mechanism, rather than the very first physiological response.
*Decreased systolic blood pressure*
- **Decreased systolic blood pressure** (hypotension) is a later sign of shock and indicates a failure of the body's compensatory mechanisms to maintain adequate blood volume and perfusion, often reflecting a loss of more than 30-40% of blood volume.
- The body initially tries to maintain blood pressure through increased heart rate and vasoconstriction before it drops.
*Decreased urine output*
- **Decreased urine output** (oliguria) is a renal compensatory mechanism in response to reduced renal perfusion and increased antidiuretic hormone (ADH) release, aiming to conserve fluid.
- This response takes time to manifest and is not typically the very first physiological change after acute blood loss.
Orthostatic changes in hemodynamics US Medical PG Question 4: A 27-year-old woman G2P1 at 34 weeks estimated gestational age presents with bouts of sweating, weakness, and dizziness lasting a few minutes after lying down on the bed. She says symptoms resolve if she rolls on her side. She reports that these episodes have occurred several times over the last 3 weeks. On lying down, her blood pressure is 90/50 mm Hg and her pulse is 50/min. When she rolls on her side, her blood pressure slowly increases to 120/65 mm Hg, and her pulse increases to 72/min. Which of the following best describes the mechanism which underlies this patient’s most likely condition?
- A. Peripheral vasodilation
- B. Increase in plasma volume
- C. Progesterone surge
- D. Renin-angiotensin system activation
- E. Aortocaval compression (Correct Answer)
Orthostatic changes in hemodynamics Explanation: ***Aortocaval compression***
- This condition, also known as **supine hypotensive syndrome**, occurs when the gravid uterus **compresses the inferior vena cava (IVC)** and potentially the aorta, reducing **venous return** to the heart.
- The symptoms (sweating, weakness, dizziness, hypotension, bradycardia) and their resolution upon changing position are classic signs of reduced cardiac output due to IVC compression.
*Peripheral vasodilation*
- While **peripheral vasodilation** does occur in pregnancy due to hormonal changes, it generally contributes to a **mild decrease in systemic vascular resistance** and is not the primary mechanism behind acute, position-dependent hypotensive episodes.
- It would not explain the sudden, severe symptoms that resolve promptly with a change in position, nor the associated bradycardia which is more indicative of a **vasovagal response** to decreased cardiac filling.
*Increase in plasma volume*
- Pregnancy is associated with a significant **increase in plasma volume** (up to 50%), which is a physiological adaptation to support the uteroplacental unit.
- An increase in plasma volume would generally help **maintain blood pressure** and prevent hypotension, rather than causing the specific symptoms described in this patient.
*Progesterone surge*
- **Progesterone levels do increase significantly** during pregnancy and contribute to **smooth muscle relaxation**, which can lead to vasodilation.
- However, a progesterone surge itself does not directly cause acute, position-dependent hypotensive episodes; its vasodilatory effects are more chronic and physiological.
*Renin-angiotensin system activation*
- The **renin-angiotensin system (RAS) is typically activated** and upregulated during pregnancy, contributing to fluid balance and blood pressure regulation.
- Activation of the RAS would generally lead to **vasoconstriction and increased blood pressure**, not the hypotensive episodes observed in this patient.
Orthostatic changes in hemodynamics US Medical PG Question 5: A 58-year-old man presents to the emergency department following a fall while walking in a grocery store. He has a history of at least 6 previous collapses to the ground with no warning. When these episodes occur, he becomes pale, diaphoretic, and recovers quickly within a few seconds. These episodes always occur when he is standing. His past medical history is significant for type 2 diabetes mellitus, hypercholesterolemia, and one myocardial infarction. His medication list includes aspirin, clopidogrel, bisoprolol, metformin, rosuvastatin, and valsartan. Further history reveals that he has constipation, early satiety, and recently lost 2.2 kg (5 lb) of weight. While lying down, his blood pressure is 145/64 mm Hg and the heart rate is 112/min. After 2 minutes of standing, the blood pressure is 120/65 mm Hg and the heart rate is 112/min. A 12-lead ECG showed Q waves in leads II, III, and aVF. Laboratory results are given below:
Hemoglobin 13.8 g/dL
White blood cell count 8500/mm3
Platelets 250,000/mm3
Sodium 142 mEq/L
Potassium 4.4 mEq/L
Calcium 9.1 mg/dL
Creatinine 1.0 mg/dL
TSH 1.4 U/mL
HbA1c 10.2%
What additional clinical feature would most likely be present in this patient?
- A. Heat intolerance
- B. Diplopia
- C. Erectile dysfunction (Correct Answer)
- D. Lipodystrophy
- E. Amyotrophy
Orthostatic changes in hemodynamics Explanation: ***Erectile dysfunction***
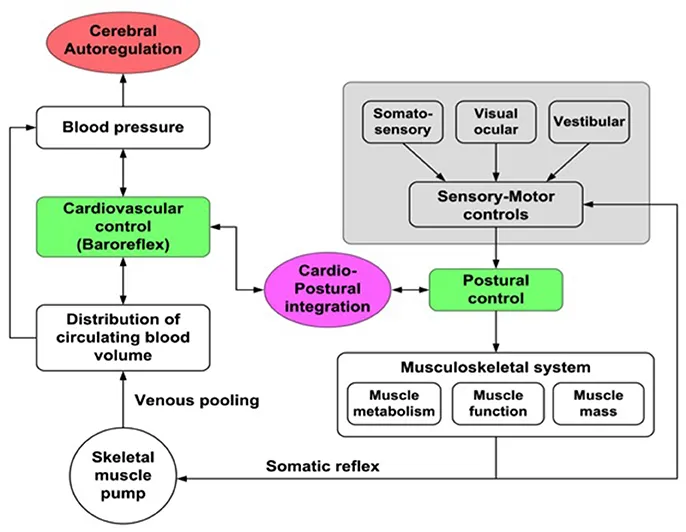
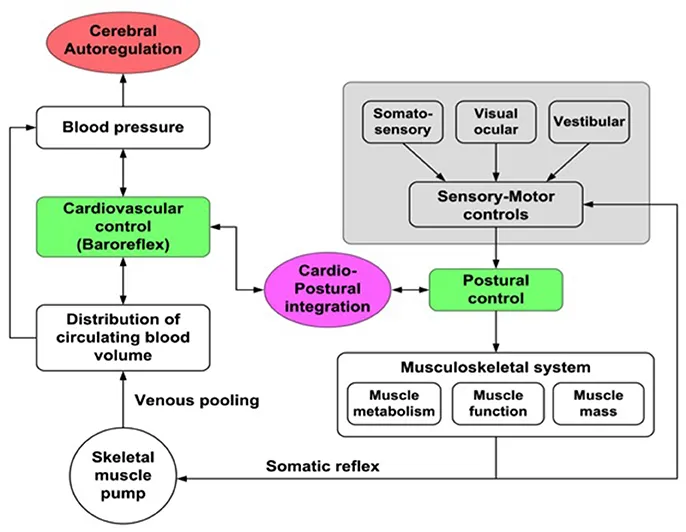
- The patient exhibits features of **diabetic autonomic neuropathy**, including **orthostatic hypotension with absent compensatory tachycardia** (heart rate remains 112/min despite BP drop from 145/64 to 120/65 on standing - this failure of baroreceptor reflex is pathognomonic for autonomic dysfunction), **gastroparesis** (early satiety, weight loss, constipation), and poor glycemic control (HbA1c 10.2%).
- **Erectile dysfunction** is a common manifestation of **diabetic autonomic neuropathy** due to impaired parasympathetic innervation affecting penile blood flow and nerve-mediated vasodilation.
*Heat intolerance*
- This is typically associated with **hyperthyroidism** or sometimes with impaired sweating from **sudomotor autonomic neuropathy**, but it's not the most direct or common manifestation given the other symptoms.
- The patient's TSH is normal (1.4 U/mL), ruling out a thyroid cause.
*Diplopia*
- While possible in diabetes due to **cranial nerve palsies** (e.g., CN III, IV, VI neuropathy), it is not a direct or prominent symptom of *autonomic* neuropathy.
- Diplopia would indicate a *somatic* neuropathy affecting ocular muscles, rather than an autonomic dysfunction.
*Lipodystrophy*
- This condition refers to abnormal fat distribution and is often seen with **insulin therapy** (at injection sites) or certain genetic syndromes, not directly related to diabetic autonomic neuropathy.
- There is no information to suggest the patient is on insulin, and lipodystrophy does not explain the cluster of autonomic symptoms.
*Amyotrophy*
- **Diabetic amyotrophy** (proximal motor neuropathy) primarily causes **muscle weakness** and **wasting**, typically in the quadriceps, and severe pain in the affected areas.
- This is a *somatic* neuropathy, affecting motor nerves, rather than the constellation of autonomic symptoms presented by the patient.
Orthostatic changes in hemodynamics US Medical PG Question 6: A 73-year-old woman comes to the physician because of recurrent episodes of losing consciousness for several seconds upon standing. She has a history of hypertension, which has been treated with hydrochlorothiazide. Her blood pressure is 130/87 mm Hg in the supine position and 100/76 mm Hg 30 seconds after standing up. Cardiac examination shows no abnormalities. Which of the following sets of changes in venous return, cardiac output, and blood pressure (respectively) is most likely to occur when the patient stands up?
- A. ↓ ↑ ↓
- B. No change ↓ ↓
- C. ↑ ↑ ↓
- D. ↓ ↓ ↓ (Correct Answer)
- E. ↑ ↑ ↑
Orthostatic changes in hemodynamics Explanation: ***Correct: ↓ ↓ ↓***
- Upon standing, gravity causes **blood pooling in the lower extremities**, leading to a **decrease in venous return** to the heart.
- Reduced venous return directly results in decreased **cardiac output** (via Frank-Starling mechanism), which then causes the observed **drop in blood pressure**.
- This patient demonstrates orthostatic hypotension, exacerbated by diuretic therapy (hydrochlorothiazide), which reduces intravascular volume and impairs compensatory baroreceptor responses.
*Incorrect: ↓ ↑ ↓*
- While there is a **decrease in venous return** and **blood pressure** upon standing, a paradoxical increase in **cardiac output** is not physiologically plausible in the immediate response to orthostasis causing syncope.
- If cardiac output were to increase significantly, it would likely help to maintain blood pressure, rather than cause a sharp drop and syncope.
*Incorrect: No change ↓ ↓*
- It is inaccurate to state that there is **no change in venous return** upon standing; gravity inevitably causes blood to pool in the lower limbs, reducing venous return.
- A decrease in blood pressure as described, particularly leading to syncope, is primarily a consequence of reduced venous return and subsequent drop in cardiac output.
*Incorrect: ↑ ↑ ↓*
- An increase in both **venous return** and **cardiac output** upon standing is contrary to the gravitational effects on blood distribution.
- If both increased, blood pressure would likely increase or be maintained, not decrease to the point of syncope.
*Incorrect: ↑ ↑ ↑*
- An increase in **venous return**, **cardiac output**, and **blood pressure** upon standing would indicate a robust and effective baroreceptor response, which is the opposite of what is observed in a patient experiencing orthostatic syncope.
- This pattern would be seen in healthy individuals whose compensatory mechanisms prevent a significant drop in blood pressure.
Orthostatic changes in hemodynamics US Medical PG Question 7: A 68-year-old woman is brought to the emergency department by ambulance after she was found down by her daughter. She lives alone in her apartment so it is unclear when she began to develop symptoms. Her medical history is significant for cardiac arrhythmias, diabetes, pericarditis, and a stroke 2 years ago. On presentation her temperature is 98.1°F (36.7°C), blood pressure is 88/51 mmHg, pulse is 137/min, and respirations are 18/min. On physical exam her skin is cold and clammy. If special tests were obtained, they would reveal dramatically decreased pulmonary capillary wedge pressure, increased systemic vascular resistance, and mildly decreased cardiac output. Which of the following treatments would most directly target the cause of this patient's low blood pressure?
- A. Vasopressors
- B. Intravenous fluids (Correct Answer)
- C. Antibiotic administration
- D. Relieve obstruction
- E. Intravenous inotropes
Orthostatic changes in hemodynamics Explanation: ***Intravenous fluids***
- The patient exhibits signs of **hypovolemic shock**, including **hypotension** (BP 88/51 mmHg), **tachycardia** (pulse 137/min), and **cold, clammy skin**. The dramatically decreased **pulmonary capillary wedge pressure (PCWP)** indicates low preload, which is characteristic of hypovolemia.
- Administration of intravenous fluids directly addresses the underlying cause of this patient's low blood pressure by increasing intravascular volume, thereby improving **cardiac preload** and ultimately **cardiac output** and blood pressure.
*Vasopressors*
- While vasopressors can temporarily increase blood pressure by causing **vasoconstriction**, they do not address the root cause of hypovolemic shock, which is insufficient circulating blood volume.
- Using vasopressors without adequate fluid resuscitation in hypovolemic shock can lead to further **organ hypoperfusion** due to increased afterload on an already compromised heart.
*Antibiotic administration*
- Although the patient's presentation with hypotension and tachycardia could raise suspicion for **sepsis**, there is no explicit evidence of infection presented (e.g., fever, focal source).
- The **decreased PCWP** points more strongly towards hypovolemic shock rather than septic shock, where PCWP can be variable or even normal/elevated.
*Relieve obstruction*
- Obstruction, such as in **cardiac tamponade** or **pulmonary embolism**, can cause obstructive shock, which presents with hypotension.
- However, the dramatically **decreased PCWP** is not typically seen in obstructive shock, where PCWP would likely be normal or elevated due to impedance to cardiac filling or outflow.
*Intravenous inotropes*
- **Inotropes** like dobutamine increase myocardial contractility and are primarily indicated in **cardiogenic shock** or severe heart failure with reduced ejection fraction to improve cardiac output.
- While cardiac output is mildly decreased, the primary issue is reduced preload as indicated by the very low PCWP, making fluid resuscitation a more appropriate initial step than directly increasing contractility.
Orthostatic changes in hemodynamics US Medical PG Question 8: A 19-year-old man presents to the clinic with a complaint of increasing shortness of breath for the past 2 years. His shortness of breath is associated with mild chest pain and occasional syncopal attacks during strenuous activity. There is no history of significant illness in the past, however, one of his uncles had similar symptoms when he was his age and died while playing basketball a few years later. He denies alcohol use, tobacco consumption, and the use of recreational drugs. On examination, pulse rate is 76/min and is regular and bounding; blood pressure is 130/70 mm Hg. A triple apical impulse is observed on the precordium and a systolic ejection crescendo-decrescendo murmur is audible between the apex and the left sternal border along with a prominent fourth heart sound. The physician then asks the patient to take a deep breath, close his mouth, and pinch his nose and try to breathe out without allowing his cheeks to bulge out. In doing so, the intensity of the murmur increases. Which of the following hemodynamic changes would be observed first during this maneuver?
- A. ↓ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↓ Parasympathetic Outflow
- B. ↑ Mean Arterial Pressure, ↓ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow (Correct Answer)
- C. ↑ Mean Arterial Pressure, ↓ Heart rate, ↓ Baroreceptor activity, ↑ Parasympathetic Outflow
- D. ↑ Mean Arterial Pressure, ↑ Heart rate, ↓ Baroreceptor activity, ↓ Parasympathetic Outflow
- E. ↑ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow
Orthostatic changes in hemodynamics Explanation: **↑ Mean Arterial Pressure, ↓ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow**
- This maneuver is the **Valsalva Maneuver**, which involves forced expiration against a closed glottis. It causes a transient increase in **intrathoracic pressure**, compressing the great vessels and temporarily increasing **mean arterial pressure**.
- The initial rise in blood pressure is detected by **baroreceptors**, leading to a reflex decrease in **heart rate** via increased **parasympathetic outflow**.
*↓ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↓ Parasympathetic Outflow*
- This option describes changes more typical of the **later phases** of a Valsalva maneuver (Phase 2), where venous return and cardiac output decrease, leading to a fall in MAP and a compensatory increase in heart rate.
- It does not represent the **immediate hemodynamic changes** (Phase 1) that occur during the initial strain of the maneuver.
*↑ Mean Arterial Pressure, ↓ Heart rate, ↓ Baroreceptor activity, ↑ Parasympathetic Outflow*
- A decrease in **baroreceptor activity** would typically lead to an *increase* in heart rate and a *decrease* in parasympathetic outflow, contrary to the initial response to increased blood pressure.
- The initial increase in MAP correctly leads to *increased* baroreceptor activity.
*↑ Mean Arterial Pressure, ↑ Heart rate, ↓ Baroreceptor activity, ↓ Parasympathetic Outflow*
- An increase in **mean arterial pressure** (MAP) would reflexively cause a *decrease* in heart rate and an *increase* in parasympathetic outflow, mediated by *increased* baroreceptor activity, not decreased activity.
- Therefore, the proposed changes in heart rate, baroreceptor activity, and parasympathetic outflow are inconsistent with an initial increase in MAP.
*↑ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow*
- While an increase in **mean arterial pressure** does lead to an increase in **baroreceptor activity** and **parasympathetic outflow**, the reflexive response to this increased pressure is a *decrease* in **heart rate**, not an increase.
- An increased heart rate combined with increased parasympathetic outflow is contradictory, as sympathetic and parasympathetic systems typically exert opposing effects on heart rate.
Orthostatic changes in hemodynamics US Medical PG Question 9: An 83-year-old male presents with dyspnea, orthopnea, and a chest radiograph demonstrating pulmonary edema. A diagnosis of congestive heart failure is considered. The following clinical measurements are obtained: 100 bpm heart rate, 0.2 mL O2/mL systemic blood arterial oxygen content, 0.1 mL O2/mL pulmonary arterial oxygen content, and 400 mL O2/min oxygen consumption. Using the above information, which of the following values represents this patient's cardiac stroke volume?
- A. 30 mL/beat
- B. 70 mL/beat
- C. 40 mL/beat (Correct Answer)
- D. 60 mL/beat
- E. 50 mL/beat
Orthostatic changes in hemodynamics Explanation: ***40 mL/beat***
- First, calculate cardiac output (CO) using the **Fick principle**: CO = Oxygen Consumption / (Arterial O2 content - Venous O2 content). Here, CO = 400 mL O2/min / (0.2 mL O2/mL - 0.1 mL O2/mL) = 400 mL O2/min / 0.1 mL O2/mL = **4000 mL/min**.
- Next, calculate stroke volume (SV) using the formula: SV = CO / Heart Rate. Given a heart rate of 100 bpm, SV = 4000 mL/min / 100 beats/min = **40 mL/beat**.
*30 mL/beat*
- This answer would result if there was an error in calculating either the **cardiac output** or if the **arteriovenous oxygen difference** was overestimated.
- A stroke volume of 30 mL/beat with a heart rate of 100 bpm would yield a cardiac output of 3 L/min, which is sub-physiologic for an oxygen consumption of 400 mL/min given the provided oxygen content values.
*70 mL/beat*
- This stroke volume is higher than calculated and would imply either a significantly **lower heart rate** or a much **higher cardiac output** than derived from the Fick principle with the given values.
- A stroke volume of 70 mL/beat at a heart rate of 100 bpm would mean a cardiac output of 7 L/min, which is inconsistent with the provided oxygen consumption and arteriovenous oxygen difference.
*60 mL/beat*
- This value is higher than the correct calculation, suggesting an error in the initial calculation of **cardiac output** or the **avO2 difference**.
- To get 60 mL/beat, the cardiac output would need to be 6000 mL/min, which would mean an avO2 difference of 0.067 mL O2/mL, not 0.1 mL O2/mL.
*50 mL/beat*
- This stroke volume would result from an incorrect calculation of the **cardiac output**, potentially from a slight miscalculation of the **arteriovenous oxygen difference**.
- A stroke volume of 50 mL/beat at 100 bpm would mean a cardiac output of 5 L/min, requiring an avO2 difference of 0.08 mL O2/mL, which is not consistent with the given values.
Orthostatic changes in hemodynamics US Medical PG Question 10: A 69-year-old woman is admitted to the hospital with substernal, crushing chest pain. She is emergently moved to the cardiac catheterization lab where she undergoes cardiac angiography. Angiography reveals that the diameter of her left anterior descending artery (LAD) is 50% of normal. If her blood pressure, LAD length, and blood viscosity have not changed, which of the following represents the most likely change in LAD flow from baseline?
- A. Decreased by 93.75% (Correct Answer)
- B. Increased by 6.25%
- C. Decreased by 25%
- D. Decreased by 87.5%
- E. Increased by 25%
Orthostatic changes in hemodynamics Explanation: ***Decreased by 93.75%***
- This option is correct based on Poiseuille's Law, which states that flow is proportional to the **fourth power of the radius (r^4)**. A 50% decrease in diameter means a 50% decrease in radius (0.5r).
- The new flow would be (0.5)^4 = 0.0625 times the original flow. Therefore, the decrease in flow is 1 - 0.0625 = 0.9375, or **93.75%**.
*Increased by 6.25%*
- This answer incorrectly suggests an **increase** in flow, which is contrary to the effect of a narrowed artery.
- While 6.25% represents the new flow as a percentage of baseline (since 0.0625 = 6.25%), the vessel stenosis causes a **decrease**, not an increase in flow.
*Decreased by 25%*
- This calculation might arise from considering a linear relationship (e.g., radius decreases by 50%, so flow decreases by 50% of 50%, which is incorrect).
- It does not account for the **fourth power relationship** between radius and flow according to Poiseuille's Law.
*Decreased by 87.5%*
- This percentage represents a calculation error, likely from misapplying the fourth power relationship or confusing the calculation steps.
- It does not accurately reflect the dramatic reduction in flow caused by a 50% reduction in vessel diameter.
*Increased by 25%*
- This option implies a significant increase in blood flow, which would not happen with a **stenosed artery**.
- It completely contradicts the physiological response to a **narrowed vessel**.
More Orthostatic changes in hemodynamics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.