Filtration barrier components US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Filtration barrier components. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Filtration barrier components US Medical PG Question 1: A 12-year-old boy is found on a routine auditory screening to have mild high frequency hearing impairment. On exam, he has no ear pain, no focal neurological deficits, and no cardiac murmurs. He has not had any recent illness. Laboratory studies show:
Serum:
Creatinine: 0.7 mg/dl
Protein: 3.8 g/dl
Antistreptolysin O titer: 60 Todd units (12-166 normal range)
Urinalysis:
Microscopic heme
Protein: 4+
RBCs: 6/hpf
A kidney biopsy is taken. Which of the following findings is most characteristic of this patient’s disease?
- A. Thickened “tram-track” appearance of basement membrane on electron microscopy
- B. “Spike and dome” appearance on electron microscopy
- C. Crescent-moon shapes on light microscopy
- D. Large eosinophilic nodular lesions on light microscopy
- E. “Basket-weave” pattern of basement membrane on electron microscopy (Correct Answer)
Filtration barrier components Explanation: ***“Basket-weave” pattern of basement membrane on electron microscopy***
- The combination of **Sensorineural hearing loss**, **microscopic hematuria**, and **proteinuria** in a young boy is highly suggestive of **Alport syndrome**.
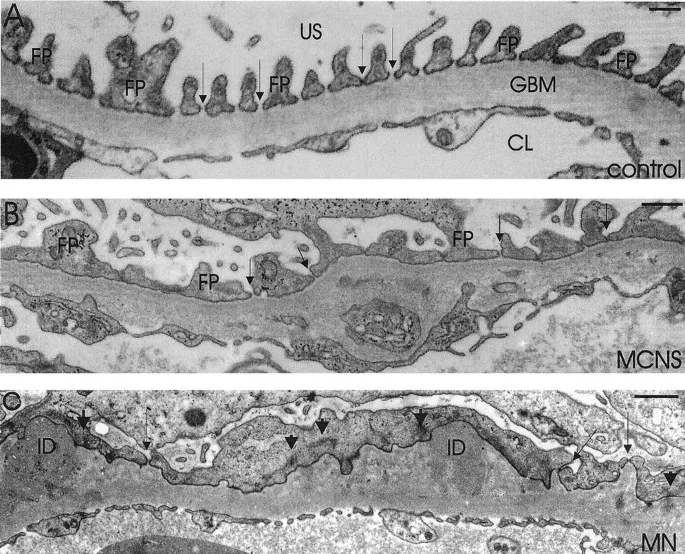
- **Alport syndrome** is characterized by mutations in genes encoding **Type IV collagen**, leading to characteristic ultrastructural changes in the glomerular basement membrane, including splitting and thinning, which gives it a **"basket-weave" appearance** on electron microscopy.
*Thickened “tram-track” appearance of basement membrane on electron microscopy*
- This finding is characteristic of **dense deposit disease** (also known as C3 glomerulopathy), where dense deposits within the glomerular basement membrane lead to a unique pattern.
- While dense deposit disease can cause hematuria and proteinuria, it is not typically associated with the high-frequency hearing loss seen in this patient.
*“Spike and dome” appearance on electron microscopy*
- This is a classic finding in **membranous nephropathy**, due to subepithelial immune deposits and new basement membrane material forming around them.
- Membranous nephropathy typically presents with **nephrotic syndrome** in adults and is not associated with hearing impairment.
*Crescent-moon shapes on light microscopy*
- **Crescent formation** is characteristic of rapidly progressive glomerulonephritis (RPGN), indicating severe glomerular injury and often associated with systemic vasculitis or anti-GBM disease.
- While RPGN can cause hematuria and proteinuria, the clinical presentation with hearing loss is not typical, and the underlying pathology is different.
*Large eosinophilic nodular lesions on light microscopy*
- This describes the **Kimmelstiel-Wilson lesions** seen in **diabetic nephropathy**, which are pathognomonic for this condition.
- Diabetic nephropathy is a complication of long-standing diabetes and is not consistent with the patient's age or clinical presentation.
Filtration barrier components US Medical PG Question 2: A 43-year-old man comes to the physician for a 1-week history of swelling around his eyes and decreased urination. His pulse is 87/min, and blood pressure is 152/95 mm Hg. Physical examination shows 1+ periorbital and pretibial edema. Serum studies show a urea nitrogen concentration of 21 mg/dL and a creatinine concentration of 1.4 mg/dL. Urinalysis shows 3+ blood and 1+ protein. Further evaluation of this patient is most likely to show which of the following?
- A. Urinary rhomboid crystals
- B. Renal interstitial inflammation
- C. Hypoalbuminemia
- D. Detached renal tubular epithelial cells
- E. Red blood cell casts (Correct Answer)
Filtration barrier components Explanation: ***Red blood cell casts***
- The patient's presentation with **periorbital and pretibial edema**, **hypertension**, elevated **creatinine**, **hematuria** (3+ blood), and mild **proteinuria** (1+ protein) is highly suggestive of **acute glomerulonephritis**.
- **Red blood cell casts** are pathognomonic for **glomerulonephritis**, indicating that red blood cells are leaking from the glomeruli and congealing in the renal tubules.
*Urinary rhomboid crystals*
- **Urinary rhomboid crystals** are typically associated with conditions like **uric acid nephrolithiasis** or gout, which are not suggested by the patient's symptoms or lab findings.
- Their presence would indicate a risk for **kidney stones**, not evidence of glomerular inflammation.
*Renal interstitial inflammation*
- **Renal interstitial inflammation** is characteristic of **acute interstitial nephritis**, which often presents with fever, rash, eosinophilia, and flank pain, usually due to drug reactions or infections.
- While kidney injury can occur, the primary findings of **hematuria** and **proteinuria** in this context strongly point away from an interstitial process as the initial diagnosis.
*Hypoalbuminemia*
- **Hypoalbuminemia** is a hallmark of **nephrotic syndrome**, characterized by severe proteinuria (>3.5 g/day), significant edema, and hyperlipidemia.
- This patient has only 1+ proteinuria, which is not severe enough to cause significant hypoalbuminemia or the full nephrotic picture.
*Detached renal tubular epithelial cells*
- **Detached renal tubular epithelial cells** and **tubular cell casts** are characteristic findings in **acute tubular necrosis (ATN)**, usually resulting from ischemia or nephrotoxins.
- While ATN can cause acute kidney injury, the prominent **hematuria** and **hypertension** in this case are more indicative of a glomerular process than tubular damage.
Filtration barrier components US Medical PG Question 3: A 45-year-old man presents with a 3-day history of right-sided flank pain due to a lodged ureteral stone. What changes would be expected to be seen at the level of glomerular filtration?
- A. Increase in glomerular capillary oncotic pressure
- B. Increase in Bowman's space oncotic pressure
- C. Increase in filtration fraction
- D. Increase in Bowman's space hydrostatic pressure (Correct Answer)
- E. No change in filtration fraction
Filtration barrier components Explanation: ***Increase in Bowman's space hydrostatic pressure***
- A lodged ureteral stone causes **obstruction** of urine flow, leading to a backup of fluid in the renal tubules and eventually into **Bowman's space**.
- This increased fluid volume in Bowman's space directly raises its **hydrostatic pressure**, which opposes glomerular filtration, thereby reducing the net filtration pressure.
*Increase in glomerular capillary oncotic pressure*
- **Glomerular capillary oncotic pressure** primarily reflects the protein concentration within the glomerular capillaries, which would not be directly increased by a ureteral stone.
- This parameter typically rises when fluid is filtered out, increasing protein concentration in the remaining blood, but not as the initial insult from obstruction.
*Increase in Bowman's space oncotic pressure*
- **Bowman's space oncotic pressure** is normally very low because the glomerular filtration barrier prevents significant protein filtration.
- An increase in this pressure would imply increased protein leakage into Bowman's space, which is not a direct consequence of a ureteral obstruction.
*Increase in filtration fraction*
- The **filtration fraction** is the ratio of glomerular filtration rate (GFR) to renal plasma flow.
- Ureteral obstruction typically **decreases GFR** due to increased Bowman's space hydrostatic pressure, which would lead to a reduction, not an increase, in the filtration fraction, assuming renal plasma flow remains stable or slightly reduced.
*No change in filtration fraction*
- Ureteral obstruction significantly impacts the forces driving glomerular filtration, primarily by increasing **Bowman's space hydrostatic pressure**.
- This change inevitably leads to a **decrease in GFR**, thus altering the filtration fraction, meaning it would not remain unchanged.
Filtration barrier components US Medical PG Question 4: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Filtration barrier components Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
Filtration barrier components US Medical PG Question 5: A scientist is studying the excretion of a novel toxin X by the kidney in order to understand the dynamics of this new substance. He discovers that this new toxin X has a clearance that is half that of inulin in a particular patient. This patient's filtration fraction is 20% and his para-aminohippuric acid (PAH) dynamics are as follows:
Urine volume: 100 mL/min
Urine PAH concentration: 30 mg/mL
Plasma PAH concentration: 5 mg/mL
Given these findings, what is the clearance of the novel toxin X?
- A. 1,500 mL/min
- B. 600 mL/min
- C. 300 mL/min
- D. 60 mL/min (Correct Answer)
- E. 120 mL/min
Filtration barrier components Explanation: ***60 ml/min***
- First, calculate the **renal plasma flow (RPF)** using PAH clearance: RPF = (Urine PAH conc. × Urine vol.) / Plasma PAH conc. = (30 mg/mL × 100 mL/min) / 5 mg/mL = 600 mL/min.
- Next, calculate the **glomerular filtration rate (GFR)**, which is the clearance of inulin. GFR = RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min. Toxin X clearance is half of inulin clearance, so 120 mL/min / 2 = **60 mL/min**.
*1,500 ml/min*
- This value is likely obtained if an incorrect formula or conversion was made, possibly by misinterpreting the units or the relationship between GFR, RPF, and filtration fraction.
- It significantly overestimates the clearance for a substance that is cleared at half the rate of inulin.
*600 ml/min*
- This value represents the **renal plasma flow (RPF)**, calculated using the PAH clearance data.
- It does not account for the filtration fraction or the fact that toxin X clearance is half of inulin clearance (GFR).
*300 ml/min*
- This value would be obtained if the renal plasma flow (RPF) was incorrectly halved, or if an intermediate calculation was misinterpreted as the final answer.
- It does not align with the given filtration fraction and the relationship between toxin X and inulin clearance.
*120 ml/min*
- This value represents the **glomerular filtration rate (GFR)**, which is equal to the clearance of inulin (RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min).
- The question states that the clearance of toxin X is **half** that of inulin, so this is an intermediate step, not the final answer.
Filtration barrier components US Medical PG Question 6: A 12-year-old boy presents to your office with facial swelling and dark urine. He has no other complaints other than a sore throat 3 weeks ago that resolved after 6 days. He is otherwise healthy, lives at home with his mother and 2 cats, has no recent history of travel, and no sick contacts. On physical examination his temperature is 99°F (37.2°C), blood pressure is 130/85 mmHg, pulse is 80/min, respirations are 19/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal examinations are unremarkable. There is mild periorbital and pedal edema. Urinalysis shows 12-15 RBC/hpf, 2-5 WBC/hpf, and 30 mg/dL protein. Which additional finding would you expect to see on urinalysis?
- A. Fatty casts
- B. RBC casts (Correct Answer)
- C. WBC casts
- D. Granular casts
- E. Hyaline casts
Filtration barrier components Explanation: ***RBC casts***
- The patient's presentation with **facial swelling**, **dark urine**, and a history of a recent **sore throat** points toward **post-streptococcal glomerulonephritis (PSGN)**.
- **RBC casts** are a hallmark microscopic finding in **glomerulonephritis**, indicating **glomerular inflammation** and bleeding.
*Fatty casts*
- **Fatty casts** are characteristic of **nephrotic syndrome**, which primarily involves heavy proteinuria and generalized edema.
- While there is some proteinuria and edema, the dark urine and history of recent infection are more consistent with nephritic syndrome.
*Hyaline casts*
- **Hyaline casts** are composed of Tamm-Horsfall proteins and can be found in healthy individuals, or in conditions like **dehydration** or **fever**.
- They are a non-specific finding and do not indicate specific renal pathology like glomerulonephritis.
*WBC casts*
- **WBC casts** are typically seen in **pyelonephritis** (kidney infection) or **interstitial nephritis**, indicating inflammation within the renal tubules.
- The patient's primary symptoms and lab findings are more consistent with glomerular disease rather than an infection of the renal parenchyma.
*Granular casts*
- **Granular casts** are formed from degenerated cellular casts or protein aggregates and are often seen in **acute tubular necrosis (ATN)** or **chronic kidney disease**.
- While they suggest renal parenchymal injury, they are not as specific for glomerulonephritis as RBC casts, especially in a subacute presentation like this.
Filtration barrier components US Medical PG Question 7: A 47-year-old man comes to the physician for a routine health maintenance examination. He states that he has felt fatigued and dizzy on several occasions over the past week. He has back pain for which he takes ibuprofen. Digital rectal examination shows no abnormalities. Laboratory studies show a hemoglobin concentration of 15 g/dL, a serum urea nitrogen concentration of 22 mg/dL, a serum creatinine concentration of 1.4 mg/dL, and a serum calcium concentration of 8.4 mg/dL. His prostate-specific antigen (PSA) level is 0.3 ng/mL (N < 4.5). An intravenous infusion of para-aminohippurate (PAH) is administered and its clearance is calculated. The patient's effective renal plasma flow is estimated to be 660 mL/min (N = 500–1350). The filtration fraction is calculated to be 9% (N = 17–23). Which of the following is the most likely cause of this patient's laboratory abnormalities?
- A. Kidney stones
- B. Multiple myeloma
- C. Bacteremia
- D. Hypovolemia
- E. NSAID use (Correct Answer)
Filtration barrier components Explanation: ***NSAID use***
- The patient's **low filtration fraction (9%)** and **slightly elevated creatinine (1.4 mg/dL)** despite a normal effective renal plasma flow (ERPF) are highly suggestive of **impaired autoregulation of GFR**.
- **NSAIDs** inhibit **prostaglandin synthesis**, which normally helps maintain GFR through **efferent arteriolar vasoconstriction**.
- Loss of prostaglandin-mediated efferent constriction leads to **efferent arteriolar vasodilation**, reducing glomerular capillary hydrostatic pressure and causing a **disproportionate fall in GFR** compared to renal plasma flow, thus decreasing the filtration fraction.
- This mechanism is particularly important in states of decreased renal perfusion where prostaglandins play a critical compensatory role.
*Kidney stones*
- While kidney stones can cause back pain, they typically lead to **obstructive nephropathy**, which would present with a decrease in both GFR and ERPF, and often with **hematuria**, none of which are specifically indicated here.
- They do not directly cause the specific pattern of a low filtration fraction with preserved ERPF described.
*Multiple myeloma*
- Multiple myeloma commonly causes **renal impairment**, often due to **light chain cast nephropathy**, leading to elevated creatinine.
- However, it typically presents with **hypercalcemia**, **anemia**, and evidence of paraproteinemia, which are not seen in this patient (normal hemoglobin, normal calcium).
*Bacteremia*
- **Bacteremia** can lead to **sepsis** and **acute kidney injury (AKI)**, often characterized by **hypotension** and a significant drop in GFR and ERPF.
- This patient's symptoms are mild (fatigue, dizziness) and his ERPF is within the normal range, making severe sepsis less likely.
*Hypovolemia*
- **Hypovolemia** causes **prerenal acute kidney injury**, characterized by reduced ERPF, GFR, and an **increased BUN/creatinine ratio** due to increased tubular reabsorption of sodium and water.
- This patient has a normal ERPF and a normal BUN/creatinine ratio, making hypovolemia less likely to be the primary cause of his specific renal abnormalities.
Filtration barrier components US Medical PG Question 8: A 9-year-old boy is brought to the physician's office by his mother because of facial swelling for the past 2 days. The mother says that her son has always been healthy and active but is becoming increasingly lethargic and now has a puffy face. Upon inquiry, the boy describes a foamy appearance of his urine, but denies having blood in the urine, urinary frequency at night, or pain during urination. He has no history of renal or urinary diseases. Physical examination is unremarkable, except for generalized swelling of the face and pitting edema on the lower limbs. Dipstick analysis reveals 4+ proteinuria. An abdominal ultrasound shows normal kidney size and morphology. A renal biopsy yields no findings under light and fluorescence microscopy; however, glomerular podocyte foot effacement is noted on electron microscopy. Which of the following changes in Starling forces occurs in this patient's condition?
- A. Decreased oncotic pressure in the Bowman's capsule
- B. Increased hydrostatic pressure in the Bowman's capsule
- C. Decreased hydrostatic pressure in the Bowman's capsule
- D. Decreased glomerular oncotic pressure (Correct Answer)
- E. Increased glomerular hydrostatic pressure
Filtration barrier components Explanation: ***Decreased glomerular oncotic pressure***
- The patient presents with **nephrotic syndrome**, characterized by severe proteinuria (4+ on dipstick), edema, and **minimal change disease** (podocyte foot effacement on electron microscopy without changes on light or fluorescence microscopy).
- In nephrotic syndrome, large amounts of plasma proteins, particularly **albumin**, are lost in the urine, leading to **hypoalbuminemia** and a significant decrease in the **oncotic pressure of the plasma** (and thus the glomerular capillaries).
*Decreased oncotic pressure in the Bowman's capsule*
- The Bowman's capsule normally has a **very low oncotic pressure** due to the almost complete absence of proteins in the filtrate.
- While theoretically a massive increase in protein filtration could increase it, the primary Starling force affected by protein loss in nephrotic syndrome is the **plasma oncotic pressure**.
*Increased hydrostatic pressure in the Bowman's capsule*
- This condition is not typically associated with nephrotic syndrome and would rather **impair filtration**.
- Increased hydrostatic pressure in the Bowman's capsule is usually seen in conditions causing **urinary tract obstruction**, which is not present here.
*Decreased hydrostatic pressure in the Bowman's capsule*
- This would tend to **increase glomerular filtration rate** by favoring filtration, which is not the primary physiological change driving edema in nephrotic syndrome.
- There is no clinical indication for such a change in this patient's presentation.
*Increased glomerular hydrostatic pressure*
- While sometimes seen in specific glomerular diseases, this is not the primary or defining Starling force change in nephrotic syndrome leading to systemic edema.
- Increased glomerular hydrostatic pressure would tend to **increase filtration**, potentially worsening proteinuria, but the fundamental issue in nephrotic syndrome is the **loss of oncotic pressure due to protein leakage**.
Filtration barrier components US Medical PG Question 9: A 70-year-old female with chronic kidney failure secondary to diabetes asks her nephrologist to educate her about the techniques used to evaluate the degree of kidney failure progression. She learns about the concept of glomerular filtration rate (GFR) and learns that it can be estimated by measuring the levels of some substances. The clearance of which of the following substances is the most accurate estimate for GFR?
- A. Paraaminohippurate (PAH)
- B. Sodium
- C. Inulin (Correct Answer)
- D. Creatinine
- E. Glucose
Filtration barrier components Explanation: ***Inulin***
- **Inulin** is freely filtered by the glomeruli and is neither reabsorbed nor secreted by the renal tubules, making its clearance the **gold standard** for accurately measuring GFR.
- Due to its ideal physiological properties, inulin clearance perfectly reflects the rate at which plasma is filtered by the kidneys.
*Paraaminohippurate (PAH)*
- **PAH** is almost completely cleared from the blood by both glomerular filtration and **tubular secretion**, making its clearance an accurate measure of **renal plasma flow (RPF)**, not GFR.
- While important for assessing renal blood flow, it does not directly reflect the filtration capacity of the glomeruli.
*Sodium*
- **Sodium** is freely filtered at the glomerulus, but a significant portion (approximately **99%**) is **reabsorbed** by the renal tubules.
- Its clearance is highly variable and depends on various physiological factors, making it unsuitable for GFR estimation.
*Creatinine*
- **Creatinine** is freely filtered by the glomeruli and is also **modestly secreted** by the renal tubules, leading to an **overestimation of GFR** at lower kidney function levels.
- Despite being the most commonly used clinical marker due to its endogenous production, its tubular secretion makes it less accurate than inulin.
*Glucose*
- **Glucose** is freely filtered by the glomeruli but is almost **completely reabsorbed** by the renal tubules under normal physiological conditions.
- Its presence in urine (glycosuria) indicates a high plasma glucose level or tubular reabsorption defects, not a measure of GFR.
Filtration barrier components US Medical PG Question 10: A 73-year-old male is brought in by ambulance after he was found to be lethargic and confused. He has not been routinely seeing a physician and is unable to recall how he came to be in the hospital. His temperature is 99°F (37°C), blood pressure is 150/95 mmHg, pulse is 75/min, and respirations are 18/min. His past medical history is significant for poorly controlled diabetes and longstanding hypertension, and he says that he has not been taking his medications recently. Labs are obtained and shown below:
Serum:
Na+: 142 mEq/L
Cl-: 105 mEq/L
K+: 5 mEq/L
HCO3-: 16 mEq/L
Urea nitrogen: 51 mg/dL
Glucose: 224 mg/dL
Creatinine: 2.6 mg/dL
Which of the following changes would most likely improve the abnormal parameter that is responsible for this patient's symptoms?
- A. Increased Bowman's space hydrostatic pressure
- B. Decreased filtration coefficient
- C. Increased Bowman's space oncotic pressure
- D. Decreased glomerular capillary hydrostatic pressure
- E. Increased glomerular capillary hydrostatic pressure (Correct Answer)
Filtration barrier components Explanation: ***Increased glomerular capillary hydrostatic pressure***
- This patient presents with **acute kidney injury (AKI)** evidenced by **elevated creatinine (2.6 mg/dL)** and **BUN (51 mg/dL)**, causing uremic symptoms of **lethargy and confusion**
- The "abnormal parameter" is the **reduced GFR** causing azotemia and uremia
- To improve AKI and restore adequate filtration, **GFR must be increased**
- **Increasing glomerular capillary hydrostatic pressure** increases the net filtration pressure: **NFP = (PGC - PBS) - (πGC - πBS)**, where PGC is the primary driving force for filtration
- In prerenal AKI (likely in this patient with poor medication compliance for hypertension), restoring adequate renal perfusion pressure is the therapeutic goal
- While chronic hyperfiltration can contribute to long-term diabetic/hypertensive nephropathy, the **acute management priority** is restoring adequate GFR to clear uremic toxins
*Decreased glomerular capillary hydrostatic pressure*
- This would **decrease the net filtration pressure**, thereby **reducing GFR**
- Lower GFR would worsen azotemia and uremic symptoms
- This is the opposite of what's needed to improve acute kidney injury
*Increased Bowman's space hydrostatic pressure*
- This **opposes filtration** by increasing back-pressure against the glomerular capillaries
- Would **decrease GFR** and worsen the AKI
- Occurs pathologically in urinary tract obstruction
*Decreased filtration coefficient*
- The filtration coefficient (Kf) represents the permeability and surface area of the glomerular capillaries
- **Decreasing Kf reduces GFR**, worsening kidney function
- This represents glomerular damage, not a therapeutic intervention
*Increased Bowman's space oncotic pressure*
- This would theoretically **increase net filtration pressure** and GFR
- However, this is **physiologically implausible** as Bowman's space normally contains minimal protein (filtrate is protein-free)
- Significant protein in Bowman's space indicates severe glomerular damage with proteinuria, not a mechanism to improve function
More Filtration barrier components US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.