Starling forces in glomerular filtration US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Starling forces in glomerular filtration. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Starling forces in glomerular filtration US Medical PG Question 1: A 55-year-old woman presents to a physician’s clinic for a diabetes follow-up. She recently lost weight and believes the diabetes is ‘winding down’ because the urinary frequency has slowed down compared to when her diabetes was "at its worst". She had been poorly compliant with medications, but she is now asking if she can decrease her medications as she feels like her diabetes is improving. Due to the decrease in urinary frequency, the physician is interested in interrogating her renal function. Which substance can be used to most accurately assess the glomerular filtration rate (GFR) in this patient?
- A. Para-aminohippurate (PAH)
- B. Glucose
- C. Inulin (Correct Answer)
- D. Urea
- E. Creatinine
Starling forces in glomerular filtration Explanation: ***Correct Answer: Inulin***
- **Inulin** is freely filtered by the glomeruli and is neither reabsorbed nor secreted by the renal tubules, making its clearance rate an **accurate measure of GFR**.
- It is considered the **gold standard** for GFR measurement, although it is not routinely used in clinical practice due to its exogenous nature and the need for continuous infusion.
*Incorrect: Para-aminohippurate (PAH)*
- **PAH** is both filtered and actively secreted by the renal tubules, meaning its clearance reflects **renal plasma flow**, not GFR.
- Due to its high extraction fraction, it is used to measure **effective renal plasma flow (ERPF)**.
*Incorrect: Glucose*
- **Glucose** is freely filtered by the glomeruli but is almost completely reabsorbed in the proximal convoluted tubule in healthy individuals, especially at normal blood glucose levels.
- Therefore, glucose clearance is typically **zero** and does not measure GFR.
*Incorrect: Urea*
- **Urea** is filtered by the glomeruli, but a significant portion is **reabsorbed** by the renal tubules, particularly in states of lower urine flow.
- Its clearance **underestimates GFR** and varies with hydration status and protein intake, making it an unreliable sole measure of GFR.
*Incorrect: Creatinine*
- **Creatinine** is freely filtered by the glomeruli, but a small amount is also **secreted** by the renal tubules, leading to an overestimation of GFR, especially in advanced kidney disease.
- Although commonly used as an **estimate of GFR** in clinical practice due to its endogenous production, it is not as accurate as inulin.
Starling forces in glomerular filtration US Medical PG Question 2: Which factor most strongly influences protein filtration at the glomerulus?
- A. Electrical charge
- B. Molecular size (Correct Answer)
- C. Shape
- D. Temperature
Starling forces in glomerular filtration Explanation: ***Molecular size***
- The glomerular filtration barrier, particularly the **slit diaphragms** between podocytes, acts as a size-selective filter, restricting the passage of larger molecules.
- Proteins like **albumin** (molecular radius ~36 Å, molecular weight ~69 kDa) are significantly large, making them difficult to pass through the filtration barrier.
- Size selectivity is the **primary and most important** factor in protein filtration.
*Electrical charge*
- The glomerular basement membrane contains **negatively charged proteoglycans** (heparan sulfate), which repel negatively charged proteins like albumin, contributing to their retention.
- While important, the role of electrical charge is **secondary** to molecular size in preventing the bulk passage of most proteins.
*Shape*
- While abnormal protein shapes (e.g., **amyloid fibrils**) can impact filtration in specific disease states, the typical physiological filtration of most proteins is primarily governed by size and charge.
- The inherent shape of normal globular proteins plays a less direct role compared to their overall size.
*Temperature*
- **Physiological temperature** is relatively constant in the body and does not directly influence the molecular interactions and physical properties of the glomerular filtration barrier in a way that significantly alters protein filtration.
- Temperature changes would lead to denaturation or aggregation, which are not the primary determinants of normal protein filtration.
Starling forces in glomerular filtration US Medical PG Question 3: A 45-year-old man presents with a 3-day history of right-sided flank pain due to a lodged ureteral stone. What changes would be expected to be seen at the level of glomerular filtration?
- A. Increase in glomerular capillary oncotic pressure
- B. Increase in Bowman's space oncotic pressure
- C. Increase in filtration fraction
- D. Increase in Bowman's space hydrostatic pressure (Correct Answer)
- E. No change in filtration fraction
Starling forces in glomerular filtration Explanation: ***Increase in Bowman's space hydrostatic pressure***
- A lodged ureteral stone causes **obstruction** of urine flow, leading to a backup of fluid in the renal tubules and eventually into **Bowman's space**.
- This increased fluid volume in Bowman's space directly raises its **hydrostatic pressure**, which opposes glomerular filtration, thereby reducing the net filtration pressure.
*Increase in glomerular capillary oncotic pressure*
- **Glomerular capillary oncotic pressure** primarily reflects the protein concentration within the glomerular capillaries, which would not be directly increased by a ureteral stone.
- This parameter typically rises when fluid is filtered out, increasing protein concentration in the remaining blood, but not as the initial insult from obstruction.
*Increase in Bowman's space oncotic pressure*
- **Bowman's space oncotic pressure** is normally very low because the glomerular filtration barrier prevents significant protein filtration.
- An increase in this pressure would imply increased protein leakage into Bowman's space, which is not a direct consequence of a ureteral obstruction.
*Increase in filtration fraction*
- The **filtration fraction** is the ratio of glomerular filtration rate (GFR) to renal plasma flow.
- Ureteral obstruction typically **decreases GFR** due to increased Bowman's space hydrostatic pressure, which would lead to a reduction, not an increase, in the filtration fraction, assuming renal plasma flow remains stable or slightly reduced.
*No change in filtration fraction*
- Ureteral obstruction significantly impacts the forces driving glomerular filtration, primarily by increasing **Bowman's space hydrostatic pressure**.
- This change inevitably leads to a **decrease in GFR**, thus altering the filtration fraction, meaning it would not remain unchanged.
Starling forces in glomerular filtration US Medical PG Question 4: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Starling forces in glomerular filtration Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
Starling forces in glomerular filtration US Medical PG Question 5: A 70-year-old female with chronic kidney failure secondary to diabetes asks her nephrologist to educate her about the techniques used to evaluate the degree of kidney failure progression. She learns about the concept of glomerular filtration rate (GFR) and learns that it can be estimated by measuring the levels of some substances. The clearance of which of the following substances is the most accurate estimate for GFR?
- A. Paraaminohippurate (PAH)
- B. Sodium
- C. Inulin (Correct Answer)
- D. Creatinine
- E. Glucose
Starling forces in glomerular filtration Explanation: ***Inulin***
- **Inulin** is freely filtered by the glomeruli and is neither reabsorbed nor secreted by the renal tubules, making its clearance the **gold standard** for accurately measuring GFR.
- Due to its ideal physiological properties, inulin clearance perfectly reflects the rate at which plasma is filtered by the kidneys.
*Paraaminohippurate (PAH)*
- **PAH** is almost completely cleared from the blood by both glomerular filtration and **tubular secretion**, making its clearance an accurate measure of **renal plasma flow (RPF)**, not GFR.
- While important for assessing renal blood flow, it does not directly reflect the filtration capacity of the glomeruli.
*Sodium*
- **Sodium** is freely filtered at the glomerulus, but a significant portion (approximately **99%**) is **reabsorbed** by the renal tubules.
- Its clearance is highly variable and depends on various physiological factors, making it unsuitable for GFR estimation.
*Creatinine*
- **Creatinine** is freely filtered by the glomeruli and is also **modestly secreted** by the renal tubules, leading to an **overestimation of GFR** at lower kidney function levels.
- Despite being the most commonly used clinical marker due to its endogenous production, its tubular secretion makes it less accurate than inulin.
*Glucose*
- **Glucose** is freely filtered by the glomeruli but is almost **completely reabsorbed** by the renal tubules under normal physiological conditions.
- Its presence in urine (glycosuria) indicates a high plasma glucose level or tubular reabsorption defects, not a measure of GFR.
Starling forces in glomerular filtration US Medical PG Question 6: A 75-year-old woman is brought to a physician’s office by her son with complaints of diarrhea and vomiting for 1 day. Her stool is loose, watery, and yellow-colored, while her vomitus contains partially digested food particles. She denies having blood or mucus in her stools and vomitus. Since the onset of her symptoms, she has not had anything to eat and her son adds that she is unable to tolerate fluids. The past medical history is unremarkable and she does not take any medications regularly. The pulse is 115/min, the respiratory rate is 16/min, the blood pressure is 100/60 mm Hg, and the temperature is 37.0°C (98.6°F). The physical examination shows dry mucous membranes and slightly sunken eyes. The abdomen is soft and non-tender. Which of the following physiologic changes in glomerular filtration rate (GFR), renal plasma flow (RPF), and filtration fraction (FF) are expected?
- A. Decreased GFR, decreased RPF, decreased FF
- B. Decreased GFR, decreased RPF, no change in FF
- C. Increased GFR, increased RPF, increased FF
- D. Increased GFR, decreased RPF, increased FF
- E. Decreased GFR, decreased RPF, increased FF (Correct Answer)
Starling forces in glomerular filtration Explanation: ***Decreased GFR, decreased RPF, increased FF***
- Due to **dehydration** from diarrhea and vomiting, there is a decrease in blood volume leading to decreased renal blood flow and **renal plasma flow (RPF)**.
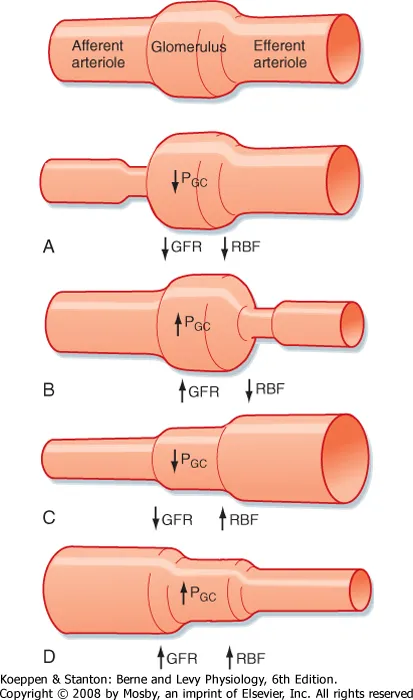
- The body responds to hypovolemia by activating the renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system, which cause **preferential efferent arteriolar constriction** (more than afferent constriction). This helps maintain glomerular hydrostatic pressure despite reduced renal perfusion.
- As a result, **GFR decreases** but proportionally **less than RPF decreases**, causing the **filtration fraction (FF = GFR/RPF) to increase**.
- In this patient with significant dehydration (tachycardia, hypotension, dry mucous membranes), both GFR and RPF are reduced, but FF is elevated due to compensatory mechanisms.
*Decreased GFR, decreased RPF, decreased FF*
- While GFR and RPF will decrease due to dehydration, the **filtration fraction is expected to increase**, not decrease.
- A decreased FF would imply GFR fell proportionally more than RPF, which contradicts the physiologic response where efferent arteriolar constriction helps preserve GFR relative to RPF.
*Decreased GFR, decreased RPF, no change in FF*
- With significant fluid loss and compensatory mechanisms (efferent arteriolar constriction via angiotensin II), a change in **filtration fraction** is expected.
- The body actively alters arteriolar tone to prioritize GFR maintenance, which directly increases FF.
*Increased GFR, increased RPF, increased FF*
- This pattern suggests **hypervolemia** or increased renal perfusion, which directly contradicts the patient's severe dehydration.
- Both GFR and RPF are expected to decrease in volume depletion, not increase.
*Increased GFR, decreased RPF, increased FF*
- An increase in GFR is physiologically impossible given the patient's severe volume depletion and reduced renal perfusion.
- While FF does increase in dehydration, this occurs in the context of **both GFR and RPF being decreased**, not with an increased GFR.
Starling forces in glomerular filtration US Medical PG Question 7: A researcher is investigating the effects of a new antihypertensive medication on renal physiology. She gives a subject a dose of the new medication, and she then collects plasma and urine samples. She finds the following: Hematocrit: 40%; Serum creatinine: 0.0125 mg/mL; Urine creatinine: 1.25 mg/mL. Urinary output is 1 mL/min. Renal blood flow is 1 L/min. Based on the above information and approximating that the creatinine clearance is equal to the GFR, what answer best approximates filtration fraction in this case?
- A. 10%
- B. 17% (Correct Answer)
- C. 33%
- D. 50%
- E. 25%
Starling forces in glomerular filtration Explanation: ***17%***
- First, calculate **GFR** using the creatinine clearance formula: GFR = (Urine creatinine × Urinary output) / Serum creatinine = (1.25 mg/mL × 1 mL/min) / 0.0125 mg/mL = **100 mL/min**.
- Next, calculate **Renal Plasma Flow (RPF)** from Renal Blood Flow (RBF) and Hematocrit: RPF = RBF × (1 - Hematocrit) = 1000 mL/min × (1 - 0.40) = **600 mL/min**.
- Finally, calculate **Filtration Fraction (FF)** = GFR / RPF = 100 mL/min / 600 mL/min = 0.1667 = **16.7%, which approximates to 17%**.
- This is the correct answer based on the physiological calculations and represents a normal filtration fraction.
*10%*
- This would correspond to a filtration fraction of 0.10, which would require either a GFR of 60 mL/min (lower than calculated) or an RPF of 1000 mL/min (higher than calculated).
- This value is too low given the provided parameters and doesn't match the calculation from the given data.
*25%*
- This value would suggest FF = 0.25, requiring a GFR of 150 mL/min with the calculated RPF of 600 mL/min.
- This is higher than the calculated GFR of 100 mL/min and doesn't match the given creatinine values.
*33%*
- This would imply FF = 0.33, requiring a GFR of approximately 200 mL/min with RPF of 600 mL/min.
- This is significantly higher than the calculated GFR and would represent an abnormally elevated filtration fraction.
*50%*
- A filtration fraction of 50% is unphysiologically high and would indicate severe pathology.
- This would require a GFR of 300 mL/min with the calculated RPF, which is impossible given the provided creatinine clearance data.
Starling forces in glomerular filtration US Medical PG Question 8: A 48-year-old woman comes to the physician for a follow-up examination. At her visit 1 month ago, her glomerular filtration rate (GFR) was 100 mL/min/1.73 m2 and her renal plasma flow (RPF) was 588 mL/min. Today, her RPF is 540 mL/min and her filtration fraction (FF) is 0.2. After her previous appointment, this patient was most likely started on a drug that has which of the following effects?
- A. Inhibition of the renal Na-K-Cl cotransporter
- B. Constriction of the afferent arteriole
- C. Relaxation of urinary smooth muscle
- D. Constriction of the efferent arteriole (Correct Answer)
- E. Inhibition of vasopressin
Starling forces in glomerular filtration Explanation: ***Constriction of the efferent arteriole***
- The previous GFR was 100 mL/min and RPF was 588 mL/min. For the follow-up, RPF is 540 mL/min and FF is 0.2. The new GFR can be calculated as FF × RPF = 0.2 × 540 = **108 mL/min**.
- The patient shows **increased GFR** (100→108 mL/min) with **decreased RPF** (588→540 mL/min), resulting in an **increased filtration fraction**.
- Medications that **constrict the efferent arteriole**, such as **NSAIDs**, produce this pattern by blocking prostaglandin synthesis. Prostaglandins normally cause vasodilation (predominantly of the afferent arteriole). When blocked, there is relatively more **efferent arteriolar constriction**, which increases glomerular hydrostatic pressure, thereby **increasing GFR while reducing overall RPF**.
*Inhibition of the renal Na-K-Cl cotransporter*
- This effect describes **loop diuretics** (e.g., furosemide), which increase sodium excretion and water diuresis.
- Loop diuretics typically cause a **decrease in GFR** due to reduced fluid volume and lower filtration pressure, which contradicts the slight increase in GFR observed.
*Constriction of the afferent arteriole*
- **Afferent arteriole constriction** (e.g., by NSAIDs in high doses or norepinephrine) would decrease blood flow into the glomerulus, leading to a **decrease in both RPF and GFR**.
- While RPF decreased in this case, GFR actually increased, making this option incorrect.
*Relaxation of urinary smooth muscle*
- Relaxation of urinary smooth muscle is characteristic of drugs like **alpha-blockers** (e.g., tamsulosin) or antimuscarinics used for conditions like benign prostatic hyperplasia or overactive bladder.
- This effect primarily impacts urine flow out of the bladder and does **not directly affect GFR or RPF** in the way described.
*Inhibition of vasopressin*
- Vasopressin (ADH) inhibition leads to **increased water excretion** and is seen with drugs like **vasopressin receptor antagonists** (vaptans) or ethanol.
- While it affects fluid balance, it typically causes a **decrease in GFR** due to hypovolemia and has no direct mechanism to increase GFR with decreased RPF as observed.
Starling forces in glomerular filtration US Medical PG Question 9: A 76-year-old woman presents to the office with a generalized weakness for the past month. She has a past medical history significant for uncontrolled hypertension and type 2 diabetes mellitus. Her temperature is 37.0°C (98.6°F), blood pressure is 135/82 mm Hg, pulse is 90/min, respiratory rate is 17/min, and oxygen saturation is 99% on room air. Physical exam shows no remarkable findings. Her last recorded glomerular filtration rate was 30 mL/min. A radiograph of the patient’s hand is given. Which of the following lab findings is most likely to be found in this patient?
- A. Increased PTH, decreased calcium, increased phosphate (Correct Answer)
- B. Increased PTH, decreased calcium, decreased phosphate
- C. Normal PTH, increased calcium, normal phosphate
- D. Increased PTH, increased calcium, decreased phosphate
- E. Increased PTH, increased calcium, increased phosphate
Starling forces in glomerular filtration Explanation: ***Increased PTH, decreased calcium, increased phosphate***
- The patient's **glomerular filtration rate (GFR) of 30 mL/min** indicates **Stage 4 chronic kidney disease (CKD)**. In CKD, the kidneys are unable to adequately excrete phosphate, leading to **hyperphosphatemia**.
- Hyperphosphatemia leads to the formation of calcium-phosphate complexes, causing a decrease in free calcium (hypocalcemia) by precipitating out. Additionally, damaged kidneys cannot convert vitamin D into its active form, which further reduces calcium absorption from the gut and bone, contributing to hypocalcemia. This persistent hypocalcemia stimulates the parathyroid glands to produce more **parathyroid hormone (PTH)**, resulting in **secondary hyperparathyroidism**.
*Increased PTH, decreased calcium, decreased phosphate*
- This pattern of laboratory findings is characteristic of **primary hyperparathyroidism**, where an adenoma or hyperplasia of the parathyroid glands leads to excessive PTH production.
- In primary hyperparathyroidism, elevated PTH causes increased bone resorption and renal phosphate excretion, typically resulting in **hypercalcemia** and **hypophosphatemia**.
*Normal PTH, increased calcium, normal phosphate*
- This combination is not typically seen in CKD-related mineral and bone disorder.
- While hypercalcemia can occur in some conditions, normal PTH with increased calcium often points toward conditions like **paraneoplastic syndromes** or **granulomatous diseases** producing PTH-related protein, or **vitamin D intoxication**.
*Increased PTH, increased calcium, decreased phosphate*
- This specific combination (high PTH, high calcium, low phosphate) is the classic hallmark of **primary hyperparathyroidism**.
- In contrast, secondary hyperparathyroidism due to CKD typically presents with **hypocalcemia** and **hyperphosphatemia** due to impaired renal function.
*Increased PTH, increased calcium, increased phosphate*
- This pattern is highly unusual and not characteristic of any common parathyroid or kidney disorder.
- While both PTH and phosphate can be increased in certain advanced stages of CKD, calcium levels are typically low or normal, not elevated in secondary hyperparathyroidism.
Starling forces in glomerular filtration US Medical PG Question 10: Activation of the renin-angiotensin-aldosterone system yields a significant physiological effect on renal blood flow and filtration. Which of the following is most likely to occur in response to increased levels of Angiotensin-II?
- A. Decreased renal plasma flow, decreased filtration fraction
- B. Decreased renal plasma flow, increased glomerular capillary oncotic pressure
- C. Increased renal plasma flow, decreased filtration fraction
- D. Increased renal plasma flow, increased filtration fraction
- E. Decreased renal plasma flow, increased filtration fraction (Correct Answer)
Starling forces in glomerular filtration Explanation: ***Decreased renal plasma flow, increased filtration fraction***
- **Angiotensin II** causes **efferent arteriolar constriction**, which reduces blood flow leaving the glomerulus, thereby **decreasing renal plasma flow**.
- This efferent constriction also increases **glomerular hydrostatic pressure** and reduces plasma flow distal to the glomerulus, leading to a **higher filtration fraction** (GFR/RPF).
*Decreased renal plasma flow, decreased filtration fraction*
- While **renal plasma flow decreases**, a **decreased filtration fraction** would imply that either GFR decreases disproportionately more than RPF or GFR does not increase despite the RPF reduction, which is not the typical response to **angiotensin II** due to its predominant effect on the **efferent arteriole**.
*Decreased renal plasma flow, increased glomerular capillary oncotic pressure*
- **Increased glomerular capillary oncotic pressure** is a consequence of increased filtration fraction, as more fluid is filtered out, leaving behind a more concentrated plasma. This option includes a correct element (decreased RPF) but pairs it with a less direct and defining outcome of acute Angiotensin II action as the primary physiological effect.
*Increased renal plasma flow, decreased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, predominantly of the efferent arteriole, which by definition would **decrease renal plasma flow**, not increase it.
- A **decreased filtration fraction** would be inconsistent with efferent arteriolar constriction which typically raises GFR relative to RPF.
*Increased renal plasma flow, increased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, leading to a **decrease in renal plasma flow**, not an increase.
- While **filtration fraction is increased**, the initial premise of increased renal plasma flow is incorrect.
More Starling forces in glomerular filtration US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.