Renal blood flow autoregulation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Renal blood flow autoregulation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Renal blood flow autoregulation US Medical PG Question 1: A 55-year-old woman presents to a physician’s clinic for a diabetes follow-up. She recently lost weight and believes the diabetes is ‘winding down’ because the urinary frequency has slowed down compared to when her diabetes was "at its worst". She had been poorly compliant with medications, but she is now asking if she can decrease her medications as she feels like her diabetes is improving. Due to the decrease in urinary frequency, the physician is interested in interrogating her renal function. Which substance can be used to most accurately assess the glomerular filtration rate (GFR) in this patient?
- A. Para-aminohippurate (PAH)
- B. Glucose
- C. Inulin (Correct Answer)
- D. Urea
- E. Creatinine
Renal blood flow autoregulation Explanation: ***Correct Answer: Inulin***
- **Inulin** is freely filtered by the glomeruli and is neither reabsorbed nor secreted by the renal tubules, making its clearance rate an **accurate measure of GFR**.
- It is considered the **gold standard** for GFR measurement, although it is not routinely used in clinical practice due to its exogenous nature and the need for continuous infusion.
*Incorrect: Para-aminohippurate (PAH)*
- **PAH** is both filtered and actively secreted by the renal tubules, meaning its clearance reflects **renal plasma flow**, not GFR.
- Due to its high extraction fraction, it is used to measure **effective renal plasma flow (ERPF)**.
*Incorrect: Glucose*
- **Glucose** is freely filtered by the glomeruli but is almost completely reabsorbed in the proximal convoluted tubule in healthy individuals, especially at normal blood glucose levels.
- Therefore, glucose clearance is typically **zero** and does not measure GFR.
*Incorrect: Urea*
- **Urea** is filtered by the glomeruli, but a significant portion is **reabsorbed** by the renal tubules, particularly in states of lower urine flow.
- Its clearance **underestimates GFR** and varies with hydration status and protein intake, making it an unreliable sole measure of GFR.
*Incorrect: Creatinine*
- **Creatinine** is freely filtered by the glomeruli, but a small amount is also **secreted** by the renal tubules, leading to an overestimation of GFR, especially in advanced kidney disease.
- Although commonly used as an **estimate of GFR** in clinical practice due to its endogenous production, it is not as accurate as inulin.
Renal blood flow autoregulation US Medical PG Question 2: Which factor most strongly influences protein filtration at the glomerulus?
- A. Electrical charge
- B. Molecular size (Correct Answer)
- C. Shape
- D. Temperature
Renal blood flow autoregulation Explanation: ***Molecular size***
- The glomerular filtration barrier, particularly the **slit diaphragms** between podocytes, acts as a size-selective filter, restricting the passage of larger molecules.
- Proteins like **albumin** (molecular radius ~36 Å, molecular weight ~69 kDa) are significantly large, making them difficult to pass through the filtration barrier.
- Size selectivity is the **primary and most important** factor in protein filtration.
*Electrical charge*
- The glomerular basement membrane contains **negatively charged proteoglycans** (heparan sulfate), which repel negatively charged proteins like albumin, contributing to their retention.
- While important, the role of electrical charge is **secondary** to molecular size in preventing the bulk passage of most proteins.
*Shape*
- While abnormal protein shapes (e.g., **amyloid fibrils**) can impact filtration in specific disease states, the typical physiological filtration of most proteins is primarily governed by size and charge.
- The inherent shape of normal globular proteins plays a less direct role compared to their overall size.
*Temperature*
- **Physiological temperature** is relatively constant in the body and does not directly influence the molecular interactions and physical properties of the glomerular filtration barrier in a way that significantly alters protein filtration.
- Temperature changes would lead to denaturation or aggregation, which are not the primary determinants of normal protein filtration.
Renal blood flow autoregulation US Medical PG Question 3: A 64-year-old African American female comes to the physician's office for a routine check-up. The patient's past medical history is significant for hypertension, diabetes, and osteoarthritis in her right knee. Her medications include metformin, glimepiride, lisinopril, metoprolol, hydrochlorothiazide, and ibuprofen as needed. Her only complaint is an unremitting cough that started about 3 weeks ago and she has noticed some swelling around her mouth. The drug most likely responsible for her recent symptoms causes its primary renal hemodynamic effect on which part of the kidney?
- A. Collecting duct
- B. Distal convoluted tubule
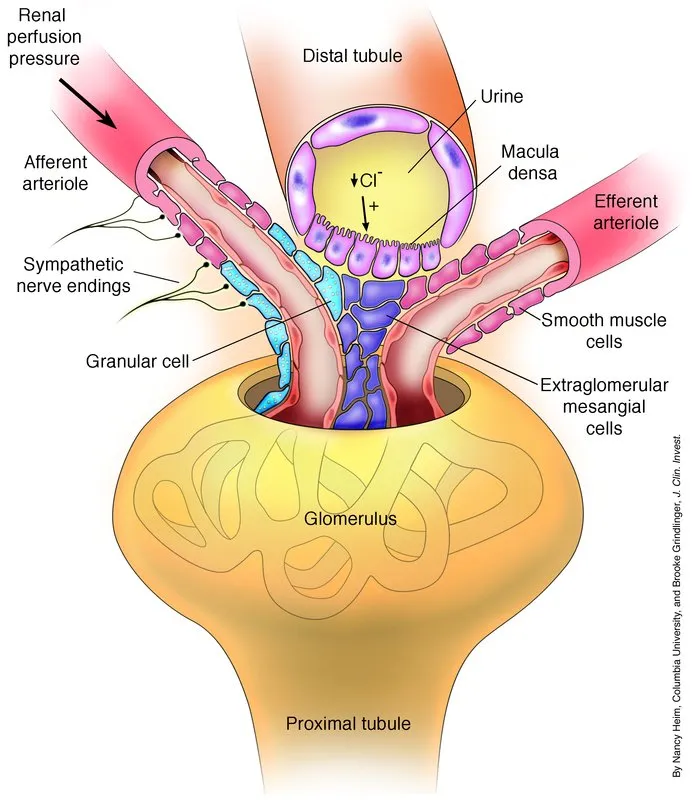
- C. Juxtaglomerular cells
- D. Efferent arteriole (Correct Answer)
- E. Afferent arteriole
Renal blood flow autoregulation Explanation: ***Efferent arteriole***
- The patient's symptoms of an **unremitting cough** and **angioedema** (swelling around her mouth) are classic side effects of **ACE inhibitors**, such as **lisinopril**.
- ACE inhibitors primarily exert their renal hemodynamic effects by **dilating the efferent arteriole**, leading to a decrease in intraglomerular pressure and glomerular filtration rate.
*Collecting duct*
- The collecting duct is the primary site of action for **vasopressin (ADH)** and **aldosterone**, regulating water and sodium reabsorption, respectively.
- While other medications like **thiazides** (used by the patient) affect distal tubules and collecting ducts indirectly, their direct impact on the collecting duct is not the cause of angioedema or cough.
*Distal convoluted tubule*
- The distal convoluted tubule is the main site of action for **thiazide diuretics** (e.g., hydrochlorothiazide), which inhibit the Na-Cl cotransporter.
- This tubule segment is not directly involved in the mechanism leading to angioedema or cough caused by ACE inhibitors.
*Juxtaglomerular cells*
- Juxtaglomerular cells are responsible for producing **renin**, which is the initial step in the **renin-angiotensin-aldosterone system (RAAS)**.
- While ACE inhibitors block the conversion of angiotensin I to angiotensin II, they do not directly act on the juxtaglomerular cells themselves to cause their side effects.
*Afferent arteriole*
- The afferent arteriole is primarily regulated by **sympathetic tone** and local factors, and is the main site of action for medications like **NSAIDs** (e.g., ibuprofen, which the patient takes as needed).
- While NSAIDs cause **afferent arteriole constriction** and can impair renal function, they do not cause angioedema or a chronic cough.
Renal blood flow autoregulation US Medical PG Question 4: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Renal blood flow autoregulation Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
Renal blood flow autoregulation US Medical PG Question 5: A 33-year-old pilot is transported to the emergency department after she was involved in a cargo plane crash during a military training exercise in South Korea. She is conscious but confused. She has no history of serious illness and takes no medications. Physical examination shows numerous lacerations and ecchymoses over the face, trunk, and upper extremities. The lower extremities are cool to the touch. There is continued bleeding despite the application of firm pressure to the sites of injury. The first physiologic response to develop in this patient was most likely which of the following?
- A. Increased respiratory rate
- B. Increased capillary refill time
- C. Decreased systolic blood pressure
- D. Decreased urine output
- E. Increased heart rate (Correct Answer)
Renal blood flow autoregulation Explanation: ***Increased heart rate***
- **Tachycardia** is often the first physiological response to **hypovolemia** (due to hemorrhage, such as that stemming from multiple lacerations). The heart attempts to compensate for reduced circulating blood volume by increasing its pumping rate.
- This sympathetic nervous system response aims to maintain **cardiac output** and tissue perfusion as **blood pressure** and **venous return** start to fall.
*Increased respiratory rate*
- An increased respiratory rate, or **tachypnea**, typically occurs later as the body attempts to compensate for decreased oxygen delivery and metabolic acidosis that can result from sustained hypoperfusion and shock.
- While significant, it usually follows the initial hemodynamic adjustments of the heart.
*Increased capillary refill time*
- **Increased capillary refill time** indicates impaired peripheral perfusion and is a sign of more significant **hypovolemic shock**, often occurring after initial compensatory mechanisms have been activated.
- This reflects **peripheral vasoconstriction**, a later compensatory mechanism, rather than the very first physiological response.
*Decreased systolic blood pressure*
- **Decreased systolic blood pressure** (hypotension) is a later sign of shock and indicates a failure of the body's compensatory mechanisms to maintain adequate blood volume and perfusion, often reflecting a loss of more than 30-40% of blood volume.
- The body initially tries to maintain blood pressure through increased heart rate and vasoconstriction before it drops.
*Decreased urine output*
- **Decreased urine output** (oliguria) is a renal compensatory mechanism in response to reduced renal perfusion and increased antidiuretic hormone (ADH) release, aiming to conserve fluid.
- This response takes time to manifest and is not typically the very first physiological change after acute blood loss.
Renal blood flow autoregulation US Medical PG Question 6: A new drug X is being tested for its effect on renal function. During the experiments, the researchers found that in patients taking substance X, the urinary concentration of sodium decreases while urine potassium concentration increase. Which of the following affects the kidneys in the same way as does substance X?
- A. Aldosterone (Correct Answer)
- B. Furosemide
- C. Spironolactone
- D. Atrial natriuretic peptide
- E. Hydrochlorothiazide
Renal blood flow autoregulation Explanation: ***Aldosterone***
- **Aldosterone** acts on the **principal cells** of the **collecting duct** to increase sodium reabsorption and potassium secretion.
- This action leads to a decrease in urinary sodium concentration and an increase in urinary potassium concentration, matching the effects of drug X.
*Furosemide*
- **Furosemide** is a **loop diuretic** that inhibits the **Na-K-2Cl cotransporter** in the **thick ascending limb** of the loop of Henle.
- This inhibition leads to increased excretion of sodium, potassium, and water, resulting in higher urinary sodium concentration.
*Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that blocks aldosterone's effects on the collecting duct.
- This leads to increased sodium excretion and decreased potassium excretion (potassium-sparing effect), which is the opposite of drug X.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** is released in response to atrial stretch and causes **natriuresis** (increased sodium excretion) and **diuresis**.
- It works by dilating afferent arterioles and constricting efferent arterioles, increasing GFR, and inhibiting sodium reabsorption, thus increasing urinary sodium concentration.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that inhibits the **Na-Cl cotransporter** in the **distal convoluted tubule**.
- This leads to increased sodium and chloride excretion but typically causes potassium wasting (hypokalemia), which differs from the increased urinary potassium concentration seen with drug X.
Renal blood flow autoregulation US Medical PG Question 7: A 70-year-old female with chronic kidney failure secondary to diabetes asks her nephrologist to educate her about the techniques used to evaluate the degree of kidney failure progression. She learns about the concept of glomerular filtration rate (GFR) and learns that it can be estimated by measuring the levels of some substances. The clearance of which of the following substances is the most accurate estimate for GFR?
- A. Paraaminohippurate (PAH)
- B. Sodium
- C. Inulin (Correct Answer)
- D. Creatinine
- E. Glucose
Renal blood flow autoregulation Explanation: ***Inulin***
- **Inulin** is freely filtered by the glomeruli and is neither reabsorbed nor secreted by the renal tubules, making its clearance the **gold standard** for accurately measuring GFR.
- Due to its ideal physiological properties, inulin clearance perfectly reflects the rate at which plasma is filtered by the kidneys.
*Paraaminohippurate (PAH)*
- **PAH** is almost completely cleared from the blood by both glomerular filtration and **tubular secretion**, making its clearance an accurate measure of **renal plasma flow (RPF)**, not GFR.
- While important for assessing renal blood flow, it does not directly reflect the filtration capacity of the glomeruli.
*Sodium*
- **Sodium** is freely filtered at the glomerulus, but a significant portion (approximately **99%**) is **reabsorbed** by the renal tubules.
- Its clearance is highly variable and depends on various physiological factors, making it unsuitable for GFR estimation.
*Creatinine*
- **Creatinine** is freely filtered by the glomeruli and is also **modestly secreted** by the renal tubules, leading to an **overestimation of GFR** at lower kidney function levels.
- Despite being the most commonly used clinical marker due to its endogenous production, its tubular secretion makes it less accurate than inulin.
*Glucose*
- **Glucose** is freely filtered by the glomeruli but is almost **completely reabsorbed** by the renal tubules under normal physiological conditions.
- Its presence in urine (glycosuria) indicates a high plasma glucose level or tubular reabsorption defects, not a measure of GFR.
Renal blood flow autoregulation US Medical PG Question 8: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Renal blood flow autoregulation Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
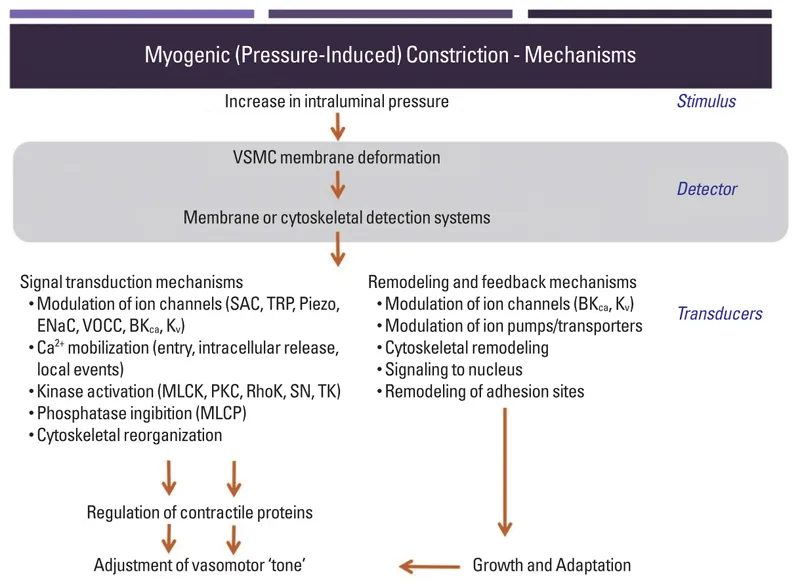
*Myogenic response*
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
Renal blood flow autoregulation US Medical PG Question 9: Which mechanism primarily regulates sodium reabsorption in the collecting duct?
- A. Glomerulotubular balance
- B. Atrial natriuretic peptide
- C. Antidiuretic hormone
- D. Aldosterone (Correct Answer)
Renal blood flow autoregulation Explanation: ***Aldosterone***
- **Aldosterone** is the primary hormone that stimulates **sodium reabsorption** and **potassium secretion** in the principal cells of the collecting duct.
- It acts by increasing the synthesis and activity of **ENaC channels** on the apical membrane and **Na+/K+-ATPase pumps** on the basolateral membrane.
*Glomerulotubular balance*
- **Glomerulotubular balance** refers to the mechanism by which the **proximal tubule** reabsorbs a constant fraction of the filtered load, regardless of changes in glomerular filtration rate (GFR).
- This mechanism maintains a relatively constant delivery of fluid and solutes to downstream segments but does not primarily regulate sodium in the collecting duct.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** primarily **inhibits sodium reabsorption** in the collecting duct, leading to **natriuresis** and **diuresis**, which is the opposite of sodium reabsorption.
- ANP is released in response to atrial stretch, indicating increased blood volume.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)** primarily regulates **water reabsorption** in the collecting duct by increasing the insertion of **aquaporin-2 channels** into the apical membrane, making the collecting duct permeable to water.
- While ADH can indirectly affect sodium concentration by influencing water movement, it does not directly regulate sodium transport to the same extent as aldosterone.
Renal blood flow autoregulation US Medical PG Question 10: A scientist is studying the excretion of a novel toxin X by the kidney in order to understand the dynamics of this new substance. He discovers that this new toxin X has a clearance that is half that of inulin in a particular patient. This patient's filtration fraction is 20% and his para-aminohippuric acid (PAH) dynamics are as follows:
Urine volume: 100 mL/min
Urine PAH concentration: 30 mg/mL
Plasma PAH concentration: 5 mg/mL
Given these findings, what is the clearance of the novel toxin X?
- A. 1,500 mL/min
- B. 600 mL/min
- C. 300 mL/min
- D. 60 mL/min (Correct Answer)
- E. 120 mL/min
Renal blood flow autoregulation Explanation: ***60 ml/min***
- First, calculate the **renal plasma flow (RPF)** using PAH clearance: RPF = (Urine PAH conc. × Urine vol.) / Plasma PAH conc. = (30 mg/mL × 100 mL/min) / 5 mg/mL = 600 mL/min.
- Next, calculate the **glomerular filtration rate (GFR)**, which is the clearance of inulin. GFR = RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min. Toxin X clearance is half of inulin clearance, so 120 mL/min / 2 = **60 mL/min**.
*1,500 ml/min*
- This value is likely obtained if an incorrect formula or conversion was made, possibly by misinterpreting the units or the relationship between GFR, RPF, and filtration fraction.
- It significantly overestimates the clearance for a substance that is cleared at half the rate of inulin.
*600 ml/min*
- This value represents the **renal plasma flow (RPF)**, calculated using the PAH clearance data.
- It does not account for the filtration fraction or the fact that toxin X clearance is half of inulin clearance (GFR).
*300 ml/min*
- This value would be obtained if the renal plasma flow (RPF) was incorrectly halved, or if an intermediate calculation was misinterpreted as the final answer.
- It does not align with the given filtration fraction and the relationship between toxin X and inulin clearance.
*120 ml/min*
- This value represents the **glomerular filtration rate (GFR)**, which is equal to the clearance of inulin (RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min).
- The question states that the clearance of toxin X is **half** that of inulin, so this is an intermediate step, not the final answer.
More Renal blood flow autoregulation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.