Microcirculation physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Microcirculation physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Microcirculation physiology US Medical PG Question 1: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Microcirculation physiology Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
Microcirculation physiology US Medical PG Question 2: A scientist is studying the excretion of a novel toxin X by the kidney in order to understand the dynamics of this new substance. He discovers that this new toxin X has a clearance that is half that of inulin in a particular patient. This patient's filtration fraction is 20% and his para-aminohippuric acid (PAH) dynamics are as follows:
Urine volume: 100 mL/min
Urine PAH concentration: 30 mg/mL
Plasma PAH concentration: 5 mg/mL
Given these findings, what is the clearance of the novel toxin X?
- A. 1,500 mL/min
- B. 600 mL/min
- C. 300 mL/min
- D. 60 mL/min (Correct Answer)
- E. 120 mL/min
Microcirculation physiology Explanation: ***60 ml/min***
- First, calculate the **renal plasma flow (RPF)** using PAH clearance: RPF = (Urine PAH conc. × Urine vol.) / Plasma PAH conc. = (30 mg/mL × 100 mL/min) / 5 mg/mL = 600 mL/min.
- Next, calculate the **glomerular filtration rate (GFR)**, which is the clearance of inulin. GFR = RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min. Toxin X clearance is half of inulin clearance, so 120 mL/min / 2 = **60 mL/min**.
*1,500 ml/min*
- This value is likely obtained if an incorrect formula or conversion was made, possibly by misinterpreting the units or the relationship between GFR, RPF, and filtration fraction.
- It significantly overestimates the clearance for a substance that is cleared at half the rate of inulin.
*600 ml/min*
- This value represents the **renal plasma flow (RPF)**, calculated using the PAH clearance data.
- It does not account for the filtration fraction or the fact that toxin X clearance is half of inulin clearance (GFR).
*300 ml/min*
- This value would be obtained if the renal plasma flow (RPF) was incorrectly halved, or if an intermediate calculation was misinterpreted as the final answer.
- It does not align with the given filtration fraction and the relationship between toxin X and inulin clearance.
*120 ml/min*
- This value represents the **glomerular filtration rate (GFR)**, which is equal to the clearance of inulin (RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min).
- The question states that the clearance of toxin X is **half** that of inulin, so this is an intermediate step, not the final answer.
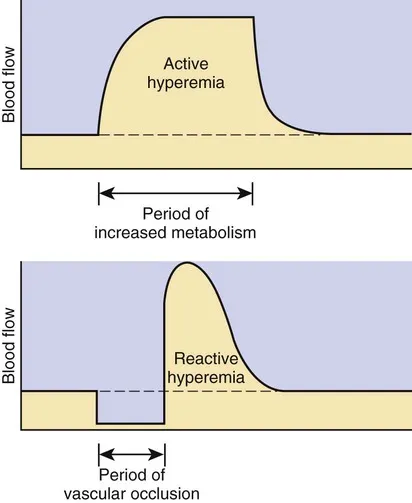
Microcirculation physiology US Medical PG Question 3: During a clinical study evaluating the effects of exercise on muscle perfusion, 15 healthy individuals perform a 20-minute treadmill run at submaximal effort. Before and after the treadmill session, perfusion of the quadriceps muscle is evaluated with contrast-enhanced magnetic resonance imaging. The study shows a significant increase in muscle blood flow per unit of tissue mass. Which of the following local changes is most likely involved in the observed change in perfusion?
- A. Increase in adenosine (Correct Answer)
- B. Decrease in potassium
- C. Increase in thromboxane A2
- D. Increase in endothelin
- E. Decrease in prostacyclin
Microcirculation physiology Explanation: ***Increase in adenosine***
- **Adenosine** is a potent **vasodilator** released by metabolically active tissues, particularly in response to increased oxygen demand and ATP hydrolysis during exercise.
- Its accumulation leads to relaxation of vascular smooth muscle, increasing blood flow to meet the muscles' elevated metabolic needs.
*Decrease in potassium*
- An increase in **extracellular potassium** (not a decrease) generally causes vasodilation in skeletal muscle by hyperpolarizing smooth muscle cells.
- A decrease in potassium outside the cell would not be expected to cause vasodilation and increased perfusion during exercise.
*Increase in thromboxane A2*
- **Thromboxane A2** is primarily a **vasoconstrictor** and platelet aggregator, mainly involved in hemostasis and inflammation.
- Increased levels would lead to reduced blood flow, not the observed increase in perfusion during exercise.
*Increase in endothelin*
- **Endothelin** is one of the most potent **vasoconstrictors** known, primarily released from endothelial cells.
- An increase in endothelin would severely constrict blood vessels and decrease muscle perfusion, counteracting the effects of exercise.
*Decrease in prostacyclin*
- **Prostacyclin (PGI2)** is a potent **vasodilator** and inhibitor of platelet aggregation.
- A decrease in prostacyclin would lead to vasoconstriction and reduced blood flow, which is contrary to the increased perfusion seen during exercise.
Microcirculation physiology US Medical PG Question 4: An 8-year-old boy is shifted to a post-surgical floor following neck surgery. The surgeon has restricted his oral intake for the next 24 hours. He does not have diarrhea, vomiting, or dehydration. His calculated fluid requirement is 1500 mL/day. However, he receives 2000 mL of intravenous isotonic fluids over 24 hours. Which of the following physiological parameters in the boy’s circulatory system is most likely to be increased?
- A. Interstitial oncotic pressure
- B. Interstitial hydrostatic pressure
- C. Capillary wall permeability
- D. Capillary oncotic pressure
- E. Capillary hydrostatic pressure (Correct Answer)
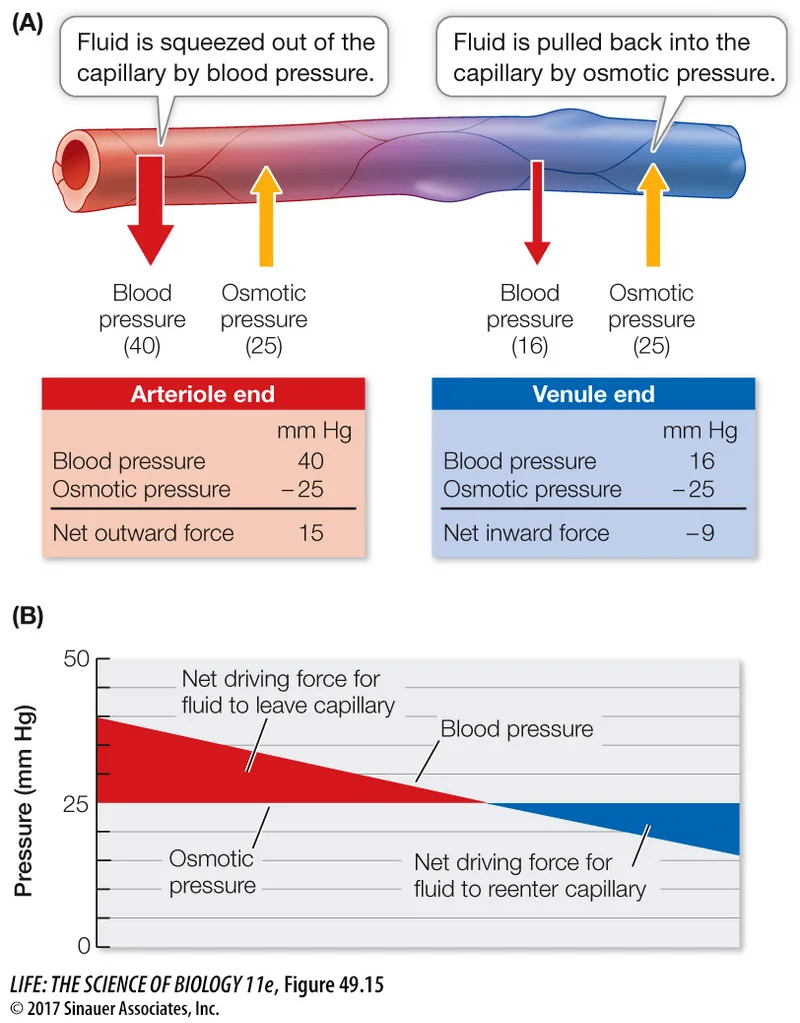
Microcirculation physiology Explanation: ***Capillary hydrostatic pressure***
- Giving 2000 mL of intravenous isotonic fluids when the calculated requirement is 1500 mL/day leads to a **positive fluid balance** and **fluid overload**.
- This excess fluid directly increases the **intravascular volume**, thereby raising the **capillary hydrostatic pressure**, which pushes fluid out of the capillaries.
*Interstitial oncotic pressure*
- This pressure is primarily determined by the **protein concentration** in the interstitial fluid.
- While fluid overload can dilute interstitial proteins, it generally does not directly increase interstitial oncotic pressure; rather, it might decrease it due to fluid movement.
*Interstitial hydrostatic pressure*
- As fluid moves out of the capillaries due to increased capillary hydrostatic pressure, the **interstitial hydrostatic pressure** will also increase.
- However, the primary driving force for this change, and thus the most direct consequence of fluid overload, is the increase in capillary hydrostatic pressure.
*Capillary wall permeability*
- This parameter refers to the ease with which substances, including fluid and proteins, can cross the capillary wall.
- Fluid overload does not typically affect **capillary wall permeability** unless there is an underlying condition causing inflammation or damage to the capillary endothelium.
*Capillary oncotic pressure*
- This pressure is mainly determined by the **protein concentration** within the capillaries.
- In a state of fluid overload with isotonic fluids, the plasma proteins are diluted, leading to a **decrease** in capillary oncotic pressure, not an increase.
Microcirculation physiology US Medical PG Question 5: A 67-year-old woman comes to the physician with a 6-month history of pain and swelling of both legs. The symptoms are worst at the end of the day and are associated with itching of the overlying skin. Physical examination shows bilateral pitting ankle edema. An image of one of the ankles is shown. This patient is at greatest risk for which of the following complications?
- A. Osmotic injury to the peripheral nerves
- B. Thrombosis of a deep vein
- C. Malignant transformation of lymphatic endothelium
- D. Biliverdin accumulation in the epidermis
- E. Ulceration of the cutis (Correct Answer)
Microcirculation physiology Explanation: ***Ulceration of the cutis (skin)***
- This patient has **chronic venous insufficiency** with signs of **venous stasis dermatitis** (bilateral pitting edema, end-of-day worsening, pruritus)
- Chronic venous hypertension leads to skin breakdown and **venous stasis ulcers**, typically at the medial malleolus
- The 6-month duration, itching, and skin changes indicate progression toward ulceration - the **most common serious complication** of chronic venous insufficiency
- Venous ulcers develop in 3-5% of patients with chronic venous disease
*Osmotic injury to the peripheral nerves*
- Not a recognized complication of venous insufficiency
- Osmotic nerve injury occurs in conditions like **diabetes** with glucose-induced osmotic stress, unrelated to the venous pathology presented
*Thrombosis of a deep vein*
- While **venous stasis** is a risk factor for DVT (Virchow's triad), this patient has **chronic bilateral** findings suggesting longstanding venous insufficiency rather than acute thrombosis
- DVT typically presents with **unilateral**, acute-onset pain, warmth, and swelling
- Given the chronic presentation with skin changes, **ulceration is the greatest risk**
*Malignant transformation of lymphatic endothelium*
- Refers to **lymphangiosarcoma (Stewart-Treves syndrome)**, an extremely rare complication of **chronic lymphedema**, not venous insufficiency
- Would present with purple nodules and typically occurs after years of severe lymphatic obstruction
*Biliverdin accumulation in the epidermis*
- **Hemosiderin** (not biliverdin) deposition occurs in chronic venous insufficiency, causing brown hyperpigmentation (hemosiderin staining)
- However, this is a cosmetic finding, not a serious complication like ulceration
- Biliverdin is associated with bruising/hematoma resolution, not chronic venous disease
Microcirculation physiology US Medical PG Question 6: A researcher is studying proteins that contribute to intestinal epithelial permeability. He has isolated intestinal tissue from several mice. After processing the tissue into its individual components, he uses a Western blot analysis to identify a protein that forms part of a multi-protein complex at the apical aspect of epithelial cells. The complex is known to provide a diffusion barrier between the apical and basolateral aspects of epithelial cells. Which of the following proteins is this researcher most likely investigating?
- A. Integrin
- B. Connexon
- C. Desmoglein
- D. E-cadherin
- E. Claudin (Correct Answer)
Microcirculation physiology Explanation: ***Claudin***
- **Claudins** are integral membrane proteins that are primary components of **tight junctions** (zonulae occludentes), which form a diffusion barrier at the **apical aspect** of epithelial cells.
- They regulate **paracellular permeability**, crucial for maintaining the integrity of the intestinal epithelial barrier.
*Integrin*
- **Integrins** are transmembrane receptors that mediate cell-extracellular matrix (ECM) adhesion and cell-cell adhesion, but they are not the primary components of tight junction diffusion barriers.
- They are involved in cell signaling and structural support, rather than forming a direct paracellular seal.
*Connexon*
- A **connexon** is a protein assembly that forms a **gap junction**, allowing direct communication and passage of small molecules between adjacent cells.
- Gap junctions facilitate intercellular communication, but do not primarily contribute to sealing the paracellular space as a diffusion barrier.
*Desmoglein*
- **Desmoglein** is a cadherin family protein found in **desmosomes** (maculae adherens), which are cell-cell adhesion complexes that provide strong mechanical attachments between cells.
- Desmosomes resist shearing forces and provide structural integrity but do not regulate paracellular permeability as tight junctions do.
*E-cadherin*
- **E-cadherin** is a crucial component of **adherens junctions** (zonula adherens), which provide cell-cell adhesion and help establish and maintain cell polarity.
- While important for epithelial integrity, E-cadherin primarily links cells to the actin cytoskeleton and is not directly responsible for forming the selective diffusion barrier itself.
Microcirculation physiology US Medical PG Question 7: A 31-year-old female with a history of anxiety has a panic attack marked by dizziness, weakness, and blurred vision. Which of the following most likely accounts for the patient’s symptoms?
- A. Oxygen toxicity
- B. Increased arterial CO2
- C. Carotid artery obstruction
- D. Decreased cerebral blood flow (Correct Answer)
- E. Decreased respiratory rate
Microcirculation physiology Explanation: ***Decreased cerebral blood flow***
- During a panic attack, **hyperventilation** leads to a drop in arterial CO2, causing **cerebral vasoconstriction** and reduced blood flow to the brain.
- This reduction in cerebral blood flow manifests as neurological symptoms like **dizziness, blurred vision, and weakness**.
*Oxygen toxicity*
- This typically occurs with exposure to **high partial pressures of oxygen**, often in diving or hyperbaric oxygen therapy.
- Symptoms include **seizures, visual changes, and nausea**; it is not associated with panic attacks or their physiological responses.
*Increased arterial CO2*
- Panic attacks involve **hyperventilation**, which causes a decrease, not an increase, in arterial CO2 (hypocapnia).
- Increased arterial CO2 (hypercapnia) usually leads to **vasodilation**, which would increase cerebral blood flow rather than decrease it.
*Carotid artery obstruction*
- This condition involves a physical blockage in the carotid arteries, reducing blood flow to the brain, which can cause symptoms similar to those described.
- However, such an obstruction is a **structural problem** and not an acute physiological response to a panic attack in a young patient without other risk factors.
*Decreased respiratory rate*
- Panic attacks are characterized by **hyperventilation**, meaning an increased respiratory rate and depth, not a decreased one.
- A decreased respiratory rate would lead to an **increase in arterial CO2**, which is contrary to the physiological changes seen in a panic attack.
Microcirculation physiology US Medical PG Question 8: An otherwise healthy 65-year-old man comes to the physician for a follow-up visit for elevated blood pressure. Three weeks ago, his blood pressure was 160/80 mmHg. Subsequent home blood pressure measurements at days 5, 10, and 15 found: 165/75 mm Hg, 162/82 mm Hg, and 170/80 mmHg, respectively. He had a cold that was treated with over-the-counter medication 4 weeks ago. Pulse is 72/min and blood pressure is 165/79 mm Hg. Physical examination shows no abnormalities. Laboratory studies, including thyroid function studies, serum electrolytes, and serum creatinine, are within normal limits. Which of the following is the most likely underlying cause of this patient's elevated blood pressure?
- A. Decrease in arterial compliance (Correct Answer)
- B. Increase in left ventricular end-diastolic volume
- C. Increase in aldosterone production
- D. Decrease in baroreceptor sensitivity
- E. Medication-induced vasoconstriction
Microcirculation physiology Explanation: ***Decrease in arterial compliance***
- In elderly patients, **systolic hypertension** (isolated or combined) is commonly caused by **stiffening of the large arteries** (aorta and its major branches), which is a decrease in **arterial compliance**. This leads to a higher systolic pressure needed to eject blood into the stiffened vessels.
- The patient's age (65), persistent elevated systolic blood pressure readings with relatively normal diastolic pressure (though slightly elevated), and the absence of other obvious causes point towards **age-related arterial stiffness**.
*Increase in left ventricular end-diastolic volume*
- An increase in **left ventricular end-diastolic volume (LVEDV)** typically increases **preload** and **cardiac output**, which can contribute to hypertension.
- However, primary hypertension in older adults is more directly linked to **arterial stiffness**, which impacts systolic pressure more profoundly than changes in LVEDV alone.
*Increase in aldosterone production*
- Increased **aldosterone production** (primary hyperaldosteronism) causes hypertension primarily by increasing **sodium and water retention**, leading to **volume expansion** and often accompanied by **hypokalemia**.
- This patient has **normal serum electrolytes**, making primary hyperaldosteronism less likely as the primary cause of his hypertension.
*Decrease in baroreceptor sensitivity*
- A decrease in **baroreceptor sensitivity** can contribute to **blood pressure lability** and impaired compensatory responses to postural changes, but it is not the primary underlying mechanism for sustained, consistently elevated systolic blood pressure in essential hypertension in the elderly.
- While age can affect baroreceptor function, **arterial stiffness** is a more direct cause of the observed systolic hypertension.
*Medication-induced vasoconstriction*
- Some over-the-counter medications, particularly **decongestants** (e.g., pseudoephedrine), can cause **vasoconstriction** and elevate blood pressure.
- However, the patient's cold was 4 weeks ago, and his current symptoms and blood pressure elevations are sustained and occurred *after* the cold resolved and with normal examination, suggesting a more chronic rather than acute medication-induced effect.
Microcirculation physiology US Medical PG Question 9: A 73-year-old woman presents to clinic with a week of fatigue, headache, and swelling of her ankles bilaterally. She reports that she can no longer go on her daily walk around her neighborhood without stopping frequently to catch her breath. At night she gets short of breath and has found that she can only sleep well in her recliner. Her past medical history is significant for hypertension and a myocardial infarction three years ago for which she had a stent placed. She is currently on hydrochlorothiazide, aspirin, and clopidogrel. She smoked 1 pack per day for 30 years before quitting 10 years ago and socially drinks around 1 drink per month. She denies any illicit drug use. Her temperature is 99.0°F (37.2°C), pulse is 115/min, respirations are 18/min, and blood pressure is 108/78 mmHg. On physical exam there is marked elevations of her neck veins, bilateral pitting edema in the lower extremities, and a 3/6 holosystolic ejection murmur over the right sternal border. Echocardiography shows the following findings:
End systolic volume (ESV): 100 mL
End diastolic volume (EDV): 160 mL
How would cardiac output be determined in this patient?
- A. 108/3 + (2 * 78)/3
- B. (160 - 100) / 160
- C. 160 - 100
- D. (160 - 100) * 115 (Correct Answer)
- E. (100 - 160) * 115
Microcirculation physiology Explanation: ***(160 - 100) * 115***
- **Cardiac output (CO)** is calculated as **stroke volume (SV) multiplied by heart rate (HR)**.
- **Stroke volume** is determined by subtracting the **end-systolic volume (ESV)** from the **end-diastolic volume (EDV)** (SV = EDV - ESV).
*(108/3 + (2 * 78)/3)*
- This formula represents the calculation for **mean arterial pressure (MAP)**, which is not directly used to determine cardiac output.
- **MAP** is approximated as (Systolic BP + 2 * Diastolic BP) / 3.
*(160 - 100) / 160*
- This formula calculates the **ejection fraction (EF)**, which is the fraction of blood pumped out of the ventricle with each beat.
- While **ejection fraction** is a crucial measure of cardiac function, it does not directly determine cardiac output.
*160 - 100*
- This calculation represents the **stroke volume (SV)** (EDV - ESV), which is the amount of blood ejected from the ventricle per beat.
- However, to get the **cardiac output**, stroke volume must be multiplied by the heart rate.
*(100 – 160) * 115*
- This calculation would result in a **negative stroke volume**, which is physiologically incorrect as stroke volume must be a positive value.
- **Stroke volume** is always calculated as the **end-diastolic volume minus the end-systolic volume**.
Microcirculation physiology US Medical PG Question 10: An investigator is studying the role of different factors in inflammation and hemostasis. Alpha-granules from activated platelets are isolated and applied to a medium containing inactive platelets. When ristocetin is applied, the granules bind to GpIb receptors, inducing a conformational change in the platelets. Binding of the active component of these granules to GpIb receptors is most likely responsible for which of the following steps of hemostasis?
- A. Local vasoconstriction
- B. Platelet adhesion (Correct Answer)
- C. Platelet activation
- D. Platelet aggregation
- E. Clotting factor activation
Microcirculation physiology Explanation: ***Platelet adhesion***
- The scenario describes ristocetin inducing binding of granule components to **GpIb receptors**, which is the key interaction for **platelet adhesion to von Willebrand factor (vWF)** on exposed subendothelial collagen.
- This initial binding event anchors platelets to the site of vascular injury, forming a primary layer of the hemostatic plug.
*Local vasoconstriction*
- **Vasoconstriction** is primarily mediated by local factors like **endothelin-1** released from damaged endothelial cells, and serotonin and thromboxane A2 released by activated platelets.
- It occurs before platelets adhere and is a separate process intended to reduce blood flow to the injured area.
*Platelet activation*
- While binding to GpIb can *initiate* activation, the GpIb receptor itself is primarily involved in **adhesion**, not the full cascade of activation leading to granule release and conformational changes for aggregation.
- Platelet activation involves intracellular signaling pathways that lead to changes in shape, granule release, and activation of **GpIIb/IIIa receptors**.
*Platelet aggregation*
- **Platelet aggregation** involves the binding of activated **GpIIb/IIIa receptors** to **fibrinogen** (or vWF), linking platelets together.
- The GpIb receptor is specifically for initial adhesion to vWF, not for platelet-to-platelet aggregation.
*Clotting factor activation*
- **Clotting factor activation** is part of the coagulation cascade, leading to the formation of a **fibrin mesh**.
- While activated platelets provide a surface for this to occur, the direct binding of granule components to GpIb receptors is not the mechanism for activating clotting factors.
More Microcirculation physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.