Hemodynamics

On this page
🌊 The Hemodynamic Engine: Mastering Cardiovascular Flow Dynamics
You'll master how blood moves through the cardiovascular system by understanding the physics of pressure, resistance, and flow that sustain every organ. This lesson builds from foundational principles through clinical pattern recognition, teaching you to identify shock states, interpret hemodynamic profiles, and select evidence-based interventions. You'll learn to integrate cardiovascular dynamics with respiratory, renal, and metabolic systems, developing the diagnostic precision needed to stabilize critically ill patients and optimize tissue perfusion in real time.
📌 Remember: PQRST - Pressure drives flow, Quantified by resistance, Regulated by vessels, Systemic circulation dominates, Tissue perfusion is the goal
-
Pressure Gradient: The driving force (ΔP = P₁ - P₂)
- Systemic: 100 mmHg (aortic) → 0 mmHg (right atrium)
- Pulmonary: 25 mmHg (pulmonary artery) → 5 mmHg (left atrium)
- Coronary: 80 mmHg during diastole for perfusion
-
Flow Dynamics: Governed by Poiseuille's Law
- Flow ∝ r⁴ (radius to the fourth power)
- 50% radius reduction = 94% flow decrease
- Normal cardiac output: 5-6 L/min at rest

| Parameter | Systemic | Pulmonary | Coronary | Cerebral | Renal |
|---|---|---|---|---|---|
| Pressure (mmHg) | 100/0 | 25/5 | 80/0 | 50/10 | 60/5 |
| Resistance (PRU) | 15-20 | 1-3 | 0.5-1.0 | 2-4 | 1-2 |
| Flow (mL/min) | 5000 | 5000 | 250 | 750 | 1200 |
| Autoregulation | Moderate | Minimal | Excellent | Excellent | Excellent |
| Compliance | Low | High | Low | Low | Moderate |
The cardiovascular system operates as an integrated circuit where total peripheral resistance determines afterload, venous return governs preload, and cardiac contractility modulates stroke volume. Master these relationships to predict hemodynamic responses in any clinical scenario.
🌊 The Hemodynamic Engine: Mastering Cardiovascular Flow Dynamics
⚙️ The Pressure-Flow Powerhouse: Cardiovascular Physics in Action
-
Cardiac Output Determinants:
- Heart Rate: 60-100 bpm (normal range)
- Stroke Volume: 70 mL per beat
- Ejection Fraction: 55-70% (normal)
- End-diastolic volume: 120-140 mL
-
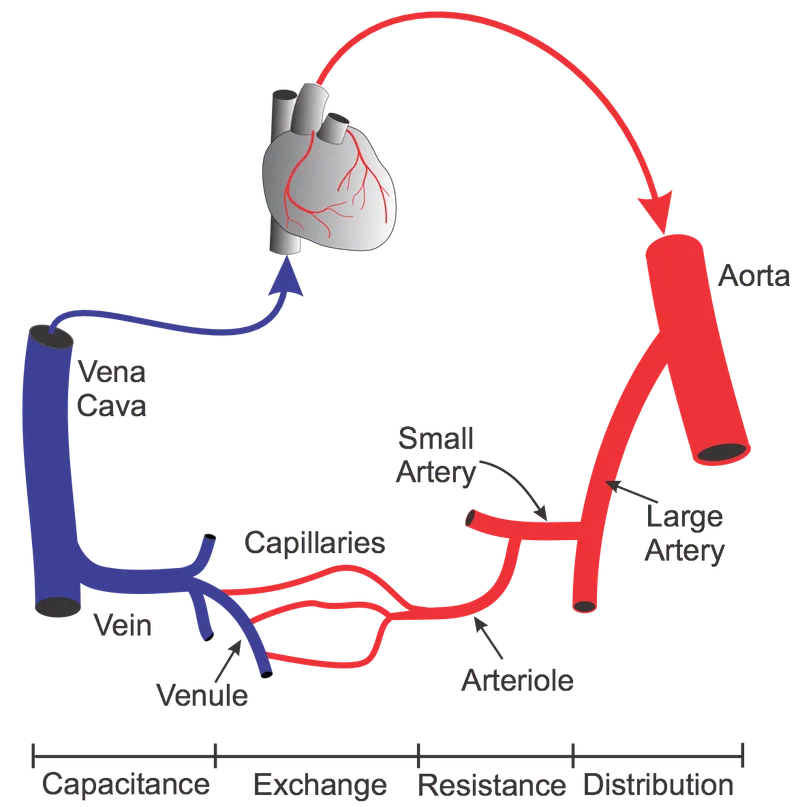
Vascular Resistance Components:
- Arterioles: 50% of total resistance
- Capillaries: 25% of total resistance
- Venules: 15% of total resistance
- Large arteries/veins: 10% of total resistance
📌 Remember: RAMP - Resistance in arterioles, Afterload from pressure, Mean pressure drives flow, Perfusion requires adequate MAP
⭐ Clinical Pearl: Systemic vascular resistance (SVR) = (MAP - CVP) × 80/CO. Normal range 800-1200 dynes·sec/cm⁵. Values >1500 indicate vasoconstriction; <600 suggest vasodilation.
The pressure-flow relationship becomes non-linear during pathological states. Critical closing pressure (20-30 mmHg) represents the minimum pressure required to maintain flow, explaining why MAP targets matter more than systolic pressure alone.
💡 Master This: Understanding pressure-flow dynamics predicts every hemodynamic intervention. Vasopressors increase resistance and pressure, while vasodilators reduce afterload but may compromise perfusion pressure.
⚙️ The Pressure-Flow Powerhouse: Cardiovascular Physics in Action
🎯 The Clinical Recognition Matrix: Hemodynamic Pattern Mastery

Master the "hemodynamic fingerprint" - each shock state creates distinct patterns of pressure, flow, and resistance that guide immediate therapeutic decisions.
-
Hypovolemic Shock Pattern:
- CVP: ↓ (<8 mmHg)
- PCWP: ↓ (<12 mmHg)
- SVR: ↑ (>1200 dynes·sec/cm⁵)
- Cardiac Index: ↓ (<2.5 L/min/m²)
-
Cardiogenic Shock Pattern:
- CVP: ↑ (>12 mmHg)
- PCWP: ↑ (>18 mmHg)
- SVR: ↑ (>1200 dynes·sec/cm⁵)
- Cardiac Index: ↓ (<2.2 L/min/m²)
📌 Remember: SHOCK - SVR tells the story, Heart pressures reveal pump function, Output measures delivery, CVP shows volume status, Key is pattern recognition

| Shock Type | CVP | PCWP | SVR | CI | Treatment Priority |
|---|---|---|---|---|---|
| Hypovolemic | ↓ | ↓ | ↑ | ↓ | Volume resuscitation |
| Cardiogenic | ↑ | ↑ | ↑ | ↓ | Inotropes/afterload reduction |
| Distributive | ↓ | ↓ | ↓ | ↑ | Vasopressors |
| Obstructive | ↑ | Variable | ↑ | ↓ | Remove obstruction |
| Mixed | Variable | Variable | Variable | ↓ | Targeted therapy |
💡 Master This: The hemodynamic profile reveals the underlying pathophysiology. Never treat numbers in isolation - the pattern tells the story and guides therapy.
🎯 The Clinical Recognition Matrix: Hemodynamic Pattern Mastery
🔬 The Hemodynamic Discrimination Engine: Differential Diagnosis Mastery
- Distributive vs. Hypovolemic Shock Discrimination:
- Skin temperature: Warm vs. cool
- Capillary refill: <2 sec vs. >3 sec
- Urine output: Variable vs. consistently ↓
- Response to fluids: Minimal vs. dramatic
- Lactate pattern: Early ↑ vs. late ↑
📌 Remember: WARM-COOL - Warm skin suggests distributive, Assess capillary refill, Response to fluids differs, Metabolic acidosis timing varies, Cardiac output patterns opposite, Organ perfusion mechanisms differ, Outcome depends on recognition, Lactate clearance predicts survival
| Parameter | Distributive | Hypovolemic | Cardiogenic | Obstructive |
|---|---|---|---|---|
| Cardiac Index | ↑ (>4.0) | ↓ (<2.5) | ↓ (<2.2) | ↓ (<2.5) |
| SVR | ↓ (<800) | ↑ (>1200) | ↑ (>1200) | ↑ (>1200) |
| Mixed Venous O₂ | ↑ (>70%) | ↓ (<65%) | ↓ (<60%) | ↓ (<65%) |
| Lactate Clearance | Slow | Rapid with volume | Poor | Variable |
| Fluid Responsiveness | Minimal | Excellent | Harmful | Variable |
- Stroke Volume Variation (SVV): >13% indicates preload dependence
- dP/dt max: <1200 mmHg/sec suggests contractile dysfunction
- Systolic Pressure Variation (SPV): >10 mmHg indicates volume depletion
- Central Venous O₂ Saturation: <70% suggests inadequate oxygen delivery
⭐ Clinical Pearl: Pulse pressure (PP) = SBP - DBP narrows in shock states. PP <25% of SBP indicates severe hemodynamic compromise. Normal PP is 30-40 mmHg.
💡 Master This: Hemodynamic discrimination requires integration of multiple parameters. Single values mislead; patterns reveal truth. The combination of cardiac output, filling pressures, and vascular resistance creates unique fingerprints for each shock state.
🔬 The Hemodynamic Discrimination Engine: Differential Diagnosis Mastery
⚕️ The Hemodynamic Treatment Algorithm: Evidence-Based Intervention Mastery
-
Fluid Resuscitation Protocols:
- Initial bolus: 30 mL/kg crystalloid within 3 hours
- Fluid responsiveness: SVV >13% or PPV >13%
- Fluid challenge: 500 mL over 15 minutes
- Stop point: CVP >12 mmHg or PCWP >18 mmHg
-
Vasopressor Selection & Dosing:
- Norepinephrine: First-line, 0.1-0.5 mcg/kg/min
- Vasopressin: Add at 0.03-0.04 units/min (fixed dose)
- Epinephrine: Second-line, 0.1-0.5 mcg/kg/min
- Phenylephrine: Pure α-agonist, 0.5-5 mcg/kg/min
| Intervention | Indication | Target | Success Rate | Monitoring |
|---|---|---|---|---|
| Fluid Challenge | SVV >13% | ↑SV by 15% | 85% | Dynamic parameters |
| Norepinephrine | MAP <65 | MAP 65-75 | 90% | Lactate clearance |
| Dobutamine | CI <2.5 | CI >2.5 | 75% | Mixed venous O₂ |
| Milrinone | High SVR + Low CI | ↓SVR, ↑CI | 70% | Arrhythmia risk |
| IABP | Cardiogenic shock | ↑DBP, ↓afterload | 60% | Limb ischemia |
⭐ Clinical Pearl: Lactate clearance >10% per hour predicts survival better than achieving MAP targets. ScvO₂ >70% indicates adequate oxygen delivery in most patients.
- Advanced Hemodynamic Support:
- ECMO: Bridge therapy, 30-50% survival in cardiogenic shock
- Impella: 2.5-5.5 L/min support, 40-60% survival
- IABP: 10-15% cardiac output augmentation
- Temporary pacing: 100% capture threshold <2 mA
💡 Master This: Hemodynamic treatment success depends on early recognition, appropriate intervention sequencing, and continuous monitoring. The goal is tissue perfusion, not just pressure targets.
⚕️ The Hemodynamic Treatment Algorithm: Evidence-Based Intervention Mastery
🌐 The Hemodynamic Integration Network: Multi-System Orchestration Mastery
- Integrated Hemodynamic Control Systems:
- Baroreceptor reflex: 1-2 second response time
- Chemoreceptor activation: 5-10 second response
- Renin-angiotensin system: 10-60 minute response
- Vasopressin release: Minutes to hours response
- Aldosterone effects: Hours to days response
📌 Remember: BRAIN - Baroreceptors respond fastest, Renin-angiotensin intermediate, Aldosterone slowest, Integration creates stability, Neural control dominates acute responses
| System | Response Time | Mechanism | Effectiveness | Clinical Relevance |
|---|---|---|---|---|
| Baroreceptor | 1-2 sec | Neural | 85% | Orthostatic tolerance |
| Chemoreceptor | 5-10 sec | Neural | 70% | Hypoxic response |
| Myogenic | 10-30 sec | Local | 90% | Autoregulation |
| Metabolic | 30-60 sec | Local | 95% | Exercise response |
| Hormonal | 10-60 min | Systemic | 80% | Volume regulation |
- Glycocalyx dysfunction: Reduces NO bioavailability by 40%
- Endothelial mechanotransduction: Shear stress >15 dynes/cm² maintains health
- Microcirculatory heterogeneity: 30% of capillaries may be non-perfused in shock
- Venous-arterial CO₂ gap: >6 mmHg indicates inadequate tissue perfusion
⭐ Clinical Pearl: Heart rate variability (HRV) reflects autonomic balance. RMSSD <20 ms indicates sympathetic dominance and poor prognosis in critically ill patients.
The hemodynamic reserve concept explains why some patients tolerate massive blood loss while others decompensate rapidly. Physiological reserve depends on age, comorbidities, and baseline cardiovascular fitness.
💡 Master This: Hemodynamic integration reveals why isolated parameter optimization fails. Success requires understanding the network effects where improving one parameter may compromise others. Systems thinking transforms hemodynamic management from reactive to predictive.
🌐 The Hemodynamic Integration Network: Multi-System Orchestration Mastery
🎯 The Hemodynamic Mastery Arsenal: Clinical Command Center
📌 Essential Numbers Arsenal: MAP >65, CI >2.5, SVR 800-1200, CVP 8-12, PCWP 12-18, SvO₂ >65%, Lactate <2, PPV <13%
- Rapid Assessment Protocol:
- Step 1: MAP - Is perfusion pressure adequate?
- Step 2: Cardiac output - Is pump function sufficient?
- Step 3: Filling pressures - Is preload optimized?
- Step 4: Tissue perfusion - Are endpoints met?
| Clinical Scenario | Key Parameters | Immediate Action | Target Endpoint |
|---|---|---|---|
| Hypotension | MAP, SVR, CO | Fluid vs. pressor | MAP >65 mmHg |
| Low output | CI, PCWP, EF | Preload vs. inotrope | CI >2.5 L/min/m² |
| Poor perfusion | Lactate, SvO₂ | Optimize delivery | Lactate clearance |
| Volume overload | CVP, PCWP | Diuresis vs. ultrafiltration | Euvolemia |
| Shock state | All parameters | Protocol-driven | Multi-target |
💡 Master This: Hemodynamic mastery requires pattern recognition, physiological understanding, and therapeutic precision. The expert clinician sees the integrated picture where novices see isolated numbers.
🎯 The Hemodynamic Mastery Arsenal: Clinical Command Center
Practice Questions: Hemodynamics
Test your understanding with these related questions
A peripheral artery is found to have 50% stenosis (50% reduction in cross-sectional area). Therefore, compared to a normal artery with no stenosis, by what factor has the flow of blood been decreased?













