Autoregulation mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Autoregulation mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Autoregulation mechanisms US Medical PG Question 1: A research scientist attempts to understand the influence of carbon dioxide content in blood on its oxygen binding. The scientist adds carbon dioxide to dog blood and measures the uptake of oxygen in the blood versus oxygen pressure in the peripheral tissue. He notes in one dog that with the addition of carbon dioxide with a pressure of 90 mmHg, the oxygen pressure in the peripheral tissue rose from 26 to 33 mmHg. How can this phenomenon be explained?
- A. High partial pressure of CO2 in tissues decreases peripheral blood volume
- B. Binding of O2 to hemoglobin in lungs drives release of CO2 from hemoglobin
- C. High partial pressure of CO2 in tissues causes alkalemia, which is necessary for O2 unloading
- D. High partial pressure of CO2 in tissues facilitates O2 unloading in peripheral tissues (Correct Answer)
- E. The sum of the partial pressures of CO2 and O2 cannot exceed a known threshold in blood
Autoregulation mechanisms Explanation: **High partial pressure of CO2 in tissues facilitates O2 unloading in peripheral tissues**
- An increase in **PCO2** leads to a decrease in pH (acidosis) in the tissues, which **decreases hemoglobin's affinity for oxygen**, promoting oxygen release.
- This phenomenon is known as the **Bohr effect**, where an acidic environment (from CO2) shifts the oxygen dissociation curve to the right, enhancing O2 unloading to meet tissue metabolic demands.
*High partial pressure of CO2 in tissues decreases peripheral blood volume*
- **Increased CO2** generally causes vasodilation in peripheral tissues, which would lead to an **increase**, not a decrease, in peripheral blood flow.
- Decreased blood volume is typically associated with conditions like hypovolemia or intense vasoconstriction, not elevated tissue CO2.
*Binding of O2 to hemoglobin in lungs drives release of CO2 from hemoglobin*
- This statement describes the **Haldane effect**, which occurs primarily in the lungs, where oxygen binding to hemoglobin facilitates the release of CO2.
- While true, it does not explain the **increased oxygen pressure in peripheral tissue** observed with added CO2, which is related to O2 unloading.
*High partial pressure of CO2 in tissues causes alkalemia, which is necessary for O2 unloading*
- High **PCO2** in tissues leads to the formation of carbonic acid and H+ ions, resulting in a **decrease in pH (acidosis)**, not alkalemia.
- **Acidosis** facilitates O2 unloading (Bohr effect), whereas alkalemia would increase hemoglobin's affinity for O2, inhibiting unloading.
*The sum of the partial pressures of CO2 and O2 cannot exceed a known threshold in blood*
- There is **no fixed threshold** for the sum of partial pressures of CO2 and O2 in the blood; these gases are independently regulated and their partial pressures fluctuate with metabolic activity.
- The partial pressure of a gas reflects its concentration and does not have an upper limit when considering the sum of different gases.
Autoregulation mechanisms US Medical PG Question 2: A histological examination of the carotid body reveals glomus cells containing dense-core vesicles. These cells function primarily as chemoreceptors for which of the following?
- A. Partial pressure of oxygen (Correct Answer)
- B. Blood pH
- C. Temperature
- D. Blood glucose levels
Autoregulation mechanisms Explanation: ***Partial pressure of oxygen***
- Carotid body **glomus cells** are highly specialized **chemoreceptors** that primarily sense changes in the **partial pressure of oxygen (PO2)** in arterial blood.
- When PO2 decreases (e.g., hypoxia), these cells are activated and stimulate the respiratory and cardiovascular systems to increase oxygen uptake.
*Blood pH*
- While carotid body chemoreceptors can sense large changes in blood pH, their primary and most sensitive role is in detecting changes in **PO2**.
- Central chemoreceptors in the brainstem are more crucial for routine regulation of respiration in response to changes in **pH and PCO2**.
*Temperature*
- **Thermoreceptors** located in the skin, hypothalamus, and other internal organs are responsible for sensing body temperature, not the carotid body.
- The carotid body's main function is related to blood gas homeostasis, not temperature regulation.
*Blood glucose levels*
- Blood glucose levels are regulated by specialized cells in the **pancreas** (islets of Langerhans) that secrete hormones like insulin and glucagon.
- The carotid body is not directly involved in sensing or regulating glucose homeostasis.
Autoregulation mechanisms US Medical PG Question 3: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Autoregulation mechanisms Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
*Myogenic response*
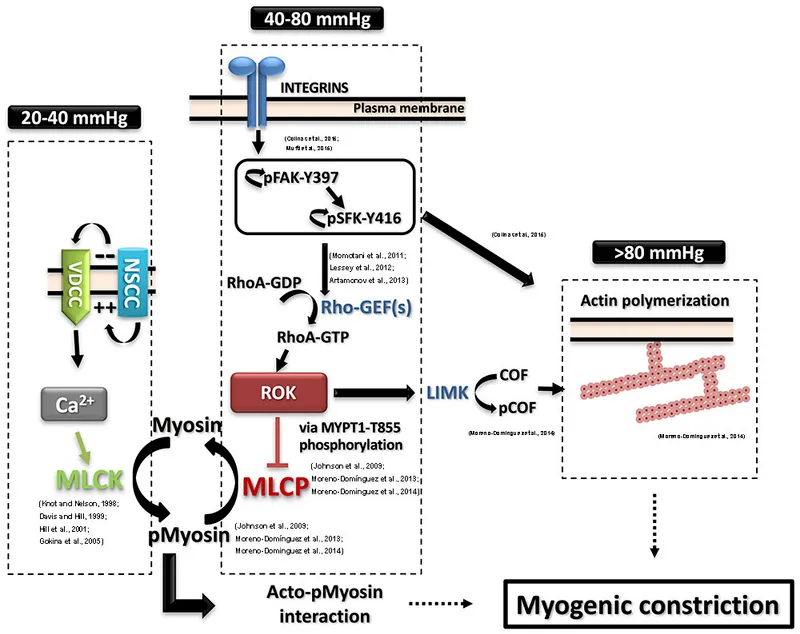
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
Autoregulation mechanisms US Medical PG Question 4: A 26-year-old medical student who is preparing for Step 1 exams is woken up by her friend for breakfast. She realizes that she must have fallen asleep at her desk while attempting to study through the night. While walking with her friend to breakfast, she realizes that she has not eaten since breakfast the previous day. Using this as motivation to review some biochemistry, she pauses to consider what organs are responsible for allowing her to continue thinking clearly in this physiologic state. Which of the following sets of organs are associated with the major source of energy currently facilitating her cognition?
- A. Muscle only
- B. Liver and kidney (Correct Answer)
- C. Liver and muscle
- D. Liver, muscle, and kidney
- E. Liver only
Autoregulation mechanisms Explanation: ***Liver and kidney***
- After an overnight fast (~16-24 hours without food), the **liver** is the **primary organ** responsible for maintaining blood glucose levels through **glycogenolysis** (initially) and **gluconeogenesis** (predominantly at this stage).
- The **kidney** also contributes to **gluconeogenesis** even during an overnight fast, providing approximately **10-15% of total glucose production**. While this contribution is relatively minor compared to the liver, it becomes increasingly important during more prolonged fasting states (>48-72 hours), where it can account for up to 40% of glucose production.
- Since the brain relies almost exclusively on glucose at this stage of fasting (ketone bodies are not yet a major fuel source), both organs that produce glucose for systemic use are correctly identified here.
*Muscle only*
- Muscle glycogen can only be used by the **muscle cells themselves** due to the absence of **glucose-6-phosphatase**, so muscle cannot release free glucose into the bloodstream for use by the brain.
- While muscle does provide amino acids (particularly alanine and glutamine) for gluconeogenesis in the liver and kidney, it does not directly supply glucose to support brain function.
*Liver and muscle*
- As explained above, muscle cannot directly supply glucose to the bloodstream to support brain function due to the lack of **glucose-6-phosphatase**.
- The liver is a major contributor, but muscle is not a direct source of blood glucose.
*Liver, muscle, and kidney*
- This option incorrectly includes muscle as a direct source of glucose for the brain. While liver and kidney both perform gluconeogenesis and release glucose into the bloodstream, muscle lacks this capability.
*Liver only*
- While the liver is indeed the **dominant source** of glucose during an overnight fast (contributing ~85-90% of gluconeogenesis), the **kidney also actively participates** in glucose production, contributing ~10-15% at this stage.
- Since the question asks which organs are "responsible" for maintaining cognition, and both organs contribute to systemic glucose production (even if disproportionately), "liver only" is incomplete.
- The kidney's contribution, though relatively minor during overnight fasting, becomes more substantial during prolonged fasting states.
Autoregulation mechanisms US Medical PG Question 5: Which mechanism primarily regulates sodium reabsorption in the collecting duct?
- A. Glomerulotubular balance
- B. Atrial natriuretic peptide
- C. Antidiuretic hormone
- D. Aldosterone (Correct Answer)
Autoregulation mechanisms Explanation: ***Aldosterone***
- **Aldosterone** is the primary hormone that stimulates **sodium reabsorption** and **potassium secretion** in the principal cells of the collecting duct.
- It acts by increasing the synthesis and activity of **ENaC channels** on the apical membrane and **Na+/K+-ATPase pumps** on the basolateral membrane.
*Glomerulotubular balance*
- **Glomerulotubular balance** refers to the mechanism by which the **proximal tubule** reabsorbs a constant fraction of the filtered load, regardless of changes in glomerular filtration rate (GFR).
- This mechanism maintains a relatively constant delivery of fluid and solutes to downstream segments but does not primarily regulate sodium in the collecting duct.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** primarily **inhibits sodium reabsorption** in the collecting duct, leading to **natriuresis** and **diuresis**, which is the opposite of sodium reabsorption.
- ANP is released in response to atrial stretch, indicating increased blood volume.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)** primarily regulates **water reabsorption** in the collecting duct by increasing the insertion of **aquaporin-2 channels** into the apical membrane, making the collecting duct permeable to water.
- While ADH can indirectly affect sodium concentration by influencing water movement, it does not directly regulate sodium transport to the same extent as aldosterone.
Autoregulation mechanisms US Medical PG Question 6: An investigator is studying muscle contraction in tissue obtained from the thigh muscle of an experimental animal. After injection of radiolabeled ATP, the tissue is stimulated with electrical impulses. Radioassay of these muscle cells is most likely to show greatest activity in which of the following structures?
- A. H zone
- B. M line
- C. A band (Correct Answer)
- D. Z line
- E. I band
Autoregulation mechanisms Explanation: ***A band***
- The **A band** contains the entire length of the **thick myosin filaments** along with the **overlap zone** where myosin and actin interact. Myosin has **ATPase activity**, meaning it binds and hydrolyzes **ATP** to power muscle contraction through cross-bridge cycling.
- Therefore, the greatest accumulation of **radiolabeled ATP** and its breakdown products would be found where **myosin heads** are located throughout the A band.
- The A band represents the most complete answer as it encompasses all regions containing myosin ATPase activity.
*H zone*
- The **H zone** is the central part of the **A band** where only **thick myosin filaments** are present, with no overlap with thin actin filaments.
- While myosin heads with ATPase activity are present here and would show radiolabeled ATP, the **H zone** is only a **subset** of the A band. The **A band** is the more comprehensive answer as it includes both the H zone and the overlap regions where most cross-bridge cycling occurs.
*M line*
- The **M line** is the very center of the **H zone** and anchors the **thick filaments**.
- It consists of structural proteins like **myomesin** and **creatine kinase**. While creatine kinase can phosphorylate ADP to regenerate ATP, it does not directly hydrolyze ATP for muscle contraction the way myosin ATPase does.
*Z line*
- The **Z line** (or Z disc) marks the boundaries of a **sarcomere** and anchors the **thin actin filaments**.
- It contains proteins like **alpha-actinin** and **desmin** but does not directly consume ATP for muscle contraction.
*I band*
- The **I band** contains only **thin actin filaments** and extends from the edge of the A band to the Z line.
- While actin is crucial for contraction, it does not possess **ATPase activity**; ATP hydrolysis primarily occurs at the **myosin heads** located in the A band.
Autoregulation mechanisms US Medical PG Question 7: In the coronary steal phenomenon, vessel dilation is paradoxically harmful because blood is diverted from ischemic areas of the myocardium. Which of the following is responsible for the coronary steal phenomenon?
- A. Venodilation
- B. Microvessel dilation (Correct Answer)
- C. Dilation of the large coronary arteries
- D. Systemic arterial dilation
- E. Volume loss of fluid in the periphery
Autoregulation mechanisms Explanation: ***Microvessel dilation***
- The coronary steal phenomenon occurs when **vasodilators** are administered, causing dilation of **healthy coronary microvessels** and a decrease in resistance.
- This preferentially diverts blood flow away from already **ischemic areas** with maximally dilated intrinsic microvessels, worsening myocardial ischemia.
*Venodilation*
- **Venodilation** primarily reduces **preload** by increasing venous capacitance, not by directly altering coronary microcirculatory blood flow distribution in a way that causes "steal."
- While some vasodilators have venodilatory effects, this specific effect is not the mechanism behind coronary steal.
*Dilation of the large coronary arteries*
- Dilation of large coronary arteries alone doesn't cause the "steal" but rather improves overall blood flow. The critical issue is the differential response of **collateral** and **non-collateral microvessels**.
- **Stenoses** in large coronary arteries are the underlying pathology, but the steal phenomenon itself results from changes in **downstream microvascular resistance**.
*Systemic arterial dilation*
- **Systemic arterial dilation** primarily reduces afterload and can lower blood pressure, but it does not specifically explain the redistribution of coronary blood flow to the detriment of ischemic zones within the myocardium.
- The key to coronary steal is the **heterogeneity of response** at the microvascular level within the coronary circulation.
*Volume loss of fluid in the periphery*
- **Volume loss** in the periphery would influence overall circulatory dynamics and cardiac output but is not directly responsible for the **localized myocardial blood flow redistribution** characteristic of the coronary steal phenomenon.
- Coronary steal is a physiological process related to **vasoreactivity** and not hypovolemia.
Autoregulation mechanisms US Medical PG Question 8: A 38-year-old woman presents to the physician’s clinic with a 6-month history of generalized weakness that usually worsens as the day progresses. She also complains of the drooping of her eyelids and double vision that is worse in the evening. Physical examination reveals bilateral ptosis after a sustained upward gaze and loss of eye convergence which improves upon placing ice packs over the eyes and after the administration of edrophonium. Which of the following is an intrinsic property of the muscle group affected in this patient?
- A. A small mass per motor unit
- B. High ATPase activity (Correct Answer)
- C. High myoglobin content
- D. High density of mitochondria
- E. Increased amount of ATP generated per molecule of glucose
Autoregulation mechanisms Explanation: ***High ATPase activity***
- This patient presents with **myasthenia gravis (MG)**, an autoimmune disorder affecting the neuromuscular junction through antibodies against acetylcholine receptors.
- **Extraocular muscles** and other muscles affected early in MG contain a high proportion of **fast-twitch (Type II) muscle fibers**, which are characterized by **high ATPase activity**.
- **Type II fibers** with high ATPase activity generate rapid, powerful contractions but are **more susceptible to neuromuscular junction dysfunction** due to their higher firing rates and greater dependence on efficient neuromuscular transmission.
- This intrinsic property (high ATPase activity) is why these muscles are preferentially affected in myasthenia gravis.
*A small mass per motor unit*
- While extraocular muscles do have **small motor units** (allowing for precise eye movements), this describes the **innervation pattern** rather than an intrinsic biochemical property of the muscle fibers themselves.
- The question specifically asks about an intrinsic property of the muscle group, referring to the metabolic and contractile characteristics of the muscle fibers.
*High myoglobin content*
- **High myoglobin content** is characteristic of **Type I (slow-twitch) oxidative fibers**, which rely on sustained oxygen delivery for prolonged, fatigue-resistant contractions.
- Muscles preferentially affected in MG have a higher proportion of **Type II fibers**, which have lower myoglobin content compared to Type I fibers.
*High density of mitochondria*
- **High mitochondrial density** is characteristic of **Type I (slow-twitch) oxidative fibers** that depend on aerobic metabolism for sustained energy production.
- While extraocular muscles do have oxidative capacity, the **Type II fibers** preferentially affected in MG have relatively lower mitochondrial density compared to Type I fibers and rely more on glycolytic metabolism for rapid energy needs.
*Increased amount of ATP generated per molecule of glucose*
- **Aerobic respiration** in Type I fibers generates approximately 32 ATP molecules per glucose through oxidative phosphorylation.
- **Type II fibers** rely more heavily on **anaerobic glycolysis**, which produces only 2 ATP per glucose molecule, making them less efficient in ATP generation per glucose.
- The muscles affected in MG have higher proportions of Type II fibers with lower ATP efficiency per glucose molecule.
Autoregulation mechanisms US Medical PG Question 9: A 31-year-old female with a history of anxiety has a panic attack marked by dizziness, weakness, and blurred vision. Which of the following most likely accounts for the patient’s symptoms?
- A. Oxygen toxicity
- B. Increased arterial CO2
- C. Carotid artery obstruction
- D. Decreased cerebral blood flow (Correct Answer)
- E. Decreased respiratory rate
Autoregulation mechanisms Explanation: ***Decreased cerebral blood flow***
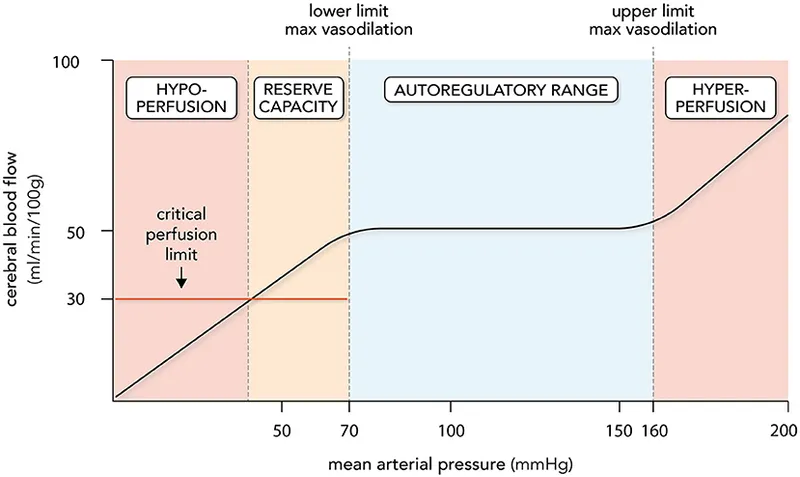
- During a panic attack, **hyperventilation** leads to a drop in arterial CO2, causing **cerebral vasoconstriction** and reduced blood flow to the brain.
- This reduction in cerebral blood flow manifests as neurological symptoms like **dizziness, blurred vision, and weakness**.
*Oxygen toxicity*
- This typically occurs with exposure to **high partial pressures of oxygen**, often in diving or hyperbaric oxygen therapy.
- Symptoms include **seizures, visual changes, and nausea**; it is not associated with panic attacks or their physiological responses.
*Increased arterial CO2*
- Panic attacks involve **hyperventilation**, which causes a decrease, not an increase, in arterial CO2 (hypocapnia).
- Increased arterial CO2 (hypercapnia) usually leads to **vasodilation**, which would increase cerebral blood flow rather than decrease it.
*Carotid artery obstruction*
- This condition involves a physical blockage in the carotid arteries, reducing blood flow to the brain, which can cause symptoms similar to those described.
- However, such an obstruction is a **structural problem** and not an acute physiological response to a panic attack in a young patient without other risk factors.
*Decreased respiratory rate*
- Panic attacks are characterized by **hyperventilation**, meaning an increased respiratory rate and depth, not a decreased one.
- A decreased respiratory rate would lead to an **increase in arterial CO2**, which is contrary to the physiological changes seen in a panic attack.
Autoregulation mechanisms US Medical PG Question 10: An otherwise healthy 65-year-old man comes to the physician for a follow-up visit for elevated blood pressure. Three weeks ago, his blood pressure was 160/80 mmHg. Subsequent home blood pressure measurements at days 5, 10, and 15 found: 165/75 mm Hg, 162/82 mm Hg, and 170/80 mmHg, respectively. He had a cold that was treated with over-the-counter medication 4 weeks ago. Pulse is 72/min and blood pressure is 165/79 mm Hg. Physical examination shows no abnormalities. Laboratory studies, including thyroid function studies, serum electrolytes, and serum creatinine, are within normal limits. Which of the following is the most likely underlying cause of this patient's elevated blood pressure?
- A. Decrease in arterial compliance (Correct Answer)
- B. Increase in left ventricular end-diastolic volume
- C. Increase in aldosterone production
- D. Decrease in baroreceptor sensitivity
- E. Medication-induced vasoconstriction
Autoregulation mechanisms Explanation: ***Decrease in arterial compliance***
- In elderly patients, **systolic hypertension** (isolated or combined) is commonly caused by **stiffening of the large arteries** (aorta and its major branches), which is a decrease in **arterial compliance**. This leads to a higher systolic pressure needed to eject blood into the stiffened vessels.
- The patient's age (65), persistent elevated systolic blood pressure readings with relatively normal diastolic pressure (though slightly elevated), and the absence of other obvious causes point towards **age-related arterial stiffness**.
*Increase in left ventricular end-diastolic volume*
- An increase in **left ventricular end-diastolic volume (LVEDV)** typically increases **preload** and **cardiac output**, which can contribute to hypertension.
- However, primary hypertension in older adults is more directly linked to **arterial stiffness**, which impacts systolic pressure more profoundly than changes in LVEDV alone.
*Increase in aldosterone production*
- Increased **aldosterone production** (primary hyperaldosteronism) causes hypertension primarily by increasing **sodium and water retention**, leading to **volume expansion** and often accompanied by **hypokalemia**.
- This patient has **normal serum electrolytes**, making primary hyperaldosteronism less likely as the primary cause of his hypertension.
*Decrease in baroreceptor sensitivity*
- A decrease in **baroreceptor sensitivity** can contribute to **blood pressure lability** and impaired compensatory responses to postural changes, but it is not the primary underlying mechanism for sustained, consistently elevated systolic blood pressure in essential hypertension in the elderly.
- While age can affect baroreceptor function, **arterial stiffness** is a more direct cause of the observed systolic hypertension.
*Medication-induced vasoconstriction*
- Some over-the-counter medications, particularly **decongestants** (e.g., pseudoephedrine), can cause **vasoconstriction** and elevate blood pressure.
- However, the patient's cold was 4 weeks ago, and his current symptoms and blood pressure elevations are sustained and occurred *after* the cold resolved and with normal examination, suggesting a more chronic rather than acute medication-induced effect.
More Autoregulation mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.